Many patients undergo elective coronary angiography without preprocedural stress testing that may be suitable if performed in patients with more angina pectoris or more frequently identified obstructive coronary artery disease (CAD). Patients in the National Cardiovascular Data Registry CathPCI Registry undergoing elective coronary angiography from July 2009 to April 2013 were assessed for differences in angina (Canadian Cardiovascular Society [CCS] class) and severity of obstructive CAD in those with and without preprocedural stress testing, stratified by CAD history. Given the large sample size, differences were considered clinically meaningful if the standardized difference (SD) was >10%. Of 790,601 patients without CAD history, 36.9% did not undergo preprocedural stress testing. Compared with patients with preprocedural stress testing, patients without preprocedural stress testing were more frequently angina free (CCS class 0; 28.2% with stress test vs 38.5% without, SD = 14.8%) and had similar rates of obstructive CAD (40.1% with stress test vs 35.7% without, SD = 9.0). Of 449,579 patients with CAD history, 44.2% did not undergo preprocedural stress testing. Patients without preprocedural stress testing reported more angina (CCS class III/IV angina: 17.8% vs 13.4%; SD = 11.3%) but were not more likely to have obstructive CAD (78.7% vs 81.1%; SD = 5.8%) than patients with preprocedural stress testing. In conclusion, approximately 40% of patients undergoing elective coronary angiography did not have preprocedural risk stratification with stress testing. For these patients, the clinical decision to proceed directly to invasive evaluation was not driven primarily by severe angina and did not result in higher detection rates for obstructive CAD.
The importance of understanding current practice patterns of proceeding directly to coronary angiography without preprocedural stress testing was underscored by a recent report assessing the appropriateness of elective percutaneous coronary interventions (PCIs). In that analysis of the National Cardiovascular Data Registry (NCDR) CathPCI Registry data, 11.6% of nonacute PCIs were deemed inappropriate ; however, >1 in 5 patients with a nonacute PCI were excluded as they did not have a preprocedural noninvasive stress test. Inclusion of these patients in those analyses may have significantly altered estimates of PCI appropriateness. Although a few studies have described this population, these studies were unable to provide detailed information on patients’ symptoms or anatomic findings. To address this gap in knowledge, we compared clinical characteristics, symptom severity, and the extent of obstructive coronary artery disease (CAD) between patients undergoing elective coronary angiography with and without preprocedural stress testing. We also examined the likelihood of any obstructive CAD in patients without preprocedural stress testing, compared with patients having a high-, intermediate-, and low-risk stress test result. Because the probability of significant CAD is known to be much higher in those with previous myocardial infarctions or revascularization procedures, we stratified the population into those without and with known CAD.
Methods
CathPCI Registry is an initiative of the American College of Cardiology Foundation and the Society for Cardiovascular Angiography and Interventions. The registry consists of consecutive diagnostic coronary angiography and PCI procedures from >1,000 hospitals of the United States. Detailed information about patient demographics, clinical features, hospital information, preprocedural stress test results, angiographic findings, and in-hospital complications are abstracted by trained staff at each hospital using standardized data elements (available at http://www.ncdr.com/WebNCDR/elements.aspx ). The CathPCI Registry conducts routine audits of their data, and a recent publication of their audit revealed an overall accuracy rate of 93.1%.
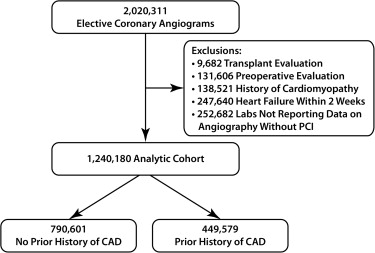
We identified 2,020,311 elective coronary angiograms performed from July 2009 to April 2013 from hospitals that reported coronary angiography data ( Figure 1 ). We included only elective coronary angiograms, as our focus was to examine the use of preprocedural stress testing in nonacute presentations, where preprocedural risk stratification is more relevant. We examined patients enrolled after July 2009 to coincide with the implementation of version 4 of the CathPCI Registry’s data collection form, which contained information on noninvasive stress testing, defined as either exercise treadmill stress test, stress echocardiogram, stress testing with single-photon emission computed tomography myocardial perfusion imaging, stress testing with cardiac magnetic resonance imaging, cardiac computed tomography coronary angiography, or coronary artery calcium score. To ensure that the study population did not have another clinical reason to proceed directly to coronary angiography without preprocedural stress testing, we excluded patients undergoing transplant evaluation (9,682 procedures), those undergoing angiography for a preoperative evaluation for noncardiac surgery (131,606 procedures), patients with a diagnosis of cardiomyopathy (138,521 procedures), patients with heart failure exacerbation within the past 2 weeks (247,640 procedures), and those admitted to hospitals that do not routinely report coronary angiography results for patients not undergoing PCI (252,682 procedures). Our final study cohort included 1,240,180 patients from 940 hospitals, of which 790,601 had no history of CAD and 449,579 had known CAD, which was defined as a history of myocardial infarction, coronary artery bypass graft surgery, or PCI.
Our primary objective was to determine whether the symptom burden, rate of obstructive CAD, and severity of obstructive CAD differed between patients who underwent elective coronary angiography with and without preprocedural stress testing. Symptom burden was assessed using the Canadian Cardiovascular Society (CCS) functional class for angina. Angina-free patients are categorized by the CathPCI Registry as CCS class 0. Consistent with recent studies for diagnostic coronary angiography, obstructive CAD was defined as a ≥50% stenosis of the left main or a major epicardial coronary artery of ≥2.0 mm in diameter. The likelihood of obstructive CAD was then defined as the proportion of patients undergoing coronary angiography with evidence of obstructive CAD. Finally, to examine differences in the extent and severity of obstructive CAD between the 2 stress test groups, we compared the distribution of 1-, 2-, and 3-vessel obstructive CAD, as well as the frequency of proximal left anterior descending (LAD) and left main CAD.
As the pretest probability for obstructive CAD is known to be higher for patients with a history of CAD, we conducted all analyses separately for patients without and with a history of known CAD. Baseline demographics and clinical characteristics were compared between patients undergoing elective coronary angiography with and without preprocedural stress testing. Because of the large sample size, which could result in statistically significant p values without clinically relevant differences in proportions, differences between groups were evaluated by computing standardized differences (differences in group means divided by the common standard deviation) for each covariate. Based on previous work, a standardized difference of >10% was used to define a clinically meaningful difference between groups.
We then examined clinically important differences in the severity of angina, the frequency of obstructive CAD, and the presence of high-risk (3-vessel, proximal LAD, or left main) CAD between patients undergoing coronary angiography with and without preprocedural stress testing. Finally, we compared the likelihood of any obstructive CAD between patients without preprocedural stress testing and those with a high-risk, intermediate-risk, and low-risk stress test result. The severity of noninvasive imaging result was defined as low, intermediate, and high risk using standardized NCDR data definitions (see Supplementary Appendix 1 ). For this last analysis, we excluded patients with preprocedural stress test whose ischemia severity was not documented (172,446 patients without CAD history and 86,770 patients with CAD history).
To ensure the robustness of our findings, we conducted a sensitivity analysis by repeating the aforementioned analyses using a more restrictive definition of obstructive CAD (a ≥50% stenosis in the left main or ≥70% stenosis in a major epicardial coronary artery of >2 mm), as this is the usual angiographic threshold for consideration of PCI. Missing data rate was <1%. All statistical analyses were performed with SAS 9.2 (SAS Institute, Inc., Cary, North Carolina) or R version 2.10.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 1,240,180 elective coronary angiograms were identified, of which 749,702 were preceded by a stress test. Stress testing with single-photon emission computed tomography myocardial perfusion imaging was the most common form of testing (78.0%), followed by stress echocardiogram (11.1%), exercise stress testing (9.3%), and stress cardiac magnetic resonance imaging (0.7%). In 790,601 patients without known CAD, coronary angiography was performed in 499,015 patients (63.1%) with preprocedural stress testing and 291,586 (36.9%) without. The mean age of this cohort was 61.9 ± 12.5 years, 51.1% of patients were men, 85.6% were of white race, and 71.2% had private health insurance. There were no differences between the 2 groups with regard to age, gender, race, insurance status, or history of diabetes mellitus ( Table 1 ). In 449,579 patients with a history of CAD, coronary angiography was performed in 250,687 (55.8%) patients with preprocedural stress testing and 198,892 (44.2%) without. The mean age of this study cohort was 66.3 ± 11.1 years, nearly 2/3 were men and had private health insurance, and 89.7% were Caucasian. Again, there were no differences between the 2 groups in demographics and other clinical variables.
| Characteristic | Patients Without CAD History | Patients With Prior CAD History | ||
|---|---|---|---|---|
| Stress Test Prior to Coronary Angiogram (n = 499,015) | No Stress Test Prior to Coronary Angiogram (n = 291,586) | Stress Test Prior to Coronary Angiogram (n = 250,687) | No Stress Test Prior to Coronary Angiogram (n = 198,892) | |
| Age (years) | 61.5 ± 11.9 | 62.6 ± 13.3 | 66.4 ± 10.7 | 66.3 ± 11.6 |
| Men | 258,889 (51.9%) | 144,915 (49.7%) | 170,876 (68.2%) | 127,888 (64.3%) |
| White | 425,555 (85.3%) | 251,182 (86.1%) | 223,549 (89.2%) | 179,673 (90.3%) |
| Private health insurance | 350,049 (72.5%) | 190,115 (68.8%) | 167,690 (68.3%) | 125,852 (65.6%) |
| No health insurance | 16,269 (3.3%) | 15,420 (5.3%) | 5,098 (2.0%) | 7,044 (3.5%) |
| Diabetes mellitus | 142,405 (28.5%) | 76,378 (26.2%) | 98,076 (39.1%) | 74,511 (37.5%) |
| On dialysis | 4,955 (1.0%) | 5,219 (1.8%) | 3,422 (1.4%) | 3,983 (2.0%) |
| Family history of premature CAD | 136,922 (27.4%) | 70,328 (24.1%) | 69,772 (27.8%) | 58,127 (29.2%) |
| Anti-anginal medications | 242,533 (48.7%) | 133,520 (45.9%) | 184,188 (73.5%) | 143,595 (72.3%) |
Of patients without a history of CAD undergoing elective coronary angiography, 32.0% reported no angina (CCS class 0) and only 12.5% reported severe angina (CCS class III or IV). Compared with patients having preprocedural stress testing, those without stress testing were more frequently angina free (38.5% for no stress test group vs 28.2% for stress test group; standardized difference of 14.8% across the CCS classes; Table 2 ). In contrast, among patients with a history of CAD undergoing elective coronary angiography, those without preceding stress tests were less likely to be angina free and more likely to have severe angina (CCS class 0: 26.1% for no stress test group vs 29.1% for stress test group and CCS class III or IV: 17.8% for no stress test group vs 13.4% for stress test group; standardized difference of 11.3% across the CCS classes). When we examined the clinical presentation of angina or angina equivalent (typical, atypical, and none), we found a similar pattern (see Table 2 ).
| Characteristic | Patients Without Prior CAD History | Patients With Prior CAD History | ||
|---|---|---|---|---|
| Stress Test Prior to Coronary Angiogram (n = 499,015) | No Stress Test Prior to Coronary Angiogram (n = 291,586) | Stress Test Prior to Coronary Angiogram (n = 250,687) | No Stress Test Prior to Coronary Angiogram (n = 198,892) | |
| Anginal classification within 2 weeks (CCS) | ||||
| 0 (Asymptomatic) | 140,193 (28.2%) | 111,782 (38.5%) ∗ | 72,668 (29.1%) | 51,647 (26.1%) ∗ |
| I | 104,835 (21.1%) | 54,910 (18.9%) ∗ | 42,331 (16.9%) | 32,953 (16.6%) ∗ |
| II | 191,401 (38.5%) | 85,977 (29.6%) ∗ | 101,415 (40.6%) | 78,371 (39.5%) ∗ |
| III | 48,240 (9.7%) | 27,232 (9.4%) ∗ | 28,386 (11.4%) | 27,670 (14.0%) ∗ |
| IV | 12,507 (2.5%) | 10,522 (3.6%) ∗ | 5,095 (2.0%) | 7,554 (3.8%) ∗ |
| CAD presentation | ||||
| Asymptomatic | 101,493 (20.4%) | 80,883 (27.8%) ∗ | 61,186 (24.4%) | 40,427 (20.4%) |
| Symptoms unlikely myocardial ischemia | 155,203 (31.1%) | 103,625 (35.6%) ∗ | 43,988 (17.6%) | 39,856 (20.1%) |
| Stable angina pectoris | 242,031 (48.5%) | 106,682 (36.6%) ∗ | 145,386 (58.0%) | 118,348 (59.6%) |
∗ Denotes clinically meaningful difference with standardized difference >10% within the cohort.
Among patients without a history of CAD undergoing elective coronary angiography, rates of 3-vessel disease were lower in patients without than in patients with preprocedural stress testing (7.6% for those without vs 9.8% for those with preprocedural stress testing; standardized difference of 10.2%; Table 3 ). However, there were no differences in rates of proximal LAD (10.9% for no stress test group vs 13.4% for stress test group; standardized difference of 7.7%) and left main CAD (2.8% for no stress test group vs 3.2% for stress test group; standardized difference of 2.4%) between the 2 groups. In patients with previous CAD, patients without preprocedural stress testing had lower rates of 3-vessel disease (27.3% for no stress test group vs 31.9% for stress test group; standardized difference of 10.7%) but similar rates of proximal LAD and left main CAD disease (see Table 3 ). These angiographic findings remained similar when we used a more restrictive definition of ≥70% stenosis for an epicardial branch coronary artery ( Table 4 ).
| Angiography | Patients Without Prior CAD History | Patients With Prior CAD History | ||
|---|---|---|---|---|
| Stress Test Prior to Coronary Angiogram (n = 499,015) | No Stress Test Prior to Coronary Angiogram (n = 291,586) | Stress Test Prior to Coronary Angiogram (n = 250,687) | No Stress Test Prior to Coronary Angiogram (n = 198,892) | |
| Any obstructive disease | 200,211 (40.1%) | 104,238 (35.7%) | 203,216 (81.1%) | 156,578 (78.7%) |
| No. of narrowed coronary arteries | ||||
| 0 | 298,804 (59.9%) | 187,348 (64.3%) ∗ | 47,471 (18.9%) | 42,314 (21.3%) ∗ |
| 1 | 93,986 (18.8%) | 52,131 (17.9%) ∗ | 61,817 (24.7%) | 54,016 (27.2%) ∗ |
| 2 | 57,152 (11.5%) | 29,853 (10.2%) ∗ | 61,323 (24.5%) | 48,308 (24.3%) ∗ |
| 3 | 49,073 (9.8%) | 22,254 (7.6%) ∗ | 80,076 (31.9%) | 54,254 (27.3%) ∗ |
| Proximal LAD narrowing | 66,786 (13.4%) | 31,687 (10.9%) | 82,551 (32.9%) | 59,885 (30.1%) |
| Left main narrowing | 15,807 (3.2%) | 8,070 (2.8%) | 27,444 (10.9%) | 19,629 (9.9%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


