Symptomatic External Carotid Artery Disease
SEAN P. RODDY, R. CLEMENT DARLING III, and KAMRAN A. JAFREE
Presentation
An 82-year-old right-handed man with hypertension, hypercholesterolemia, history of tobacco use, and coronary artery disease presents with multiple episodes of amaurosis fugax. He denied other focal symptoms and had no prior stroke. On physical examination, he had a right carotid bruit. Neurologic examination was unremarkable. A duplex study from 2 years ago demonstrated an occluded right internal carotid artery (ICA). He has no history of head or neck cancers and has never had any radiation treatments.
Differential Diagnosis
The differential diagnosis for amaurosis fugax focuses on atheroembolism from the heart to the area of brain involved. Atheroemboli primarily develop at the carotid bifurcation and usually involve the ICA origin, although an atherosclerotic plaque may reside in the aortic arch and great vessels. In the setting of an occluded ICA, emboli may be released from the ICA stump or from disease in the external carotid artery (ECA), which provides an important collateral pathway for cerebral blood flow in the presence of ICA occlusions or severe stenosis. Cardiac thrombus, especially in individuals with atrial fibrillation, valvular heart disease, or ascending aortic disease, has the potential for distal embolization, but this is not usually associated with retinal artery events.
Workup
The patient undergoes a duplex ultrasound examination of the carotid arteries, which reveals a normal right common carotid artery (CCA). The right ICA is occluded with a severe stenosis of the right ECA shown in Figure 1. The left carotid system has mild plaque in both the ECA and ICA. The vertebral arteries are patent, with antegrade flow. No evidence of aneurysmal disease is identified. Ultrasound is a quick, cost-effective, office-based procedure without radiation that helps identify the majority of extracranial carotid pathology. In this case, it not only confirms the prior occlusion of the ICA but also identifies the significant ECA stenosis that has developed. It cannot assess intracranial or intrathoracic pathology.
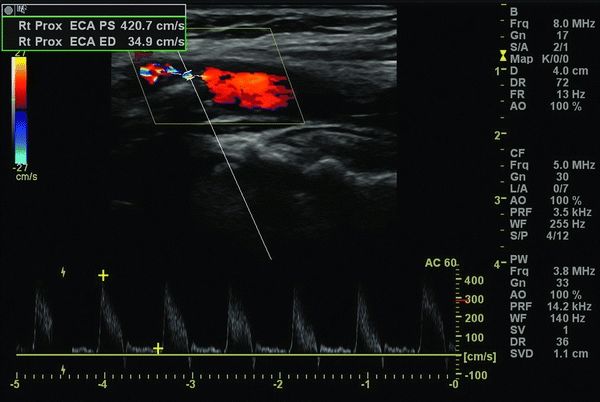
FIGURE 1 Duplex ultrasound image of the right carotid artery bifurcation demonstrating a severe stenosis in the right external carotid artery and a right internal carotid artery occlusion.

Figure 2 AP contrast arteriogram of the right common carotid artery demonstrating internal carotid artery occlusion and a stenotic, irregular external carotid artery.

Figure 3 • Straight lateral contrast arteriogram of the right carotid artery demonstrating internal carotid artery occlusion and a stenotic, irregular external carotid artery.
Cross-sectional imaging (either magnetic resonance or computed tomography [CT]) is usually the next step from the aortic arch to the intracranial vessels. In this patient, CT angiography identifies no aortic arch pathology, confirms the ICA occlusion and ECA stenosis, and rules out aneurysms, arteriovenous malformations, and intracranial hemorrhage. Alternatively, contrast arteriography of the aortic arch and great vessels may be performed with selective catheterization of the carotid arteries. Two cervical carotid selective angiographic images are listed in Figures 2 and 3 confirming the ICA occlusion and the ECA origin occlusive disease.
For completeness, the patient should undergo cardiac evaluation, including transesophageal echocardiography, for both perioperative risk assessment and source of atheroemboli. In this patient, the cardiac evaluation revealed a left ventricular ejection fraction of 50%, mild mitral regurgitation, normal ascending aorta, and no atrial or ventricular thrombus.
Diagnosis and Treatment
From these data, the most probable source of emboli is the stenotic ECA. The proximal ICA stump was occluded on duplex evaluation 2 years ago and is therefore less likely the etiology. If the ICA was previously patent, acute ICA occlusion and distal ICA thromboembolism could be a source for amaurosis fugax. The ascending aorta and proximal great vessels do not have a significant atherosclerotic plaque burden as an alternate etiology. Recommendation was made for ICA ligation and ECA endarterectomy with patch closure.
Surgical Approach
Open surgical reconstruction remains the gold standard for this pathology. The patient is placed supine under regional or general anesthesia based on surgeon preference. The carotid artery is exposed through a longitudinal neck incision. Systemic anticoagulation is achieved typically with intravenous heparin. The ICA is suture ligated. A CCA and ECA endarterectomy is performed. Prosthetic, vein, or endarterectomized ICA is typically used for patch closure.
A newer alternative recently described by Naylor et al. and Kouvelos et al. involves an endovascular approach with carotid artery stenting using bare metal stents with and without embolic protection versus ICA stump exclusion using a stentgraft that covers the ICA origin and extends into the ECA. Tapering from the CCA to the ECA is an obvious concern when using one of the current commercially available nontapered stentgrafts. Validation of this technique by others is required.
Special Intraoperative Considerations
For standard carotid endarterectomy (CEA), care should be taken to avoid the vagus and hypoglossal nerves. The surgeon must protect and separate the vagus nerve from the carotid artery so it is not caught when the vascular clamps are applied. The hypoglossal nerve traverses the superior aspect of the dissection field and can be avoided by transection of the artery and vein to the sternocleidomastoid muscle that tethers it. When ICA ligation and a CCA/ECA endarterectomy are performed, the ECA at the distal end point is skeletonized to a more significant degree than during standard CEA. The superior laryngeal nerve passes posterior to the ECA prior to entering the larynx. Dissection of the ECA and its branches distal to the atherosclerotic plaque should be performed as close as possible to the vessel wall to ensure that the nerve is separated from the adventitia.
Shunting may be performed routinely or on demand in the course of standard CEA. During ICA ligation and ECA/CCA endarterectomy, the same concerns apply though the incidence of shunt use in several series is minimal.
Patients receive systemic anticoagulation to prevent thromboembolic events during CEA. Hemostasis at the completion of the procedure is therefore critical.
Postoperative Management
Given an arterial anastomosis and use of anticoagulation with CEA, patients must be observed for hemorrhage or hematoma formation that may even compress the airway requiring operative exploration. Alternatively, thromboembolic events may lead to transient ischemic attack or stroke that also may require operative exploration and arterial reconstruction.
Elevated blood pressure occurs in over 20% of normotensive patients after CEA. Poor control of blood pressure in the postoperative period increases the risk of developing cerebral hyperperfusion syndrome. Cardiac monitoring is paramount given the rate of myocardial infarction that approaches 5% in some series (Table 1).
TABLE 1. External Carotid Artery Endarterectomy