Symptomatic Carotid Endarterectomy—Carotid Artery Stenting
DUSTIN Y. YOON and MARK K. ESKANDARI
Presentation
A 65-year-old right-handed gentleman with a history of tobacco use, myocardial infarction status post coronary bypass, and left carotid endarterectomy (CEA) 5 years ago now presents with crescendo transient ischemic attacks (TIAs). The patient states that these episodes started 2 months ago and occur several times per week. Each episode lasts 20 to 30 minutes and is associated with mild right arm weakness and blurry vision on the left side. No loss of consciousness occurs. On neurologic examination, the patient is grossly intact with mild right pronator drift. Ultrasound reveals peak systolic velocities of 380 cm/s in the left proximal internal carotid artery (ICA), and magnetic resonance angiography (MRA) of the head/neck shows two focal high-grade stenoses of 90% in this same region (Fig. 1). He remains compliant with aspirin and clopidogrel since his initial CEA.
Differential Diagnosis
The incidence of recurrent carotid stenosis is variable and depends on the definition of restenosis, method of diagnosis, and interval follow-up, with an estimated range of 8% to 19%, of which only 3% are symptomatic. Identification and management of restenosis is primarily dictated by two factors: (1) length of time from index procedure to diagnosis of restenosis and (2) the presence/absence of clinical symptoms.
A stenosis identified within the immediate post-operative period is often residual disease after an incomplete CEA rather than recurrent stenosis. Restenosis within the first 36 months is often a result of neointimal hyperplasia and is generally a smooth and homogenous lesion that is less prone to embolization. Restenosis after this 36-month post-operative period is generally a result of progressive or new atherosclerotic disease and has been associated with risk factors that include age less than 60 years, female sex, smoking, diabetes, and hypertension. Surgical management of post-CEA restenosis should be individualized and generally reserved for asymptomatic patients with greater than 80% or symptomatic patients with ≥50% lesions. However, consensus guidelines have yet to be made.
Though unlikely in this patient, differential diagnoses include new-onset atrial fibrillation (or other sources of thromboembolic disease), vasculitis, fibromuscular dysplasia (FMD), carotid dissection/aneurysm, extensive intracranial carotid disease, and migraine headaches.
Workup
The most robust assessment and follow-up data for recurrent carotid stenosis are provided by the Asymptomatic Carotid Atherosclerosis Study (ACAS) and are surveyed by noninvasive duplex ultrasonography. Color duplex ultrasound remains the preferred first-line imaging modality for evaluation although the recommended frequency of surveillance remains controversial. With the advent of contrast-enhanced MRA and now multidetector computed tomographic angiography (CTA), the anatomy of the aortic arch and circle of Willis can be assessed for carotid artery stenting (CAS) suitability. Furthermore, CTA can enhance the identification of calcification, vessel tortuosity, and any cerebral abnormalities, all of which are important for preoperative planning and post-operative monitoring. Prior to surgery, appropriate preoperative risk stratification with concomitant medical optimization with aspirin, clopidogrel, and statins should be performed.
In this patient, Figure 1 shows two focal high-grade lesions of the left ICA.

Figure 1 MRA of the head/neck shows two high-grade focal lesions at the proximal left ICA and at the level of C1.
Diagnosis and Treatment—Redo CEA or Stent?
Substantial controversy exists regarding the natural history, histopathologic significance, and threshold for intervention of post-CEA restenosis as well as the appropriate method of treatment. Although patient care should be individualized, most vascular surgeons would generally accept that symptomatic patients with ≥50% lesions should be treated. Generally, CAS has been recommended to high-risk patients with prior neck external beam irradiation, prior neck dissections/tracheostomies, inaccessible lesions unamenable to CEA (above the C2 level), and those with limited cervical spine mobility. While many centers show high patency rates in the immediate post-CEA CAS period, the long-term durability is inconclusive. Nevertheless, CAS has been continuously justified for its minimally invasive approach, the histopathologic nature of neointimal hyperplastic lesions more amenable to dilation, and the low risk for cranial nerve injury, with some studies showing up to 18% risk of nerve injury with redo CEA.
Several meta-analyses have been performed comparing the complication rates of redo CEA versus CAS in this post-CEA population. While the results are widely variable, there are trends toward lower perioperative cardiac complications, lower rate of procedure-related stroke, and lower cranial nerve injuries with CAS. These trends, however, are difficult to tease out with respect to early versus late restenosis, and some data show the highest risk of periprocedural stroke/death with CAS within 7 days of symptoms. Most studies show no difference in mortality between the two treatment groups.
This patient, who has high preoperative risk factors and late restenosis, opted to enroll in the high-risk Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy World Wide (SAPPHIRE WW) trial and undergo CAS.
Surgical Approach
Approximately 50% of all patients undergoing CEA have clinically relevant coronary artery disease, and myocardial death is the most common cause of mortality in these patients. While the North American Symptomatic Carotid Endarterectomy Trial (NASCET) excluded patients with recent unstable angina and myocardial infarction, they showed high cardiovascular complication rates. The initial results of the randomized SAPPHIRE trial comparing CEA with CAS in patients with high risk for open surgery showed that CAS was noninferior in comparison to CEA and had trends toward lower complication rates. Enrollment and results are still ongoing in the high-risk registry, but, in general, most vascular surgeons would agree that high-risk, symptomatic patients with contraindications or challenging redo CEA should undergo CAS.
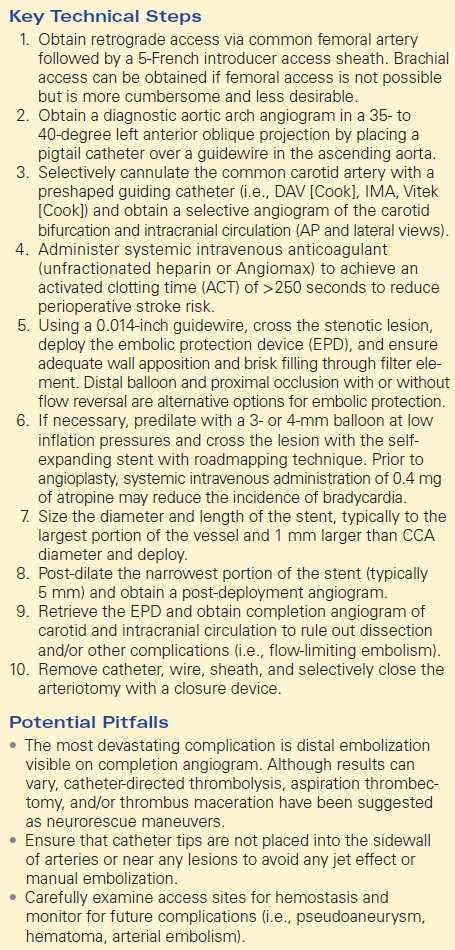
Unless contraindicated, all patients should be on dual antiplatelet regimen of aspirin and clopidogrel preoperatively. Preprocedural imaging with MRA or CTA should be obtained to carefully evaluate aortic arch morphology and origin and abnormalities of supra-aortic vessels (i.e., tortuosity, calcification, severe angulation), and to take accurate measurements of the lesion and carotid arteries (Table 1).
TABLE 1. Symptomatic Carotid Endartectomy- Carotid Artery Stenting