Syme and Lisfranc Disarticulations
Christopher P. Chiodo
Jeremy T. Smith
Syme Amputation
Initially described by Syme in the 19th century, the amputation that still bears his name consists of disarticulation through the tibiotalar joint with resection of the malleoli and preservation of the plantar heel pad. This procedure may be performed in patients with adequate distal tibial bone stock and an uncompromised soft tissue envelope. The main advantages of a Syme amputation are the creation of an end-bearing residual limb with preservation of the heel pad and only a few centimeters of lost leg length. As such, some limited ambulation may be possible without a prosthesis. The main disadvantage is the increased challenge with prosthetic fitting and inability to incorporate a hinge in the prosthesis. Additionally, adequately securing the heel pad to the residual distal tibia can be a challenge.
Indications
Unsalvageable infection, necrosis, trauma, or deformity of the foot with a viable heel pad
Elderly or minimally ambulatory patients for whom prosthetic donning may be difficult
Contraindications
Insufficient heel pad
Young, healthy individuals in whom a more functional, hinged below-knee prosthesis is desired
With gross infection, strong consideration should be given to performing the procedure in a staged fashion. At the index procedure, the ankle is disarticulated and the wound left open. Intravenous antibiotics are initiated. Serial debridements are performed if
necessary, along with the use of subatmospheric pressure wound therapy. Once the soft tissues have improved, a delayed primary wound closure is performed.
necessary, along with the use of subatmospheric pressure wound therapy. Once the soft tissues have improved, a delayed primary wound closure is performed.
 Figure 25.1 Planned skin incisions with apices just distal and inferior to the tips of the malleoli. |
An infectious disease specialist should be consulted in the setting of infection. Additionally, a vascular surgeon should be consulted if there is concern for inadequate perfusion. If necessary, perfusion should be optimized preoperatively. In emergent cases this may necessitate a staged procedure.
With the patient in the supine position, two points are marked approximately 1 cm anterior and distal to the tips of the medial and lateral malleoli. Elliptical “fish-mouth” skin incisions are then created connecting these points anteriorly and inferiorly (Fig. 25.1). These correspond with the anterior and inferior skin flaps.
After incising the skin, the subcutaneous tissues are divided with a combination of blunt and sharp dissection. Dissection begins anteriorly. The deep fascia and joint capsule are preserved when possible to facilitate a layered closure at the end of the case. The extensor tendons are identified and transected. Transecting these structures under gentle traction allows them to retract proximal to the incision. To this end, peripheral nerves should be buried proximally in healthy soft tissues away from the incision, especially in nonneuropathic patients. The anterior tibial artery is ligated.
Next, the inferior flap is created. The incision is extended in a vertical fashion inferiorly, anterior to the heel pad. The peroneal tendons laterally and the flexor tendons medially are transected. Next, a bone hook is placed on the talar dome and used to pull the talus and foot anteriorly as an elevator is used to dissect the Achilles tendon and heel pad from the calcaneus (Fig. 25.2). The skin over the calcaneal tuberosity is thin and care must be taken to avoid inadvertently creating buttonholes with dissection in this region. The posterior tibial artery is transected and ligated distally while the tibial nerve is transected proximally.
Once the disarticulation is complete, the malleoli are beveled with a saw so as to improve the contour of the residual limb (Fig. 25.3).
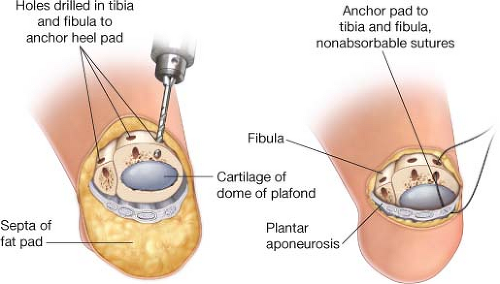
If used, the tourniquet is let down and hemostasis confirmed. Attention is then turned to closure. A deep drain is left in place if the wound bed is not dry. The heel pad is then positioned inferior to the distal tibia. The stability of the heel pad is critical to the success of this operation. Various techniques to stabilize the heel pad have been described. We use several nonabsorbable sutures secured to the anterior distal tibia passed through osseous tunnels made with a small drill bit or Kirschner wire (Fig. 25.4).
Smith et al. advocated tenodesis of the Achilles tendon to the posterior tibia in order to prevent heel pad migration. Alternatively, the lateral plantar fascia can be secured to the calcaneus with suture anchors if there is concern for varus heel pad migration.
Smith et al. advocated tenodesis of the Achilles tendon to the posterior tibia in order to prevent heel pad migration. Alternatively, the lateral plantar fascia can be secured to the calcaneus with suture anchors if there is concern for varus heel pad migration.
 Figure 25.2 The use of a bone hook with anterior translation of the talus and foot facilitates dissection of the inferior flap. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree