Although TA can occur in boys and men, it is uncommon, with several series reporting an 80% or greater prevalence of female patients. The clinical course of TA may include a prodromal prepulseless phase, which is manifested by a variety of constitutional symptoms including pyrexia, weight loss, anorexia, night sweats, malaise, arthralgias, and myalgias. Because these symptoms are nonspecific and protean, they are often not recognized as indicating an acute arteritis. Unlike the large studies reported from Japan and Mexico, patients evaluated at the authors’ institution rarely manifest the constitutional symptoms of an acute arteritis. Rather, patients usually sought medical attention for the secondary complications of arterial insufficiency or aneurysm formation. The clinical picture in this setting is one of a burned-out arteritis with a progressive deterioration in overall well-being that climaxes in a life- or limb-threatening event.
Among 40 patients treated between 1980 and 2009 at the authors’ institution, 20 presented with hypertension, nine with renal dysfunction, six with extremity ischemia, and five with cerebrovascular insufficiency as the primary indication for surgery. The most impressive constellation of symptoms has been severe systemic hypertension associated with kidney failure or varying degrees of heart failure. Among the 20 hypertensive patients, overt heart failure affected two patients and dialysis-dependent kidney failure occurred in three patients. This preponderance of hypertension is quite similar to recent reports from many Asian countries.
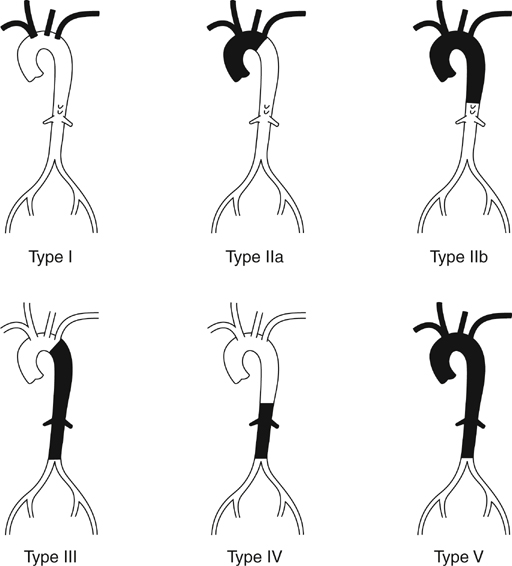
The anatomic distribution of disease is most commonly classified using the 1994 Tokyo International Conference Classification of TA, which is based on the findings of the initial aortogram (Figure 1). Among the authors’ patients, the majority presented with type V, combined aortic arch, thoracic, and abdominal aortic disease. In this experience, patients with pulmonary artery involvement have been rare, although Seoul and Mexico City authors have reported pulmonary involvement in 27% and 50% of TA patients, respectively.
Historically, all patients with suspected TA underwent conventional catheter-based abdominal and thoracic angiography. Angiography is useful in detecting luminal abnormalities, with the most common finding being tubular, long-segment stenoses or occlusions usually involving the origins of major aortic branches, aortic arch, distal descending thoracic aorta, and suprarenal abdominal aorta. Evaluation of the thoracoabdominal aorta often documents renovascular occlusive disease or a thoracoabdominal aortic coarctation. In addition to the standard anteroposterior views, lateral and oblique views of the renal and mesenteric vessels are essential for patients with a thoracoabdominal aortic coarctation. Documentation of intra arterial blood pressures above and below a stenosis is useful in planning the operative strategy.
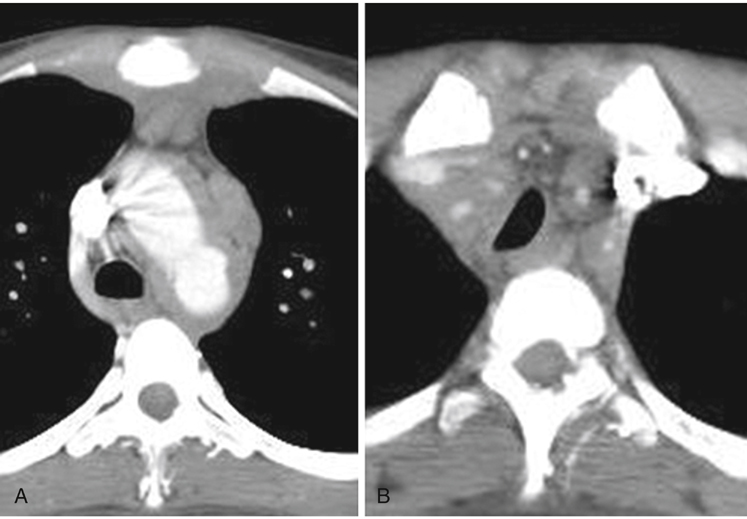
Over the last several years, computed tomography angiography (CTA) has evolved to become the mainstay of imaging in patients with suspected TA. CTA has the advantage of being able to evaluate vessel wall thickening along with luminal narrowing (Figure 2). This information is helpful in the staging of the disease as well as in developing operative strategies for revascularization. In one series, up to 61% of patients evaluated had CTA demonstrations of mural changes that identified a wider distribution of disease than that assessed by luminal changes alone.
Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) can also be used to evaluate patients with TA. MRI and MRA have the advantage of providing multiplanar section images without using ionizing radiation. Vessel wall edema and mural contrast enhancement are early signs of inflammation. However, vessel wall edema can also be a nonspecific finding, identified commonly in patients who are considered to be in clinical remission. In addition, MRA also has a tendency to overestimate the degree of stenotic disease.
Although an elevated erythrocyte sedimentation rate (ESR) is helpful in establishing a diagnosis, it is a poor indicator of disease activity. Despite an elevated ESR in most patients with TA, very few have findings consistent with an acute arteritis in arterial specimens obtained at the time of surgery. Little difference exists in the clinical course of patients with an elevated ESR as compared with those whose ESR is normal. Other acute-phase proteins identified as potential indicators of active TA disease include serum amyloid A and complement C4-binding protein.
Other diagnostic tests should be tailored to specific organ system dysfunction. In patients with renovascular hypertension or kidney failure, kidney perfusion and function are assessed by isotopic renography. Renal color-flow duplex imaging is used to assess renal parenchymal size, cortical thickness, vascular resistance, and blood flow velocity. Severe cardiac dysfunction is assessed by echocardiography because both mitral and aortic valvular insufficiency can occur in TA patients. Cardiac catheterization is indicated if significant valvular dysfunction is documented or there is suspicion of coronary or pulmonary artery involvement. Right-sided heart failure, dyspnea, or hypoxemia should raise a suspicion of pulmonary artery involvement. Cerebrovascular symptoms are evaluated with CTA or MRI/MRA. Information concerning the hemodynamics of the cerebral circulation can be provided by carotid duplex and transcranial Doppler studies.