CHAPTER 44 Surgical Treatment of Hyperhidrosis
Hyperhidrosis is commonly defined as sweating in excess of physiologic requirements. Perhaps the earliest recognition of this disorder was by Charles Dickens, whose portrayal of Uriah Heep in David Copperfield describes accurately the clinical presentation of palmar hyperhidrosis.1,2 “I saw Uriah Heep shutting up the office, and, feeling friendly towards everybody, went in and spoke to him, and at parting, gave him my hand. But oh, what a clammy hand this was! As ghostly to the touch as to the sight! I rubbed mine afterwards, to warm it, and to rub his off.”
The earliest sympathectomy undertaken specifically for treatment of hyperhidrosis was performed in Europe by Kotzareff in 1920.3 The first sympathectomy for treatment of hyperhidrosis in the United States was accomplished in 1932 by Adson and colleagues.4 The earliest thoracoscopic sympathectomy was performed in 1939 for treatment of hypertension.5 The first thoracoscopic sympathectomy for treatment of hyperhidrosis was reported in 1978.6 Paravertebral, supraclavicular, transaxillary, and transthoracic approaches have also been used to gain access to the sympathetic chain. Significant interest and large volumes of cases did not occur, however, until the availability of video-assisted thoracic surgery.
CLINICAL PRESENTATION
Sweating is intermittent and occurs at times of both apparent calm and obvious stress.7 Sweating is usually worse during the summer months. Although the degree of hyperhidrosis varies, sweating is much greater than the dampness associated with stress. A dry hand may become soaking wet within minutes. Perspiration forms on the volar surface of the fingers and on the thenar and hypothenar eminences, and it fills the palmar skin folds (Fig. 44-1). Sweat may actually run down the arm and drip to the floor.
Nearly all patients with palmar hyperhidrosis also suffer from plantar hyperhidrosis, the degree and timing of which parallels that manifested in the hands. Patients walking barefoot leave tracks as if they were walking out of the shower. Footwear is ruined by the constant moistness. Open-toe sandals are impossible to wear because the wet feet slip. Despite the frequent moistness, fungal infections are rare. As many as 50% of patients with palmar and plantar hyperhidrosis also suffer from concomitant axillary hyperhidrosis that causes garment staining and odor (bromhidrosis).1,6,8–13 Isolated axillary hyperhidrosis is a frequent complaint. Severe facial sweating is much less common.
The diagnosis of hyperhidrosis is based on patient history and physical examination. One expert multispecialty working group defined hyperhidrosis as focal sweating of greater than 6 months’ duration that fulfills at least two of the following criteria: it is bilateral and symmetric, it impairs daily activities, it occurs at least weekly, the age of onset is less than 25 years, there is a family history, and focal sweating ceases during sleep.14 There are currently no accepted objective definitions of palmar hyperhidrosis, but some have suggested that focal axillary sweat production of greater than 50 to 100 mg/5 min is diagnostic of axillary hyperhidrosis.14
EPIDEMIOLOGY
The prevalence of palmar and plantar hyperhidrosis was estimated as 0.6% to 1%1 in a study of Israeli army recruits. Based on a survey of 13,000 college and high school students, investigators from Asia reported a prevalence of 4.6%.12 A recent survey of 150,000 U.S. households yielded a hyperhidrosis prevalence of 2.8%.11 Generalized hyperhidrosis may be associated with thyrotoxicosis, neurologic diseases, and rare inherited disorders. Patients with classic palmar, plantar, and axillary hyperhidrosis do not have concomitant illnesses.
A familial history of hyperhidrosis has been obtained in as many as 65% of patients who have undergone thoracoscopic sympathectomy.1,10,12,15 Detailed kindred information provided by 49 affected individuals has led to the conclusion that the disease allele is actually present in 5% of the population, and that having one or two copies of the allele results in hyperhidrosis in 25% of carriers.15 Investigators have localized hyperhidrosis associated genes to chromosomes 1416 and 5.17
AUTONOMIC NERVOUS SYSTEM: ANATOMY AND FUNCTION
The autonomic nervous system is responsible for thermoregulation. Although both the sympathetic and parasympathetic components may contribute to sweating, the sympathetic nervous system primarily controls extremity sweating. Impulses originating in the hypothalamus reach preganglionic fibers located in the lateral horn of the ventral root of the spinal column.18 These myelinated fibers exit the ventral root and travel a brief distance through the spinal nerve before exiting as the white rami communicantes to join the paravertebral ganglia of the sympathetic chain. The nerve may immediately establish a synapse with an unmyelinated postganglionic fiber, which returns to the spinal nerve as the gray ramus communicantes, or it may ascend a variable distance within the sympathetic chain before synapsing with a postganglionic fiber. The postganglionic nerve often travels a great distance before arriving at its target organ.
The preganglionic sympathetic fibers responsible for sudomotor (sweating) activity in the hand are thought to arise from spinal segments T3 to T6. They converge on the T2 and T3 ganglia, where postganglionic fibers ascend to reach the hand via connections of the stellate ganglia to the brachial plexus.19 The precise spinal levels responsible for palmar sweating have not been defined, but T2 has been thought to be the common pathway. Release of acetylcholine from the postganglionic neurons stimulates the eccrine sweat glands.
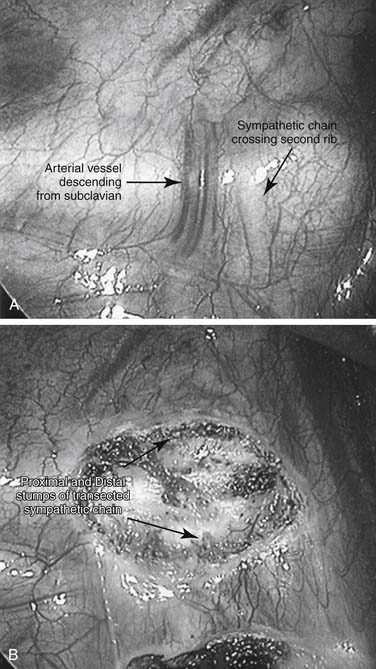
The sympathetic chain descends vertically in the thorax over the rib heads (Fig. 44-2), and rarely it is found between the medial border of the rib head and the longus colli muscle.20,21 The sympathetic ganglia are located approximately 2 mm cranial to the midportion of the underlying vertebral body.22 For example, the T2 ganglion is located between the heads of the second and third ribs. In addition to the orderly arrangement of the sympathetic nerves, Kuntz identified inconstant sympathetic branches from the second intercostal nerve to the first intercostal nerve (and hence brachial plexus) that bypassed the stellate ganglia.23 The physiologic function of these nerves is unclear.
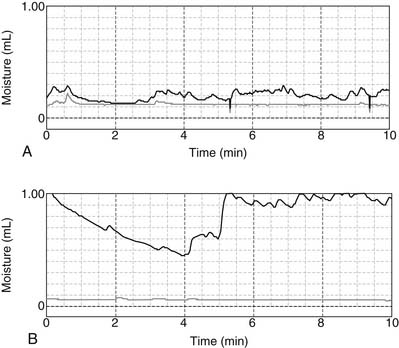
Whether hyperhidrosis represents focal dysfunction of the autonomic nervous system or is emblematic of a more global abnormality remains unknown. Resting palmar sweat production at room temperature is twice normal (Fig. 44-3).24 The sudomotor skin response is enhanced as a result of shortened nerve recovery time.25 Abnormal sensory processing is suggested by a decrease in spatial discrimination thresholds that did not improve under conditions of sensory deprivation.26 These findings (i.e., the absence of plastic cortical somatocellular changes) suggest a lack of inhibition of the hypothalamus. Palmar sweat production in response to stress is greatly increased (see Fig. 44-3). When compared with the responses in unaffected controls, pulmonary function and resting cardiac function in the supine position are normal.27–30 Circulating plasma catecholamine levels are within normal limits.31 However, peak exercise heart rate and resting heart rate in the standing position are increased.27,28 Other investigators have suggested that concomitant abnormalities of the parasympathetic system contribute to hyperhidrosis.32,33
TREATMENT
Nonoperative
Iontophoresis—placement of the hands or feet in a tap water solution through which an electric current flows—is another treatment that has been used for hyperhidrosis. The precise mechanism responsible for the elimination of sweat production is unknown. A battery-operated device is commercially available (Drionic). Control of palmar hyperhidrosis was reported in 82% of 112 patients who underwent eight daily 15-minute treatments.34 The mean remission time was 35 days. Tingling, erythema, and vesicle formation were undesirable side effects.
The neurotoxin botulinum toxin A (Botox) stops sweat production by blocking the release of acetylcholine from the postganglionic nerve end. A randomized trial has demonstrated efficacy of this treatment for axillary hyperhidrosis.35 Other investigators have reported success for palmar hyperhidrosis using 20 to 30 intradermal injections.36–38 Median duration of sweat control varies between 6 and 9 months. Weakness of the intrinsic muscle of the hand, manifested by a decrease in the thumb–index finger pinch strength, has been reported in 25% to 60% of patients.
Oral anticholinergic medications such as glycopyrrolate and oxybutynin have been employed to block the stimulation of the sweat gland caused by the release of acetylcholine from the postganglionic sympathetic nerve fiber. One published report claimed a response of 79% in patients treated with glycopyrrolate.39 Dry mouth, blurry vision, and constipation are common side effects.
Surgical
The goal of surgery is to interdict the sympathetic nerve innervation to the hand, axilla, or face. Disruption of the sympathetic chain can be accomplished by transection, by resection of ganglia, or by application of clips. The thoracic level at which interruption is necessary to achieve the desired anhidrosis while simultaneously minimizing systemic side effects is not precisely known and remains controversial. Interpretation of the voluminous literature is complicated by a plethora of inconsistent terms used to describe the operative procedures. For example, sympathectomy has been employed to describe both transection of the sympathetic chain and actual removal or ablation of the ganglion. The following recently proposed definitions seem reasonable40:
Traditionally, palmar hyperhidrosis has been treated by transecting the sympathetic chain over the second and third ribs. If concomitant axillary hyperhidrosis was present, the sympathetic chain was also transected over the fourth rib. In the absence of palmar hyperhidrosis, axillary sweating was treated by transecting the sympathetic chain over the third and fourth ribs. Some authors believe that palmar hyperhidrosis can be effectively treated by limiting the transection to the level of the third rib.41 Others have demonstrated equivalent results by transecting or clipping the sympathetic chain at T3-4.10,42 Yet other surgeons have reported success with T4-5 sympathicotomy.43
Four phase III trials have been performed, three comparing different levels for palmar hyperhidrosis and one for isolated axillary hyperhidrosis. Sixty patients with palmar hyperhidrosis were randomized to either T2-3 or T3-4 sympathicotomy.44 The single patient who did not experience complete resolution of symptoms was in the T3-4 group. However, the patients in the T3-4 group reported less severe compensatory sweating. In a second study, 232 patients were randomized to either T3 sympathicotomy or T2-to-T4 sympathicotomy.41 All patients had resolution of symptoms, but patients in the T3 cohort had fewer instances of severe compensatory sweating and were more likely to be satisfied with the results of surgery. Finally, 25 patients underwent unilateral ablation of the T2 ganglion and contralateral ablation of the T2-3 ganglia.45 The procedures were equally effective. Compensatory sweating was mild and did not differ between the two sides. Sixty-two patients with isolated axillary hyperhidrosis were randomly assigned to either T3-4 or T4 sympathectomy.46 All patients reported resolution of symptoms. However, the T4 cohort had a lower incidence of compensatory sweating (57% versus 91%).
Regardless of the surgical technique, correct identification of the anatomic level is crucial. The second rib is generally the most proximal rib that can be seen in the thorax and can be reliably identified by a vertical, descending arterial branch that crosses the rib 1 cm lateral to the sympathetic chain.47 This arterial branch originates from the subclavian artery and forms the second intercostal artery (Fig. 44-4A). The first intercostal space is covered by a fat pad, and the first rib is generally not visible from within the thorax. Additional landmarks are the azygos vein, which lies at the level of the fifth interspace, and the aortic arch, which reaches to the fourth interspace. The rib number can be determined with certainty by obtaining an intraoperative radiograph after a metallic marker has been introduced into the chest and placed over a rib.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree