Chapter 19 Surgical Reconstruction of the Supra-Aortic Trunks and Vertebral Arteries
The incidence of atherosclerotic disease is lower in the SATs than in the internal carotid and vertebral arteries. Nevertheless, the extensive study of extracranial arterial disease reported in 1968 by Hass and colleagues1 showed that one third of patients undergoing arteriography had a severe lesion involving one or more of the SATs. The morphology of atherosclerotic lesions of the SATs is not defined as well as that of the plaques found in the internal carotid artery, partly because for several years the SATs were not routinely visualized during arteriography of the cerebral vessels. In addition, the SATs are difficult to image with ultrasound techniques, which provides valuable morphologic information in the carotid bifurcation. Because there is limited knowledge of the natural history of these lesions, surgical indications are based partly on inferences. In addition, SAT lesions are often found in individuals who already have concomitant disease of the carotid or vertebral arteries—a situation that confuses the identification of the offending lesion. Stenosing lesions of the SATs usually appear at their origin from the aortic arch and often involve more than one artery. Plaques located in the ostia of the SATs are usually continuous with atheroma that extends over the dome of the aortic arch.
Symptoms of Occlusive Disease of the Supra-Aortic Trunks
Obliteration of the SATs is suggested by absent pulses in the neck (subclavian, carotid) or arm (axillary, brachial) on one or both sides and by the recording of unequal or abnormally low pressures in the upper extremities. Waveforms recorded by Doppler tracings are dampened in arteries whose origins are stenosed or occluded. Bruits may be present. In patients with subclavian steal, a pulse lag may be felt between the radial arteries of the two arms or, more precisely, a pulse wave delay of greater than 30 msec can be measured by simultaneously recording both brachial artery waveforms.2 Claudication of the arm and digital artery embolization may be present in subclavian artery disease. A computed tomographic scan of the brain is an essential part of the workup for patients with disease of the SATs. The scan may reveal clinically silent cerebral infarctions.3
Indications for Surgery
Vertebrobasilar ischemia may be due to stenosis or occlusion of the vertebral or basilar arteries, restricting flow in the territory supplied by these arteries. This is the so-called low-flow (or hemodynamic) mechanism. These patients often have repetitive transient ischemic attacks triggered by positional or postural mechanisms. Although their risk for stroke is lower than that in patients with carotid disease, they may suffer serious traumatic injuries because of loss of balance (such as syncopal attack while driving). In patients with low-flow symptoms of ischemia in the vertebrobasilar territory, the surgical indication rests on the assumption that the basilar artery is not receiving adequate inflow from the vertebral arteries. Ischemia of the vertebrobasilar territory may also be due to microembolization (atheroemboli). Contrary to prevalent views in the neurologic literature, approximately one third of vertebrobasilar ischemic episodes are caused by atheroembolization from plaques or mural lesions of the vertebral arteries.4 Patients with embolic symptoms are at high risk for infarctions of the brainstem, cerebellum, and occipital lobes. The mechanism here is microembolization from the irregular surface or from the core of a plaque in the proximal subclavian or vertebral arteries or from a lesion in the wall of the vertebral artery secondary to repetitive trauma from an osteophyte or from intramural dissection.
Reconstruction of the Supra-Aortic Trunks
Cervical Repairs
In the early 1970s, techniques for revascularization of the SATs consisted of a transverse bypass between a donor and a recipient (diseased) artery. The insertion of a bypass between the carotid and subclavian arteries, although described in 1957,5 did not become popular until the 1970s. These bypasses were between the midsegment of the carotid artery and the second (retroscalene) segment of the subclavian artery. In some cases, the carotid artery acted as the donor vessel, and the bypass corrected a blockage of the first portion of the subclavian artery. In others, the subclavian artery was the donor vessel to bypass a proximal common carotid artery lesion. In subclavian-carotid bypasses, when the anastomosis to the carotid artery is of the end-to-side type, there is always the possibility of a source of proximal embolization (from the diseased proximal common carotid artery) or of extension of the proximal thrombus across the end-to-side anastomosis. As a result, an end-to-end anastomosis (see later) into the common carotid artery is recommended.
Many of the cervical bypasses done in the 1970s used saphenous vein as the preferred graft material. There was fear of embolization from the “neointima” of prosthetic tubes and doubts about their long-term patency. However, saphenous veins also presented specific problems. They were not always available, and gross mismatches in caliber often occurred between the vein and the recipient arteries. In addition, the length required for remote bypasses led to the possibility of axial rotation or compression or kinking of the vein graft with rotation of the neck. Because of these difficulties, surgeons explored the use of prosthetic substitutes for arterial bypass in the neck. The reported results indicate that polytetrafluoroethylene (PTFE) grafts are preferable to saphenous vein for bypasses in the neck; they provide a good-caliber match, and their patency rates are excellent,5 probably as a result of the high flow rates usually measured in these arteries.
Anatomic Indications
Common Carotid Artery Occlusion or Stenosis.
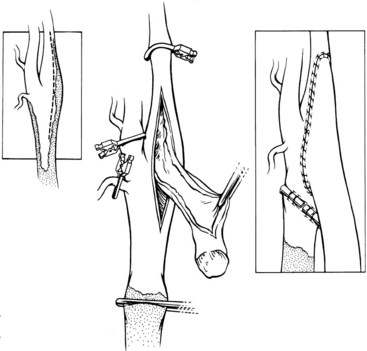
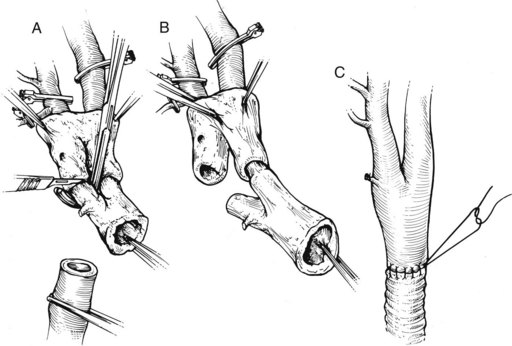
The common carotid artery can be revascularized by means of a subclavian-carotid bypass from the ipsilateral subclavian artery, with the distal anastomosis being performed end to end to avoid embolization from the diseased proximal common carotid artery. When the entire carotid system on one side is not visualized on the arteriogram, one must consider the possibility that the carotid bifurcation is patent, with retrograde flow from the external carotid artery perfusing the internal carotid artery antegradely. Delayed subtraction films may show this late opacification, but duplex imaging is the best way to show patency of the carotid bifurcation and this peculiar combination of retrograde (external carotid) and antegrade (internal carotid) flow. In these patients, atheromatous plaque is usually found at the origin of the internal carotid artery, necessitating endarterectomy before performing the distal anastomosis. The traditional means of constructing a distal anastomosis for a graft at the level of the carotid bifurcation is with an end-to-side junction (an onlay patch), with or without a concomitant endarterectomy of the carotid bulb (Figure 19-1). This end-to-side anastomosis is functionally transformed into an end-to-end junction by ligation of the common carotid artery below the anastomosis, in the soft segment created by endarterectomy of the distal portion of the common carotid artery. A preferable technique for the distal anastomosis is (Figure 19-2): to amputate of the distal common carotid artery, the carotid bulb is then everted for endarterectomy (type 2 eversion). The round cross section of the carotid bifurcation allows a simple end-to-end anastomosis to the bypass arising from the subclavian artery.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree