Small cell lung cancer (SCLC) is a virulent, rapidly growing, early metastasizing, invasive cancer. SCLC represents approximately 15% of all lung cancers and up to 25% of lung cancer deaths each year in the United States.
1 At diagnosis, approximately 90% of patients will have regional or distant spread. Although the incidence of SCLC in the United States is decreasing, there have been only modest improvements in survival noted over the past 30 years.
2Although several decades ago, surgery for SCLC was the treatment of choice, this was abandoned following the 1973 report of the British Medical Research Council, which randomized patients with limited disease SCLC to either surgery or radiotherapy alone.
3,
4,
5 It was concluded from this study that radiotherapy was preferable to surgery. Subsequently, it has been shown that SCLC can exhibit an initial dramatic response rate to chemotherapy and radiation therapy.
2 Numerous clinical trials have reported response rates of 80% to 90%. Nevertheless, despite this initial response to therapy, most patients ultimately die from this disease. For patients with limited-stage disease, the most frequent site of chemoradiotherapy treatment failure is localized recurrence.
6,
7 It is this sobering fact that has led many to reconsider surgery as part of the treatment armamentarium of SCLC. This chapter will review four clinical circumstances in which surgery may be beneficial in the treatment of SCLC: (a) SCLC presenting as a solitary pulmonary nodule (SPN) and diagnosed at the time of surgery, (b) mixed histology (i.e., SCLC and non-SCLC combined) lung cancers, (c) salvage therapy for local failure of chemoradiotherapy, and (d) planned multimodality therapy consisting of induction chemotherapy followed by surgery for limited-stage SCLC.
HISTORICAL BACKGROUND
Mountain
8 reported the MD Anderson Hospital and Tumor Institute’s surgical experience for 368 patients with pathologically proven SCLC and found only one patient surviving greater than 5 years as compared to 15% to 25% 5-year survival for non-small cell lung cancer (NSCLC). Mountain
8 did not identify any prognostic factors positively influencing survival and concluded that SCLC was a nonsurgical disease warranting systemic treatment.
To try and determine if it was ever appropriate to utilize surgery as primary treatment for SCLC, a prospective randomized trial was undertaken by the Medical Research Council of Great Britain.
3,
4,
5 In this study, 144 patients were diagnosed with SCLC by bronchoscopy, and then randomized with 71 having surgical resection and 73 radiotherapy (>30 Gy over 20 to 40 days). Median survival for the surgical patients was 199 days compared to 300 days for the radiotherapy patients. At 5 years, one and three patients were alive in the surgical and radiotherapy arms, respectively (
p = 0.04), and at 10 years, only the three radiotherapy patients remained. This study discredited surgery for SCLC for years to come. Retrospectively, the British Medical Research Council study has been criticized in several areas: (a) initial staging was crude compared with today’s preoperative staging modalities, and many of the patients likely would have been deemed inoperable, (b) only patients with central tumors were included since all required bronchoscopy for diagnosis, peripheral tumors, which might have received the most benefit were excluded, (c) only 48% of the surgical patients had complete surgical resection, all of which entailed pneumonectomy, and (d) no intraoperative staging was performed.
9,
10,
11,
12 Subsequently, the addition of preope rative radiotherapy was examined; however, no survival advantage was achieved.
13,
14,
15 Considering these facts, some surgeons still believed in the role for surgery in select patients with SCLC; therefore, further investigations were continued.
Table 38.1 outlines the results of surgery alone for SCLC.
It became evident to the 1960s and 1970s investigators that most patients with SCLC were dying from systemic metastatic disease, and that effective systemic treatment was needed. Bergsagel et al.
25 showed an improved overall survival with the addition of low-dose cyclophosphamide to radiation therapy. Similarly, the British Medical Research Council Lung Cancer Working Party
26 showed improved disease-free survival with multiagent chemotherapy and radiation. Concurrently, other investigators were applying the same adjuvant chemotherapy
principles to surgical SCLC patients. The Veterans Administration Surgical Adjuvant Group (VASOG) in the United States showed no survival benefit in 417 lung cancer patients (both SCLC and NSCLC) treated by either surgery alone, surgery plus single-agent chemotherapy, or surgery plus multiagent chemotherapy.
27 When considering those patients specifically diagnosed with SCLC, 4 out of 18 total patients were alive at 3 years, none being in the surgery alone arm. This was the first study demonstrating a possible increased survival for patients with SCLC who underwent adjuvant chemotherapy following complete surgical resection.
27In 1982, Shields et al.
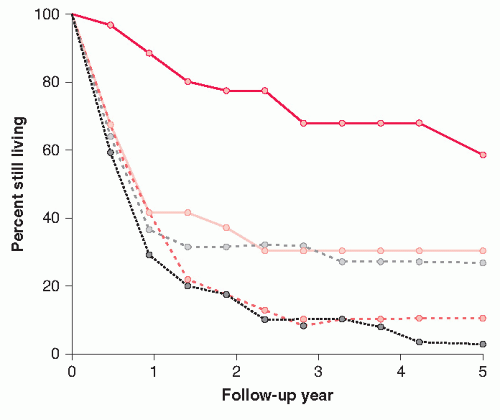
28 evaluated four of the VASOG adjuvant chemotherapy trials, which resulted in the reawakening of surgical interest in the treatment of limited disease SCLC. This study analyzed 148 patients diagnosed with SCLC who had undergone potentially curative resection. There were 16 operative deaths, and in the remaining 132 patients, the overall 5-year survival was 23%. Although in this study, there was no benefit shown with adjuvant chemotherapy, the importance of the TNM (tumor, node, metastasis) staging SCLC was demonstrated. SCLC patients with T1N0M0 tumors had a 60% 5-year survival, T1N1M0 31%, T2N0M0 28%, T2N1M0 9%, and any T3 or N2 3.6%.
28 (
Fig. 38.1) SCLC may occasionally present as an SPN. In 1975, Higgins et al.
29 reported on a VASOG trial involving 1134 patients with asymptomatic SPN. The 392 patients underwent resection for lung cancer, and 15 (4%) were found to have SCLC. The 1-, 5-, and 10-year survivals were 64%, 36%, and 18%, respectively.
29 In a retrospective review of 40 patients who underwent potentially curative resection for SCLC between 1959 and 1972, overall 5-year survival was 25%, and long-term survival was 40% in patients without
metastatically involved lymph nodes.
18 Similarly, Angeletti et al.
30 suggested that survival was statistically influenced by the N stage rather than T stage. Their results demonstrated that patients with T1, T2, and T3 SCLC tumors, without evidence of lymph node involvement, might benefit from surgical resection and adjuvant chemotherapy. SCLC typically presents as a central mass. Lennox et al.
19 observed that patients with more proximal tumors requiring pneumonectomy had worse survival than patients requiring lobectomy. The 2- and 5-year survival rates for patients undergoing lobectomy were 32% and 18%, respectively, compared with 14% and 7% for patients having pneumonectomy.
19Although some authors may consider the combination of chemoradiotherapy to be the standard of care for limited disease SCLC,
31 from this historical review, it is suggested that various subpopulations of patients with SCLC might benefit from surgery. Whether surgery can offer any substantial advantage over radiotherapy in terms of local control is still an unanswered question. However, we concede that if surgery is to have any meaningful role in the treatment of SCLC, it must be in the context of a combined modality treatment regimen, which includes systemic chemotherapy and possibly radiotherapy.