■ Alternatively, especially in obese patients with substantial abdominal pannus, a curvilinear incision can be placed 1 cm below and parallel to the inguinal ligament to avoid potential skin maceration and wound complications that may accompany vertical incisions in this situation (FIG 1, dashed line B). Although the proximal superficial femoral and deep femoral arteries can be exposed via this incision, such a curvilinear or oblique incision limits further distal arterial exposure. It therefore would not be selected if an extensive common and deep femoral artery endarterectomy is anticipated as potentially necessary to optimize inflow.
■ The incision is carried sharply through the subcutaneous tissue and superficial fascia.
Dissection and Control of the Common, Superficial, and Proximal Deep Femoral Arteries
■ Deep to the subcutaneous tissue and superficial fascia, the dissection is extended longitudinally, even when using an oblique incision, to optimize the length of femoral exposure. Depending on the depth of dissection and subcutaneous adiposity, self-retaining Weitlaner or cerebellar retractors are carefully placed to optimize exposure while avoiding traction injury to femoral nerve branches or the common femoral vein. Further dissection through the femoral sheath exposes the anterior surface of the femoral artery.
■ The dissection plane should remain centered directly over the femoral artery. Encountering venous structures indicates medial deviation from the optimal plane; exposure of the iliopsoas muscle, femoral nerve fibers, or lymphatic vessels is an indication of lateral deviation. An increasing incidence of femoral incisional complications, including wound edge necrosis and separation, lymphatic leaks, femoral neuropraxia, and venous injuries are associated with incorrectly placed inguinal incisions for femoral exposure.
■ Dissect directly along the CFA both proximally and distally. Placement of silastic vessel loops around the femoral artery and its larger branches aids in retraction, dissection, and mobilization.
■ Proximal dissection is continued along the CFA to the inguinal ligament. The inguinal ligament may be divided to aid in exposure or to enable extended endarterectomy. Caution is necessary in this area, as a prominent femoral vein tributary crosses anteriorly over the CFA in this area and is prone to injury if not identified, ligated, and divided early in the dissection. Inadvertent injury to this “vein of pain” produces retraction and troublesome bleeding. The medial and lateral femoral circumflex arteries, important collaterals in iliofemoral arterial occlusive disease, are identified at level of the inguinal ligament and individually controlled with removable clips or silastic vessel loops. Use of the former reduces clutter in the wound during endarterectomy or creation of the proximal anastomosis.
■ As the dissection proceeds distally, an abrupt change in caliber marks the femoral bifurcation and the origins of the deep (also known as “profunda femoris” in Latin) and superficial femoral arteries (SFA). The latter continues distally in the same plane; the former usually courses posteriorly and laterally away from the femoral bifurcation. After silastic loops are placed on each vessel, gentle upward traction on the CFA or SFA may help bring the deep femoral artery into view. The lateral circumflex iliac vein may course anteriorly over the origin of the deep femoral artery and should be ligated and divided to optimize exposure and control of the first segment of this vessel (FIG 2A).
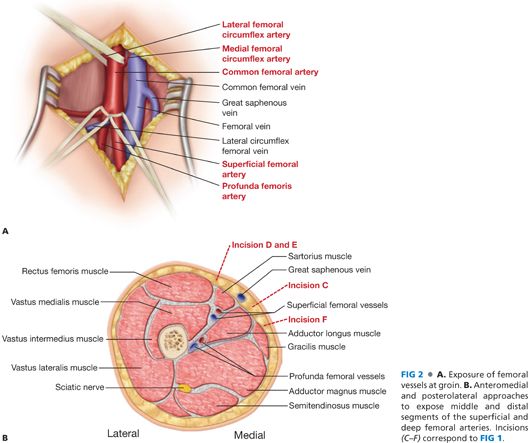
■ Medial and distal dissection provides extended exposure of the proximal SFA (FIG 1, dashed line F). This vessel only occasionally has small branches in its proximal segment. A sensory branch of the femoral nerve may be present crossing the SFA from lateral to medial. Transection may result in medial thigh discomfort. Even extended femoral bifurcation dissections rarely require division of femoral nerve branches, which should be avoided to minimize postoperative paresthesias and dysesthesias.
Exposure of the Middle and Distal Segments of Deep Femoral Artery
■ Exposure of the distal portions of the deep femoral artery often enables use of shorter vein conduit in distal leg bypass or may improve outflow from proximal revascularization procedures (iliac angioplasty and stenting or aortofemoral bypass). These segments are easily exposed from either posteromedial or anteromedial approaches (FIG 1, dashed line C–F). The approach should be dictated by the indication (inflow sources or outflow target); an additional consideration is the necessity to obtain exposure in a native field, either in the setting of prior dissection or femoral graft infection.
■ Incisions are placed along either the medial (anteromedial approach; dashed line C and F in FIG 1) or lateral borders (posterolateral approach) of the sartorius muscle (FIG 1, dashed line D and E). The dissection plane is developed through the subcutaneous tissue and fascia, passing lateral or medial to the sartorius, respectively. Mobilize and retract sartorius muscle laterally or medially, depending on approach.
■ The dissection is continued posteriorly, passing lateral to the superficial femoral vessels and accompanying nerve, to the space between the adductor longus muscle (medially) and vastus medialis (laterally) (FIG 2B, incisions C–E). The deep femoral artery and vein pass directly underneath.
■ Dissection between adductor longus and vastus medialis muscle exposes the middle segments of the deep femoral artery. Crossing venous tributaries should be ligated and divided as necessary to provide optimal exposure. The more distal segments of deep femoral artery begin to course posterior to the femur beyond this point and are therefore less useful for bypass origination or destination.
■ Alternatively, exposure between the adductor longus (anteriorly) and gracilis muscle (posteromedially) enables medial exposure of the deep femoral artery in the distal thigh (FIG 1, dashed line F; FIG 2B, incision F).
POPLITEAL ARTERY EXPOSURE
Medial Exposure of the Above-Knee Popliteal Artery
■ Place patient in supine position. Rotate leg laterally, flex the leg, and place a bump underneath the knee joint.
■ Place a 10- to 12-cm longitudinal incision along the groove formed between the edges of the vastus medialis (anteriorly) and the sartorius muscles (posteromedially) (dashed line A in FIG 3A). The incision is carried through the subcutaneous tissue and fascia. Place self-retaining retractor. Take care not to trap and injure the great saphenous vein and the saphenous nerve. The great saphenous vein is likely to be encountered more posteromedially to the incision in the subcutaneous tissue. The saphenous nerve may be encountered at distal end of the incision as it joins the saphenous vein near the medial aspect of the knee.
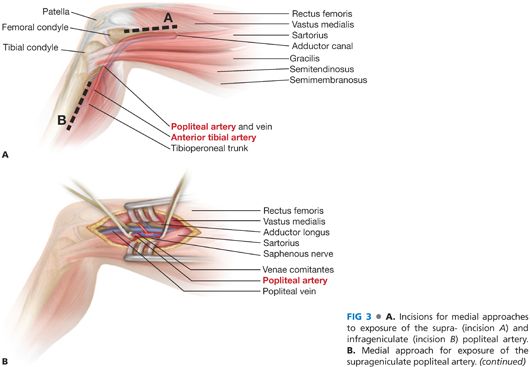
■ Incise the deep fascia longitudinally and above the sartorius muscle to enter the popliteal fossa. The popliteal artery can be palpated up against the posterior surface of the femur (FIG 3B).
■ The popliteal artery is often surrounded by multiple venous collaterals, or “venae comitantes” in Latin; the popliteal vein is usually posterolateral to the artery in this location. The popliteal and/or superficial femoral veins may be duplicated throughout the popliteal fossa and distal thigh. Isolation and control of the artery usually requires ligation and division of surrounding collateral veins.
Lateral Exposure of the Above-Knee Popliteal Artery
■ Lateral exposure of the above-knee (AK) popliteal artery is useful in a variety of circumstances—for instance, axillopopliteal bypass or when the medial approach has previously been developed or is complicated by infection or injury.
■ Place patient in supine position. Rotate leg medially, flex the knee, and place a bump underneath the knee joint.
■ Place 10- to 12-cm longitudinal incision between the vastus lateralis and the biceps femoris muscles (dashed line A in FIG 4A). The incision is carried through the subcutaneous tissue and fascia.
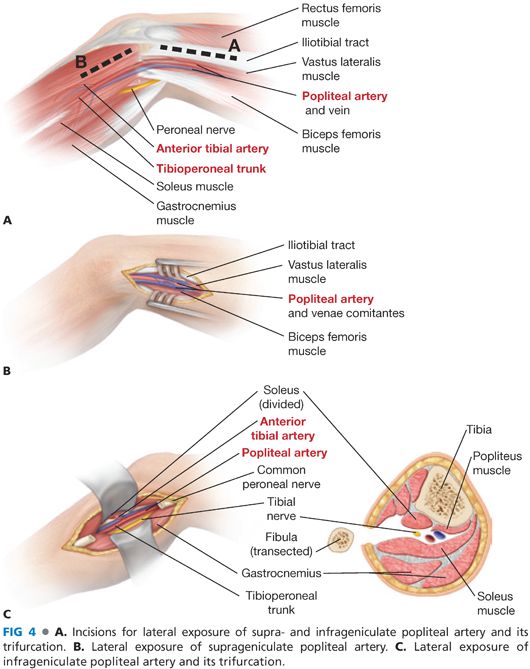
■ Make a generously cruciate incision (“T-ed”) at both ends on the fascia lata to prevent bypass graft impingement by its dense fibers.
■ Place retractor and enter the popliteal space. Sciatic nerve then popliteal vein will be encountered first before popliteal artery. Gently retract sciatic nerve downward. Then mobilize and retract popliteal vein to expose and control the popliteal artery.
Posterior Exposure of the Popliteal Vessels
■ Posterior exposure may be the preferred approach for management of popliteal artery entrapment, popliteal cyst, focal popliteal artery aneurysm, or arterial injury following traumatic posterior knee dislocation. Although direct and relatively uncomplicated, posterior access is limited by the heads of the gastrocnemius muscle distally and the biceps femoris/“hamstring” muscles proximally; only focal, limited popliteal artery access is achievable through this incision.
■ Patient is placed in prone position with pillow to prop up the lower leg and foot.
■ The incision is S-shaped, across the posterior crease of the knee joint, with its superior extent beginning medially.
■ The incision is carried anteriorly through the subcutaneous tissue and superficial fascia to enter the popliteal fossa. Exposure is maximized by mobilizing the popliteal artery between the two heads of the gastrocnemius muscle inferiorly and between semimembranosus and biceps femoris muscle superiorly.
■ The muscles are gently retracted to expose the entire popliteal fossa. The tibial and common peroneal nerves are encountered superficially in this exposure. The popliteal artery is anterior, or deep to the vein, in the depths of the wound.
■ It may be necessary to mobilize the popliteal vein with ligation and division of popliteal venous tributaries to fully expose the artery. Once the appropriate segment is exposed, silastic vessel loops are placed proximally and distally.
INFRAGENICULAR EXPOSURE
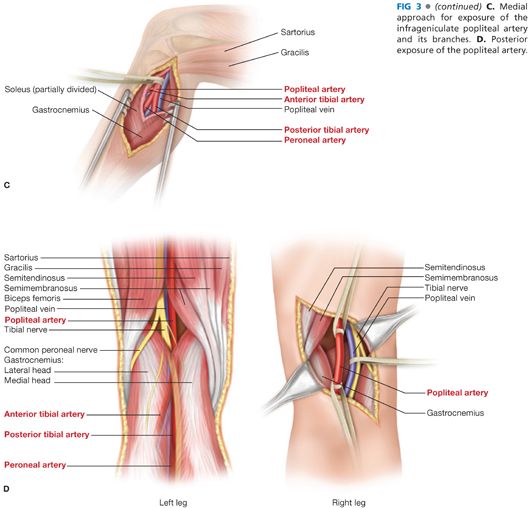
Medial Exposure of the Infragenicular Popliteal Artery and Its Branches
■ The most common approach is a medial one (FIG 3A).
■ Place patient in supine position. Rotate leg laterally, flex the leg, and place a bump underneath the knee joint.
■ Make a longitudinal incision from below the edge of the tibia along the course of the great saphenous vein (dashed line B in FIG 3A).
■ Carry the incision through subcutaneous tissue and fascia into the deep posterior compartment. The below-knee (BK) popliteal vessels reside deep in the wound and are partially covered by the origin of the soleus muscle.
■ Division of the soleus origin medially (FIG 3C) will facilitate exposure of the tibioperoneal trunk, and origin of the anterior tibial artery, but is not really necessary for exposure of the popliteal artery itself. As was described for the posterior approach, the artery lies in close proximity to the popliteal vein and tibial nerve. Mobilization of the popliteal vein from the adjacent artery is necessary for sufficient exposure of all relevant structures, including the anterior tibial artery, tibioperoneal trunk, and derivative branches (posterior tibial and peroneal arteries). It is usually necessary to ligate and divide the anterior tibial vein at its confluence with the (often paired) popliteal vein to gain sufficient exposure to isolate and mobilize the more distal branches.
■ Dissection must proceed deliberately to avoid injury to the neighboring tibial nerve and its distal branches.
Lateral Exposure of the Infragenicular Popliteal Artery and Its Trifurcation
■ The lateral approach is rarely required but may be particularly useful to avoid scarring from a previous medial approach.
■ Place the incision posterior to the head of the fibula and extend along the course of the fibula. Dissect directly onto fibula (incision is marked as dashed line B in FIG 4A). Note the location of the common peroneal nerve, which courses from posterior to anterior around the neck of the upper fibula just below its head, before it branches into the superficial and deep peroneal nerves.
■ Circumferentially elevate the periosteum of the fibula and excise the exposed segment of the fibula with a saw. The popliteal vessels and branches are found directly beneath the fibular periosteum, with the artery usually located anterior to the posterior tibial nerve and the popliteal vein.
■ Extending the dissection distally allows exposure and control of distal popliteal artery, as well as the origins of the anterior tibial and the tibioperoneal trunk.
Exposure of the Anterior Tibial Artery
■ Proximal segment
■ The proximal segment of the anterior tibial artery is exposed in a fashion similar to the exposure for the infragenicular popliteal artery and its branches.
■ Middle segment
■ The middle segment exposure of the anterior tibial artery is useful when there is limited length of autogenous vein.
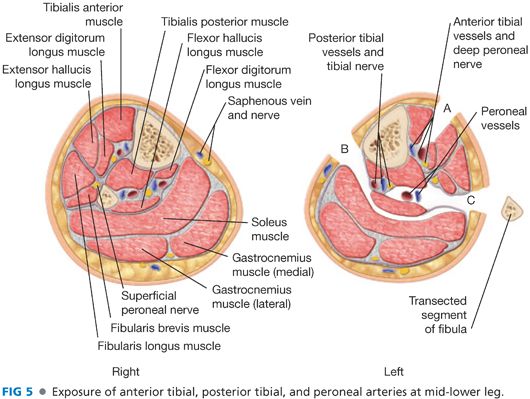
■ Place an axial incision in a vertical plane about two fingerbreadths lateral to the anterior edge of the tibia (FIG 5A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


