Supraventricular Tachycardia
Introduction and Mechanisms
Supraventricular tachycardia (SVT) refers to regular, narrow QRS complex rhythms typically in excess of 100 beats per minute (bpm). Atrial flutter and atrial fibrillation will be discussed separately. The prevalence of SVT in the general population is 2.25 per 1,000 persons with an incidence of 35 per 100,000 person-years. In the absence of preexcitation, these tachycardias are divided into three major categories: atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia due to a concealed accessory pathway (AP) (circus movement tachycardia [CMT]), and atrial tachycardia (AT). Although these three categories encompass the vast majority of regular, narrow-complex tachycardias, other rare tachycardia mechanisms separate from these may exist such as junctional ectopic tachycardia (JET).
AVNRT is the most common form of SVT. It is a form of reentry involving two functional “dual” pathways in the AV node. Although the true circuit is functionally based rather than anatomically based, AVNRT has been described as following a protected circuit within the AV node or AV junctional region along so-called slow pathway (SP) and fast pathway (FP). The SP input has been localized to the inferior portion of the triangle of Koch between the ostium of the coronary sinus (CS) and the septal leaflet of the tricuspid valve.
The FP input has been localized to the superior aspect of the tendon of Todaro at or just above this His bundle (see Fig. 8-1).
The FP input has been localized to the superior aspect of the tendon of Todaro at or just above this His bundle (see Fig. 8-1).
Dual pathways are required but not sufficient to have AVNRT. There must be block in one pathway and slow conduction in the other to allow reentry (echo beat) and this must be continuous to allow tachycardia (see Fig. 8-2). Linking of SP and FP is required for reentry to occur. Many patients will demonstrate dual pathways without being able to sustain tachycardia. In such cases there may be no linking, or more commonly a weak retrograde limb.
 FIGURE 8-1. Schematic of the functional anatomy of the atrioventricular (AV) node in the right anterior oblique (RAO) view. (See color insert.) |
The typical or common form of AVNRT (97% of cases of AVNRT) involves antegrade conduction down the SP and retrograde conduction up the FP. The P wave is generated by the retrograde conduction from the AV node to the atrium. This generates a negative P wave, which is often buried in the QRS complex and invisible on the surface electrocardiogram (ECG). The P wave is seen within the QRS because retrograde conduction is rapid, occurs simultaneous with conduction to the ventricle, and the P wave is narrow. The uncommon or atypical form of AVNRT (3% of cases of AVNRT) conducts down the FP and back up the SP and is manifest as a long RP tachycardia with negative surface P waves in 2, 3, and aVF (see Fig. 8-3). P waves in this form of AVNRT tend to be broader and deeper than in typical AVNRT because earliest activation is near the CS ostium.
Atrioventricular Reentrant Tachycardia
Atrioventricular reentrant tachycardia (AVRT) refers to tachycardias which utilize an AP as at least one limb of the tachycardia (Fig. 8-3B). If there is
antegrade or manifest conduction over the AP in sinus rhythm and there is documented SVT it is called Wolff-Parkinson-White syndrome (see Chapter 9). If the pathway only conducts in the retrograde direction it is a “concealed” pathway. APs are considered congenital abnormalities. The locations of concealed APs are similar to manifest APs. Of all patients with SVT using a concealed AP, up to 10% have a second AP. Ninety percent of concealed APs are rapidly conducting. Of rapidly conducting concealed APs, 60% are left free wall, 27% are posteroseptal, 5% are anteroseptal, and 8% are right free wall. Because the circuit necessitates conduction through the His-Purkinje system (HPS) to the ventricles and then up an AP, the retrograde limb (represented by the VA interval) is longer than in AVNRT which does not need to reach the ventricle before activating the atrium. Unlike the AV node, which is characterized by decremental conduction, accessory atrioventricular connections tend to conduct in an “all-or-none” manner.
antegrade or manifest conduction over the AP in sinus rhythm and there is documented SVT it is called Wolff-Parkinson-White syndrome (see Chapter 9). If the pathway only conducts in the retrograde direction it is a “concealed” pathway. APs are considered congenital abnormalities. The locations of concealed APs are similar to manifest APs. Of all patients with SVT using a concealed AP, up to 10% have a second AP. Ninety percent of concealed APs are rapidly conducting. Of rapidly conducting concealed APs, 60% are left free wall, 27% are posteroseptal, 5% are anteroseptal, and 8% are right free wall. Because the circuit necessitates conduction through the His-Purkinje system (HPS) to the ventricles and then up an AP, the retrograde limb (represented by the VA interval) is longer than in AVNRT which does not need to reach the ventricle before activating the atrium. Unlike the AV node, which is characterized by decremental conduction, accessory atrioventricular connections tend to conduct in an “all-or-none” manner.
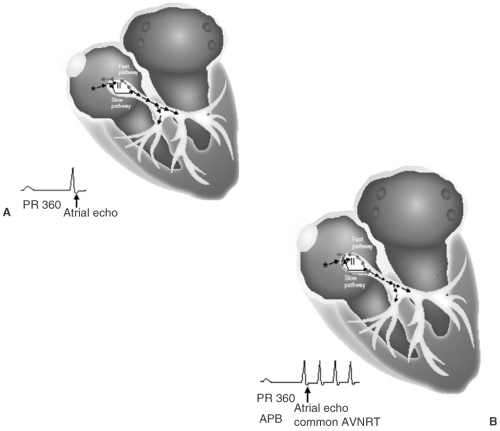 FIGURE 8-2. Diagrams of a typical atrioventricular (AV) nodal echo (A) and the initiation of atrioventricular nodal reentrant tachycardia (AVNRT) (B). The black arrow represents initial conduction down the slow pathway. The blue arrows demonstrate retrograde conduction up the slow pathway (echo beat) with subsequent conduction back down the slow pathway with initiation of AVNRT. (See color insert.) |
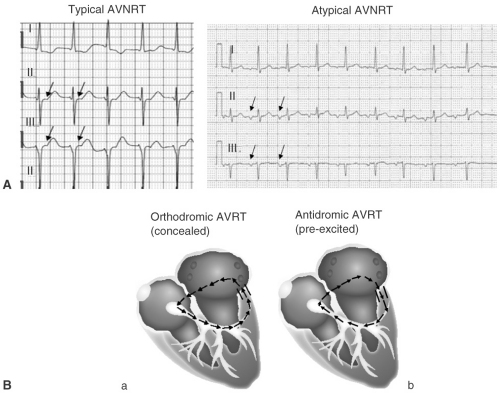 FIGURE 8-3. A: Electrocardiographic examples of typical (short RP) and atypical (long RP) atrioventricular nodal reentrant tachycardia (AVNRT). B: Atrioventricular reentrant tachycardia. (See color insert.) |
During SVT with antegrade AV nodal conduction and retrograde conduction over an AP (orthodromic AVRT), retrograde conduction is said to conduct rapidly when the ECG RP interval is less than the PR interval. Although this is a good general rule, absolute RP intervals of up to 170 msec could be rapidly conducting. The RP interval is affected by the AV nodal conduction and the presence of bundle branch block (BBB). Tachycardias employing rapidly conducting APs tend to be paroxysmal. A small minority of SVTs using a concealed AP as the retrograde limb of circuit may demonstrate longer RP intervals (greater in duration than the PR interval) and are called slowly conducting APs. These APs frequently demonstrate decremental properties and can be incessant (PJRT or the permanent form of junctional reciprocating tachycardia). AVRT which conducts antegradely over the AP and retrogradely over the AV node or a second AP are called antidromic tachycardias.
Atrial Tachycardia
This is a form of SVT in which an atrial source drives the tachycardia independent of the route of AV conduction. The mechanism of this tachycardia may be
automatic, triggered, or less commonly, reentrant. Reentrant forms of AT are generally considered macroreentrant if they can be entrained from sites over a distance of 1 or 2 cm whereas microreentrant circuits are more focal in nature. Large macroreentrant circuits are often related to atrial scarring. Frequently, AT is associated with structural heart disease and associated conditions such as myocardial infarction, chronic obstructive pulmonary disease (COPD), alcohol ingestion, hypoxia, hypokalemia, increased catecholamine states, and digoxin toxicity. Automatic atrial tachycardias (AATs) can be incessant and occasionally cause tachycardia-mediated cardiomyopathy.
automatic, triggered, or less commonly, reentrant. Reentrant forms of AT are generally considered macroreentrant if they can be entrained from sites over a distance of 1 or 2 cm whereas microreentrant circuits are more focal in nature. Large macroreentrant circuits are often related to atrial scarring. Frequently, AT is associated with structural heart disease and associated conditions such as myocardial infarction, chronic obstructive pulmonary disease (COPD), alcohol ingestion, hypoxia, hypokalemia, increased catecholamine states, and digoxin toxicity. Automatic atrial tachycardias (AATs) can be incessant and occasionally cause tachycardia-mediated cardiomyopathy.
Focal ATs generally develop in distinct anatomic locations. The crista terminalis is the most common site of AT in the right atrium and the pulmonary veins are the most common site of AT in the left atrium. Other important sites of AT include the lateral tricuspid annulus, CS ostium, para-Hisian region, mitral annulus, and atrial appendages. ATs coming from the superior crista terminalis may lie close to or originate within the sinus node complex. Reentry within the sinus node (sinus node reentry) can be considered a form of right AT. Rates in AT are often slower (100 to 180 bpm) than AVNRT or AVRT, but overlap exists.
Sinus tachycardia can be classified as appropriate in response to a stimulus such as anemia, volume depletion, or hyperthyroidism or inappropriate, indicating a rapid rate without a clear cause. Inappropriate sinus tachycardia may be due to reentry within the sinus node (sinus node reentry). Sinus node reentry tends to begin with a premature beat or rapid atrial rates and terminate spontaneously. Inappropriate sinus tachycardia may also occur as a syndrome in which the sinus rate increases in response to physical exertion, positional change, or emotional stimuli but remains rapid long after the stimulus is over. Postural orthostatic tachycardia syndrome (POTS) is a form of inappropriate sinus tachycardia in which movement from a supine to upright posture without associated orthostatic hypotension results in prolonged tachycardia. This is distinguished from orthostatic hypotension in which tachycardia occurs appropriately in response to a positional fall in blood pressure.
Clinical Presentation
Demographics
The age of onset of tachycardia or palpitations and in some cases the gender of the patient, can help narrow down the differential diagnosis of SVT. Advanced age and the presence of structural heart disease increase the likelihood of AT. Conversely, palpitations since childhood favor AVRT. The onset of tachycardia during early adulthood, often with a period of quiescence and then recurrence in middle age is typical of AVNRT. However, AVNRT can present at any age. Male gender, particularly in a young person favors AVRT, whereas female gender, regardless of the age of onset, favors AVNRT.
Symptoms and Circumstances
Several signs and symptoms may suggest a particular type of SVT. For example, a pounding sensation in the neck may indicate atrial contraction against closed AV valves, which can be seen frequently in AVNRT due to near-simultaneous depolarization of the atria and ventricles. On physical examination, patients may display visible jugular venous pulsations (“frog sign”) due to atrial contraction against a closed tricuspid valve.
The circumstances of initiation and termination may be suggestive of a particular diagnosis. Initiation after standing up from a bent-over position is common in patients with AVNRT, possibly from carotid sinus–driven changes in autonomic tone with change in posture. Similarly, termination by a vagal maneuver is common in AVNRT or AVRT. Although an abrupt onset and offset are classic manifestations of SVT (typically AVNRT or AVRT), increased sympathetic tone from tachycardia or related anxiety may blunt the sensation of an abrupt offset of tachycardia. Younger patients often have sinus tachycardia at the termination of an SVT episode, which may mask the feeling of an acute termination. Tachycardia that is incessant may lead to a cardiomyopathy. Such tachycardias are frequently due to AT or a slowly conducting AP (e.g., PJRT). The PJRT is characterized by an initiation with preceding sinus acceleration. It is often only slightly faster than the resting sinus rate and can start and stop throughout the day. Both AT and PJRT are sensitive to catecholamines, resulting in very rapid rates during daily exercise and slower rates at rest.
Diagnosis
Electrocardiography
Because most SVTs can be diagnosed by ECG, great efforts should be made to document episodes of SVT on a 12-lead ECG before instituting empiric therapy. When a systematic approach is followed, diagnostic accuracy is improved.
P-Wave Axis and Morphology
The first step in analysis is to localize atrial activity. Because identification of the P wave may be difficult, perturbations in the tachycardia or comparison to a sinus rhythm tracing may provide assistance.
P waves that are identical to the sinus P wave suggest sinus node reentry or an AT coming from a site in the right atrium near the sinus node. P waves that are inverted in the inferior leads suggest retrograde activation of the atria as is characteristic of AVNRT or AVRT using a concealed AP in the posteroseptal region of the heart as the retrograde limb. A low right AT coming from the region of the CS can also produce a negative P wave in the inferior leads.
AT can usually be localized by P-wave morphology (see Table 8-1). Generally, an upright P-wave axis in the inferior limb leads favors AT over AVRT and rules out AVNRT. ATs originating in the left atrium most often have a positive (+) or occasionally a negative then positive (±) P wave in lead V1 and frequently negative or biphasic P wave in aVL. Tachycardias arising from superior locations in either atrium (e.g., superior crista terminalis) have an inferior P-wave axis (+ II, III, and aVF), whereas ATs from inferior locations in the atria (e.g., CS ostium or inferolateral crista terminalis) have a superior (–II, III, and aVF) P-wave axis. A negative P wave in aVR suggests a site in the right atrium such as the sinus node or the crista terminalis but can be seen from the high right atrial septum or occasionally the right superior pulmonary vein. A characteristic “w-shaped” P wave is seen in AT arising from the lateral tricuspid valve (see Fig. 8-4).
ATs arising from the pulmonary veins are characterized by P waves that are positive across the precordial leads from V1 to V6, negative (−) or isoelectric in aVL, and negative in aVR. Notching is commonly seen in P waves produced by ATs from the left-sided veins in the inferior and precordial leads. P waves in V1 are often wider in ATs from the left-sided veins compared with right-sided veins, and a positive P wave in lead I is highly suggestive of a right-sided focus. Additionally, the inferior leads are usually positive with a superior vein origin of AT.
When AVRT is considered, P-wave characteristics can localize the AP. During SVT using a septal AP as the retrograde limb, P waves are usually negative in II, III, aVF and positive in aVR and aVL, and biphasic or isoelectric in V1. PJRT, which is a long RP tachycardia that is due to a concealed, slow decremental AP (>50 msec increase in VA with SVT or pacing) often reveals large inverted P waves in II, III, aVF (see Fig. 8-5). These pathways are located in the posteroseptal region. During SVT using a left free wall AP as the retrograde limb, P waves are usually negative in I whereas with right free wall pathways, the P wave is positive in I and negative in V1.
P-Wave Relationship to the QRS
The relationship of the P wave to the QRS provides important insight into the tachycardia mechanism. The presence of AV dissociation or AV block excludes the possibility of AVRT because the atria and ventricles are obligate parts of the tachycardia circuit. In the presence of AV dissociation, AVNRT is less likely than AT, but not excluded because at least in some cases the atrium is not necessary to maintain AVNRT. A clue to the presence of AVNRT with 2:1 AV block is the finding that the blocked P wave is exactly halfway between each QRS (see Fig. 8-6). In typical AVNRT, because of simultaneous activation of the atria and ventricles, a retrograde P wave might not be observed when 2:1 AV conduction is present giving the appearance of a 1:1 (A:V) tachycardia with the P wave exactly halfway between the RR interval.
TABLE 8-1 Electrocardiographic Morphology of Atrial Tachycardia
| Electrocardiographic Determination of Chamber of Origin of AT | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| a Care must be taken to measure the initial deflection of the P wave in V1; an isoelectric segment may indicate origin from the coronary sinus ostium. b V1(+) P wave during AT with V1(+/−) in SR is a better predictor of a left atrial (i.e., right superior pulmonary vein) focus than V1(+) during AT with V1(+) during SR, which may indicate a high crista terminalis focus. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| V1a,b | aVL | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Right atrium | − | + | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Left atrium | + | − | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
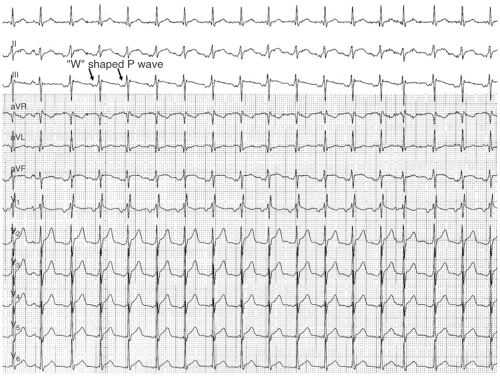 FIGURE 8-4. Electrocardiogram (ECG) of a lateral tricuspid valve annulus atrial tachycardia with the typical “W” P-wave morphology.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|