INDICATIONS/CONTRAINDICATIONS
Indications
The superior vena cava (SVC) is susceptible to invasion from tumors arising from the anterior mediastinal compartment, such as thymomas, thymic carcinoma, thyroid neoplasms, and germ cell tumors, as well as right-sided pulmonary neoplasms. Extended resection for SVC invasion (T4 disease) of nonsmall-cell lung cancer (NSCLC) and anterior mediastinal neoplasms often evokes controversy about its long-term benefit but has been associated more recently with acceptable morbidity and survival in published series. The surgeon should be familiar with the techniques used to resect and reconstruct the SVC in conjunction with the planned pulmonary resection. The most common pulmonary resection is right upper lobectomy.
Contraindications
There is little contention about SVC resection for anterior mediastinal tumors, but SVC resection in the context of NSCLC with nodal metastasis remains controversial. Staging mediastinoscopy should be performed prior to any planned resection of lung cancer to exclude N2 disease. Multistation N2 disease would be a relative contraindication to SVC resection and reconstruction by virtue of poor survival despite therapy.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
The feasibility and low morbidity of extended resection for pulmonary or mediastinal tumors infiltrating the SVC are well documented, but the selection of optimal candidates for aggressive resection is less well defined. Completeness of resection, extent of SVC involvement, and the presence of mediastinal lymph node metastases are all regarded as important in the evaluation of these select patients. Patients should be evaluated with noninvasive staging modalities such as contrast-enhanced computed tomography chest and positron emission tomography to rule out extraregional or M1 disease. Pathologic staging with mediastinoscopy, endobronchial ultrasound transbronchial lymph node biopsy, or thoracoscopy is paramount in determining a multimodality strategy in this heterogeneous population. Mediastinal MRI and sometimes cardiac-gated MRI can be considered when evaluating anterior mediastinal neoplasms to better define invasion into the great vessels or through pericardium.
 SURGERY
SURGERY
Positioning
The majority of patients with right upper lobe tumors involving the SVC can be approached through a right posterolateral thoracotomy via the fourth or fifth intercostal space (Fig. 44.1A). In contrast, median sternotomy (Fig. 44.1B) is often preferred in patients with primary mediastinal tumors involving the SVC and is ideal in patients who may require brachiocephalic vein reconstruction to the right atrium. Cardiopulmonary bypass can be considered in these cases but it is usually not necessary. A thoracosternotomy (Fig. 44.1C) incision is used in right-sided tumors that may require significant posterior mediastinal dissection. This approach allows control of the SVC and associated vasculature, particularly the right subclavian, right jugular, and left brachiocephalic venous systems. This may be of benefit for those tumors that are large and require either a concomitant chest wall resection or lysis of extensive posterior adhesions following a course of induction therapy. Moreover, for those patients needing a right upper lobe sleeve resection or a right pneumonectomy, this approach may be preferable.
Technique
Upon completing the initial exploratory approach, one should palpate the tumor and assess the degree of invasion into the SVC. Vascular control should include placement of vascular loops around left and right brachiocephalic veins and around the SVC just above the azygos vein if feasible. If the right pulmonary artery is involved, intrapericardial control of the right main pulmonary artery can be obtained between the SVC and aorta. The degree of SVC infiltration will dictate the type of resection. Primary repair should only be considered in patients when <50% of caval circumference is resected. Primary suture repair is conducted with a running nonabsorbable monofilament (polypropylene) suture usually by tangential placement of a partial occlusion clamp (Fig. 44.2). The clamp is placed from an inferior to superior direction and should include a cuff of SVC wall to permit suture placement. No systemic anticoagulation is necessary for such a limited repair where there is still flow through part of the SVC. Larger defects (where primary repair may narrow the SVC) require a patch repair (Fig. 44.3A,B). Options include bovine or autologous pericardium. Patch repair avoids narrowing of the SVC lumen and should be the preferred approach unless the defect is very small. The surgeon should plan ahead for this and have harvested autologous pericardium or retrieved a biologic or synthetic patch to reduce the amount of time that SVC flow is disrupted. Patches can be sewn with running 4-0 (polypropylene) sutures.
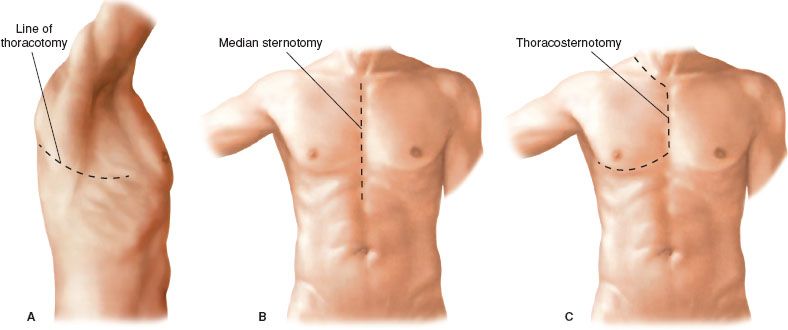
Figure 44.1 Surgical incisions used to approach SVC resection and reconstruction. A: Standard posterolateral thoracotomy, (B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


