13 Suctioning the Airway
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and WRE, it is shown simply as (Code: …). If an item is testable only on the ELE, it is shown as (ELE code: …). If an item is testable only on the WRE, it is shown as (WRE code: …).
MODULE A
1. Manipulate suctioning devices by order or protocol (ELE code: IIA8) [ELE Difficulty: R, Ap, An]
a. Get the necessary equipment for the procedure
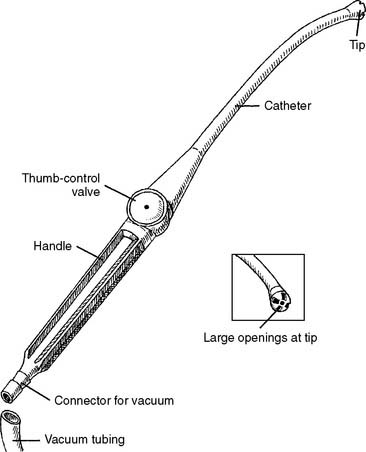
Oropharyngeal suctioning is considered a clean (not sterile) procedure. The suctioning device is often originally packaged sterile but may be used more than once. The Yankauer suction catheter is widely used, although several types are available. The Yankauer suction catheter is made of hard plastic and is angled to reach into the back of the mouth. One large opening or several medium-sized openings may be found at the tip of the catheter. The openings are large enough to permit easy suctioning of saliva, food, or vomit. Some handles include a thumb control valve so that suction can be applied to the tip only when wanted. Covering the opening with a thumb creates a vacuum at the tip for suctioning the patient’s mouth (Figure 13-1). The Yankauer may be discarded when no longer needed or sterilized for use with another patient.
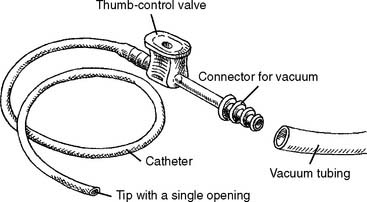
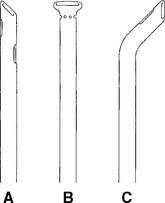
A flexible plastic or rubber catheter also can be used. It should be the largest diameter possible to reduce the chance of its becoming plugged. The opening at the catheter tip should be cut straight (perpendicular) across instead of at an angle. No side openings should be present (Figure 13-2). The catheter is discarded when no longer needed.
b. Put the equipment together and make sure that it works properly
c. Troubleshoot any problems with the equipment
If no vacuum is felt at the catheter tip, several causes are possible and must be investigated.
1. The vacuum is not turned on.
2. The system is not sealed, and the vacuum is lost to the atmosphere.
3. The system is blocked, and no vacuum can get through to the tip.
2. Suction catheters
Table 13-1 presents the recommended suction catheter sizes for the various endotracheal or tracheostomy tubes. The practitioner also can easily compare the relative sizes of the tube and suction catheter at the bedside before suctioning. Suction catheters are sized by the French (Fr) scale of the OD. Endotracheal and tracheostomy tubes are sized by ID and OD in millimeters and often by OD in French. Review Table 12-1 if necessary.
TABLE 13-1 Recommended Suction Catheter French Sizes for Endotracheal and Tracheostomy Tubes*
| Age | Tube Internal Diameter (mm) | Size of Suction Catheter (Fr) |
|---|---|---|
| NEWBORN | ||
| 1,000 g | 2.5 | 5 |
| 1,000-2,000 g | 3 | 6 |
| 2,000-3,000 | 3.5 | 8 |
| 3,000 g to 6 mo | 3.5-4 | 8 |
| PEDIATRIC | ||
| 18 mo | 4 | 8 |
| 3 yr | 4.5 | 8 |
| 5 yr | 5 | 10 |
| 6 yr | 5.5 | 10 |
| 8 yr | 6 | 10 |
| ADULT | ||
| 16 yr | 7 | 10 |
| Normal-size woman | 7.5-8 | 12 |
| Normal-size man | 8-8.5 | 14 |
| Large adult | 9-10 | 16 |
(TT), the suction catheter’s one half the inner diameter of the ET or TT.
* For suctioning of endotracheal tubes (ET) and tracheostomy tubes
a. Calculations related to catheter size (math review)
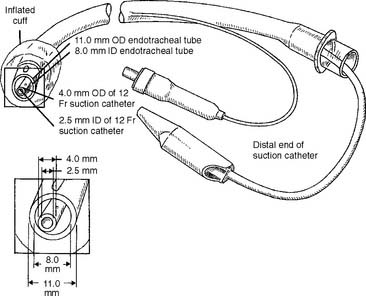
Suction catheter size (Fr) × 0.33=OD(mm) of suction catheter
Calculate the OD of a 12 Fr suction catheter:
This size catheter, therefore, could be used with an 8-mm ID endotracheal tube. Figure 13-3 shows the relative sizes of this endotracheal tube and catheter.
Calculate the largest suction catheter that should be used with a size 8 (ID) endotracheal tube:
Therefore, a 12 Fr suction catheter could be used with an 8-mm ID endotracheal (or tracheostomy) tube (see Figure 13-3).
b. Get the necessary equipment for the procedure
The term open-airway suctioning is used here to refer to a suctioning procedure on a patient who is spontaneously breathing room air after being disconnected from the source of supplemental oxygen. For example, in a patient with a normal upper airway, the oxygen mask is removed for nasotracheal suctioning. Also, in a patient with an endotracheal or a tracheostomy tube, the aerosol T-piece (Briggs adapter) or ventilator circuit is removed to allow suctioning.
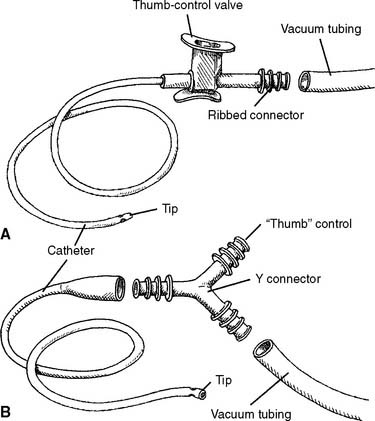
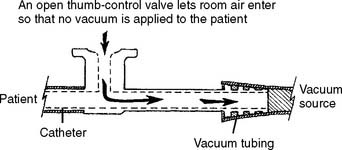
These types of catheters have been in use for many years. The two basic types are shown in Figure 13-4. Closing the thumb control, as shown in Figure 13-5, allows the vacuum to be selectively applied to the secretions when desired. The tips of the catheters can vary greatly. A considerable amount of effort has been spent trying to develop a catheter tip that most effectively removes secretions without damaging the tracheal mucosa. Figure 13-6 shows some of the catheter tips that have been developed to minimize mucosal damage. Note that all feature at least one opening in the catheter that is back from the opening at the tip. Compare this with the single end opening found on the oral suction catheter (see Figure 13-2). The side openings are designed to prevent the vacuum from being applied to the tip when it makes contact with the mucosa.
Notice in Figures 13-4 and 13-6 that most catheters are straight throughout their length. All of these catheters tend to enter the right mainstem bronchus during deep suctioning. This is because the right mainstem bronchus’s angle off of the trachea is less acute than that of the left mainstem bronchus. Therefore, it is difficult, if not impossible, to use any of these catheters to suction the left mainstem bronchus. The Coudé catheter has an angled tip to make it easier to guide into the left (or right) mainstem bronchus (see Figure 13-6, C). When these catheters are used, the direction of the thumb control valve can help determine the angle of the bent tip.
c. Get the necessary equipment for the procedure
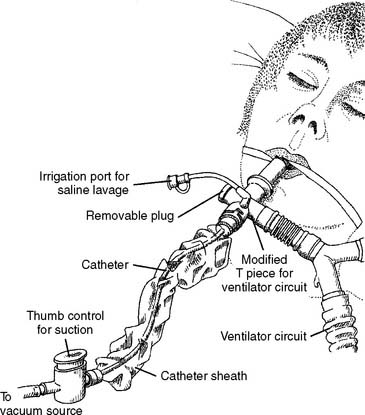
In closed-airway suctioning systems, a flexible, clear plastic sheath covers the catheter to maintain its sterility (Figure 13-7). The practitioner does not need gloves. When used for patients who need frequent suctioning, self-contained systems have a financial advantage over the traditional catheter and gloves suctioning method, because they can be reused. Closed-system suction catheters come with either the traditional straight tip or the Coudé tip for selective bronchial suctioning.
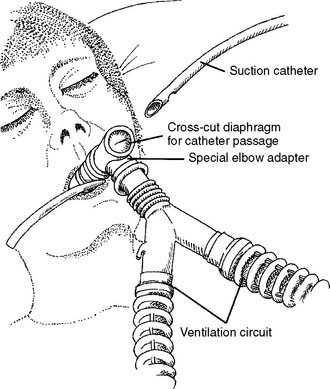
Another device used to create a sealed system for endotracheal tube suctioning consists of an elbow adapter that has an inner plastic sleeve or diaphragm. As the traditional catheter is inserted into the opening on the elbow adapter, the sleeve or diaphragm conforms to the catheter so that no air leakage occurs (Figure 13-8). This ensures that the ventilator-delivered volumes and pressures are not lost through a leak.
d. Put the equipment together andmake sure that it works properly
Figure 13-4 shows the attachment of an open-airway suction catheter to the vacuum tubing, and Figure 13-7 shows the attachment of a closed-airway suction catheter to the vacuum tubing. The other end of the vacuum tubing is attached to the vacuum regulator system.
While holding the body of the catheter, the thumb control valve, and the vacuum connector with the sterile-gloved hand and the vacuum tubing with the cleangloved hand, slip the vacuum tubing over the catheter’s vacuum connector. The seal should be tight so that no vacuum leak occurs. From now on, only the sterile-gloved hand may touch the part of the catheter that makes contact with the patient. The clean-gloved hand may touch only the thumb control valve and vacuum tubing. If the catheter is contaminated, it must be discarded.
3. Specimen collectors
a. Get the necessary equipment
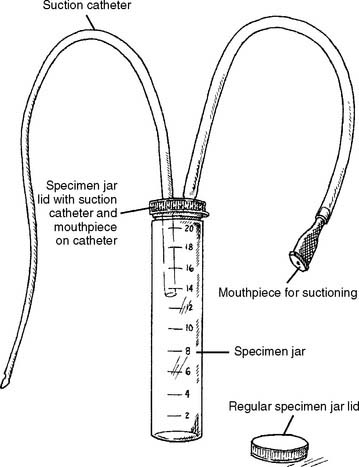
A variety of specimen collectors (commonly called Lukens traps) are available. They are packaged as sterile so that no contamination of the sputum sample occurs with nonpatient organisms. Figures 13-9 through 13-12 show the key features and functions of several sputum sample collectors. The sputum sample is obtained through a suction catheter or bronchoscope.
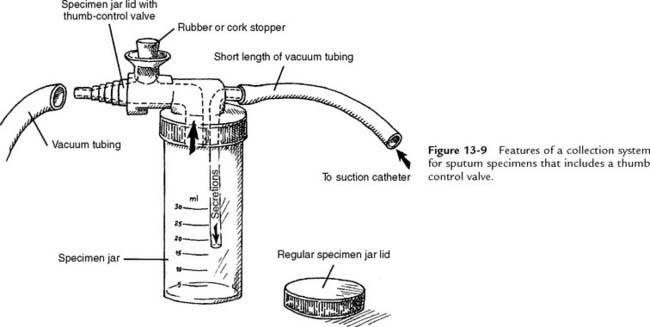
Figure 13-9 Features of a collection system for sputum specimens that includes a thumb control valve.
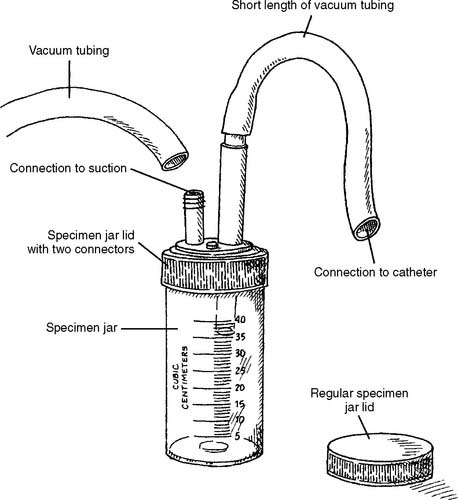
Figure 13-10 Features of a collection system for sputum specimens that does not have a thumb control valve.
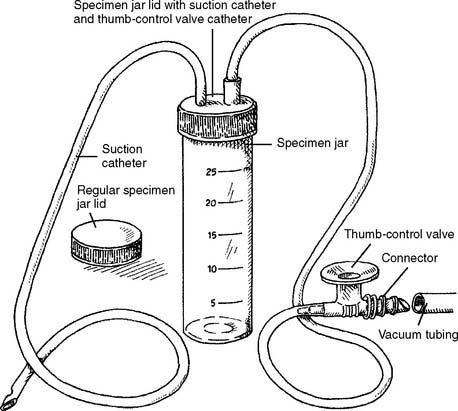
Figure 13-11 Features of a collection system for sputum specimens that has a thumb control valve built into catheter.
The specimen jar has volume markings. It screws into either a special lid used to suction the specimen or a regular lid. The regular lid is used for shipment to the laboratory. The special lids used in the systems featured in Figures 13-9 and 13-10 must be connected to a sterile catheter. Figure 13-11 shows a system with its own catheter. The vacuum source is provided to these specimen collectors by a length of vacuum tubing, as in the previously described suction catheter systems. Figure 13-12 shows a DeLee system, which is sometimes used in the delivery room. The physician, nurse, or practitioner uses mouth suction to remove secretions from the newborn. In all of these examples, after the sample has been collected, the special lid is unscrewed and replaced with the regular specimen jar lid.
MODULE B
1. Manipulate vacuum regulator systems by order or protocol (ELE Code: IIA21) [ELE Difficulty: R, Ap, An]
3. Put the equipment together and make sure that it works properly
a. Portable vacuum systems
Portable units are designed to be moved with the patient. They may be mounted on a small platform (Figure 13-13) or on a wheeled cart. The portable systems generally include an electrically powered vacuum pump with an ON/OFF switch and a collection bottle. Some units have a control valve for adjusting the level of negative pressure. A negative-pressure gauge is used to determine how much vacuum is being applied. A length of rubber vacuum tubing is used to pass the negative pressure from the pump to the collection bottle. Another length of vacuum tubing is used to pass the vacuum through to the suction catheter. Portable systems are not as powerful as central vacuum systems. They are not very effective at suctioning out large amounts of thick secretions.

Figure 13-13 Portable suction machine, showing the electrically powered motor, collection bottle and cap, and connecting tubing.
(Courtesy Allied Health Care Products, St Louis, Mo.)
In general, the following steps are followed to make the units operational:
b. Central vacuum systems
Central (wall) vacuum systems usually are available at each patient’s bedside in all special care units. Each of the wall outlets is connected through a hospital-wide piping system to a large, electrically powered vacuum pump. It is capable of generating a negative pressure far greater than that needed in most patient care situations. A regulator is used to reduce the vacuum to the desired clinical level (Figure 13-14). Either a Quick Connect or a Diameter Index Safety System (DISS) connector is used to attach the regulator to the central vacuum system.
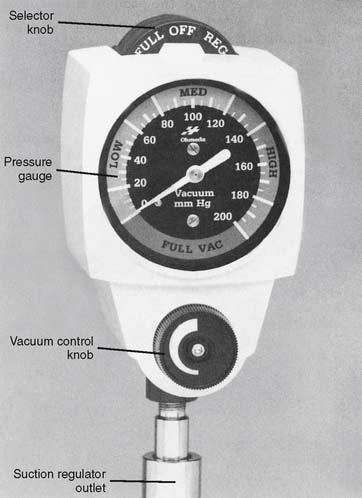
Figure 13-14 Features of the Ohmeda central vacuum regulator with a three-position selector knob.
(Courtesy Ohmeda Medical, Columbia, Md.)
In general, the following steps are followed to make the units operational:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree