18 Special Procedures
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will simply be shown as: (Code: …). If an item is only testable on the ELE, it will be shown as: (ELE code: …). If an item is only testable on the WRE, it will be shown as: (WRE code: …).
MODULE A
2. Participate in land or air patient transport outside of the hospital (Code: III I3a) [Difficulty: ELE: R; WRE: Ap, An]
3. Participate in the medical emergency team (MET) (e.g., rapid response team) (Code: III I3d) [Difficulty: ELE:R, WRE: Ap, An]
The first is airborne chemical exposure to the lungs and skin. This could include lung-damaging agents (e.g., ammonia, chlorine, and phosgene gases); blistering agents of the skin, eyes, and mucous membranes (e.g., sulfur mustard [mustard gas] and phosgene); blood agents that block oxygen’s metabolism (e.g., hydrogen cyanide and cyanogen chloride); and nerve agents that block the breakdown of acetylcholine (e.g., organophosphate pesticides). In all cases, the first action is to remove the victim from the toxic area. First responders must wear a hazardous materials suit to protect themselves before entering the toxic area to remove any victims. Once a victim is taken to a safe area, specific treatment is based upon the type of chemical exposure. Then the victim will receive other supportive measures such as supplemental oxygen, airway management, and mechanical ventilation.
Second is exposure to airborne infectious agents such as the viruses that cause avian flu and severe acute respiratory syndrome (SARS) or the spores that cause anthrax. In these cases the victim must be treated by caregivers who are wearing personal protective devices such as an N95 mask or a powered air protection respirator (PAPR). See Chapter 2 for the guidelines on airborne infection control precautions.
The third scenario would be trauma from explosion, gun fire, or train wreck, for example. The most severely injured victims would have trauma to the head, neck, chest, and/or abdomen. Many would require intubation and mechanical ventilation. Airway management and intubation are covered in Chapters 12 and 18; mechanical ventilation is covered in Chapters 15 and 16.
4. Participate in disaster management (Code: III I3c) [Difficulty: ELE:R, WRE: Ap, An]
MODULE B
1. Assist with moderate (conscious) sedation (Code: IIIJ7) [Difficulty: ELE: R, Ap; WRE: An]
Medications in the benzodiazepine group are preferred for conscious sedation and given intravenously. Currently midazolam (Versed) is preferred but diazepam (Valium) is also commonly used. When the patient’s procedure is completed, these medications can be reversed by intravenous flumazenil (Romazicon). Another option is to intravenously administer the narcotic agent fentanyl (Duragesic, Sublimaze) for rapid sedation. After the procedure is completed, naloxone (Narcan) is given intravenously to reverse the effects of fentanyl. There is more discussion of these and other sedative agents in Chapter 9, Pharmacology.
The respiratory therapist must be prepared for the possibility of the patient being overdosed with a sedative agent. This could result in a decreased respiratory rate and tidal volume or apnea. Safety guidelines require either a nurse or a respiratory therapist to monitor the patient’s breathing, pulse oximetry values, heart rate, blood pressure, and electrocardiogram. The therapist must be prepared to administer supplemental oxygen or begin bag-mask ventilation if needed.
2. Assist with the insertion of venous or arterial catheters (WRE code: IIIJ6) [Difficulty: WRE: An]
Chapter 5, Advanced Cardiopulmonary Monitoring, contains discussions on preparation, care, and maintenance of central venous, arterial, and pulmonary artery lines. Review the chapter if needed.
3. Assist with ultrasound (ELE code: IIIJ9) [Difficulty: ELE: R]
4. Assist with cardioversion (Code: IIIJ8) [Difficulty: ELE: R, Ap; WRE: An]
Cardioversion (or countershock) refers to deliberately sending a direct current (DC) electrical shock through the patient’s heart. Its purpose is to suppress an abnormal heartbeat so that the normal pacemaker at the sinoatrial (SA) node assumes control. This is accomplished if a great enough electrical current is sent through the chest wall to cause the depolarization of a critical mass of myocardial cells. After this, the SA node should take over as the pacemaker, provided that the heart muscle is oxygenated and not too acidotic. Two different types of cardioversion exist: defibrillation (also called unsynchronized cardioversion) and synchronized cardioversion. Both were introduced in Chapter 11 for the treatment of specific arrhythmias.
Defibrillation is performed in an emergency situation (see Figure 11-41). Patients who need to be defibrillated include those who have ventricular tachycardia or ventricular flutter (see Figures 11-38 and 11-39) when they are pulseless, unresponsive, or hypotensive or patients who have pulmonary edema and ventricular fibrillation (see Figure 11-40). Because the fastest possible action is needed, no attempt is made to synchronize the defibrillation shock with the heart’s rhythm. While cardiopulmonary resuscitation (CPR) is being performed, the defibrillator unit is prepared. The defibrillating paddles (large positive and negative electrodes) are placed on the patient’s right anterior and left lateral chest wall. The physician or other qualified person (respiratory therapist, registered nurse, or paramedic) performing the defibrillation should call out, “Stand clear.” All other medical personnel should stand back from the patient and the bed and not touch anything that is electrically grounded. When the buttons on the paddles are pushed, the shock is administered. If it is successful, the patient’s heartbeat returns to normal sinus rhythm. If the initial shock is unsuccessful, CPR is continued. The defibrillator is then recharged for another attempt as quickly as possible. Box 18-1 shows the sequence of increasingly more powerful countershocks that can be given.
BOX 18-1 Wattage Used in Synchronous Cardioversion and Defibrillation
Synchronized cardioversion is similar in some ways to defibrillation. An electrical shock is sent by two paddles through the heart to suppress paroxysmal atrial tachycardia, atrial flutter, atrial fibrillation, or hemodynamically stable ventricular tachycardia (see Figures 11-25, 11-26, and 11-27) so that the SA node assumes control. Its major difference from defibrillation is that the electrical shock is administered automatically by the defibrillator after an R wave is recognized by the electrocardiogram (ECG) monitor (see Figure 11-5). The ECG electrodes must be in place and the best lead (often lead II) selected to show a clear, strong, upright R wave. The defibrillator unit is programmed for synchronized cardioversion. The physician holds the paddles on the patient’s right anterior and left lateral chest wall. When the discharge buttons are pushed on the paddles, the shock is sent after the next R wave is identified by the ECG monitor.
The respiratory therapist’s role in cardioversion may include the following:
5. Bronchoscopy
Bronchoscopy is a procedure that involves looking directly into the patient’s tracheobronchial airways. The physician can perform a number of diagnostic and therapeutic tasks under direct vision. (See Box 18-2 for uses, limitations, and risks of bronchoscopy.)
BOX 18-2 Uses, Limitations, and Risks of Bronchoscopy
RIGID BRONCHOSCOPY
Therapeutic Uses
FIBEROPTIC BRONCHOSCOPY
Diagnostic Uses
a. Recommend a diagnostic bronchoscopy procedure to evaluate hemoptysis or atelectasis (Code: IC3) [Difficulty: ELE: R, Ap; WRE: An]
Hemoptysis commonly is caused by blunt chest trauma or a bleeding bronchial tumor. Segmental or lobar atelectasis is commonly caused by an aspirated foreign body or a bronchial tumor. As listed in Box 18-2, bronchoscopy can be used to help diagnose and manage these problems.
c. Assist with the bronchoscopy procedure (Code: IIIJ2) [Difficulty: ELE: R, Ap; WRE: An]
Typical duties of the respiratory therapist during bronchoscopy may include the following:
d. Manipulate a bronchoscope by order or protocol (Code: IIA27) [Difficulty: ELE: R; WRE: Ap, An]
1. Get a bronchoscope for the planned procedure
The rigid bronchoscope is a straight, hollow, stainless-steel tube (Figure 18-1). It has a distal light source so that the airway can be seen and a side port for providing oxygen or mechanical ventilation to the patient. The right and left mainstem bronchi can be observed by passing a mirror through the main channel. A hook or net can be passed through the main channel into the trachea or either bronchus to remove a foreign body. The rigid bronchoscope is preferred for the treatment of massive hemoptysis or to remove a foreign body.
Flexible fiberoptic bronchoscopy (FFB) uses a smaller diameter flexible tube with two sets of fiberoptic bundles that shine light into the airway and allow viewing of the airway. It has gained wide popularity because it is better tolerated by the patient and allows for better visualization and collection of specimens from smaller bronchi (Figures 18-2 and 18-3). The adult bronchoscopy tube is about 5- to 6-mm outer diameter (OD), and the pediatric tube is about 3-mm OD. The small diameter and ability to guide the catheter allow the operator to look into the bronchus to each lung segment (segmental bronchi). The fiberoptic bronchoscope is preferred over the rigid one when the patient is being mechanically ventilated or has disease or trauma to the skull, jaw, or cervical spine. As shown in Figure 18-2, a photo connection allows the assistant either to take still photographs of pulmonary anatomy or to videotape the entire procedure.
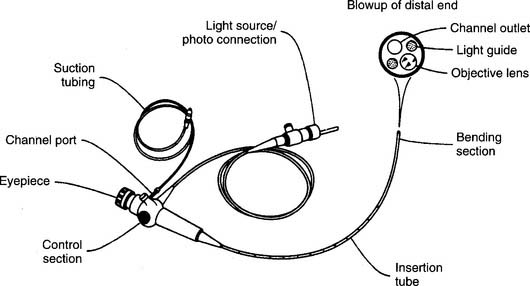
Figure 18-2 A flexible fiberoptic bronchoscope with its components and special features.
(From Wilkins RL, Stoller JK, Kacmarek RM: Egan’s fundamentals of respiratory care, ed 9, St Louis, 2009, Mosby.)
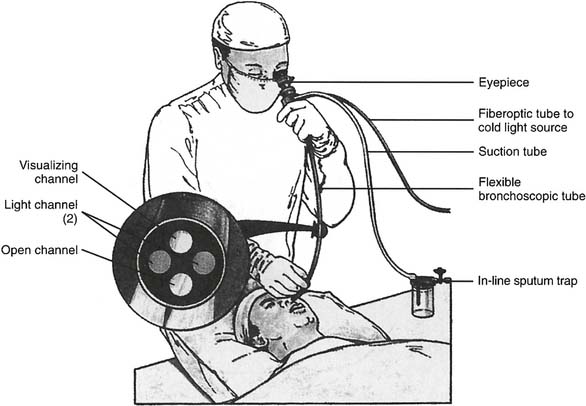
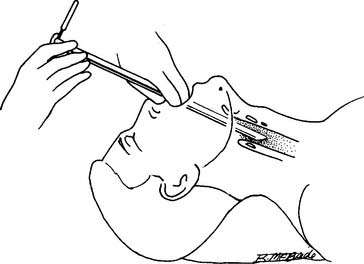
Figure 18-3 A flexible fiberoptic bronchoscopy procedure being performed on a patient.
(From Williams SF, Thompson JM: Respiratory disorders, St Louis, 1990, Mosby.)
2. Put the equipment together and make sure that it works properly
The fiberoptic bronchoscope is preassembled (see Figure 18-2 for its primary features). If photographing or videotaping is planned, the camera must be attached at the photo connection. Have a central or portable suctioning system set up with suction tubing. In addition, the following steps must be used to check for proper functioning:
6. Thoracentesis
a. Recommend a thoracentesis to treat a pleural effusion (WRE code: IC14) [Difficulty: WRE: R, Ap, An]
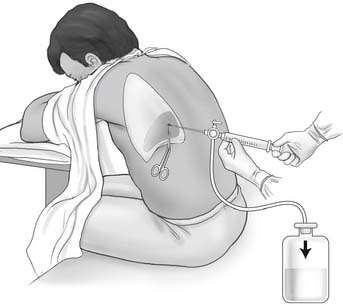
b. Assist with a thoracentesis procedure (Code: IIIJ3) [Difficulty: ELE: R, Ap; WRE: An]
General steps in the removal of pleural fluid:
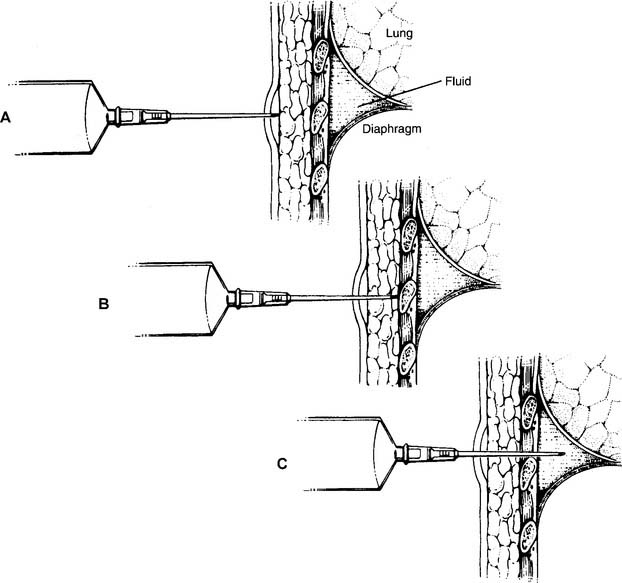
c. Assist with percutaneous needle aspiration biopsies of the lung
A pleural biopsy is indicated when exudative fluid is found during a thoracentesis procedure. The cause could be from an infection, including tuberculosis, or a lung tumor. Additionally, a pleural biopsy is indicated when a chest x-ray shows a pleural tumor or unexplained pleural thickening. A cutting needle is inserted into the parietal pleura to withdraw a specimen for analysis.
7. Management of a pneumothorax
a. Treat a tension pneumothorax (Code: III I2) [Difficulty: ELE: R, Ap; WRE: An]
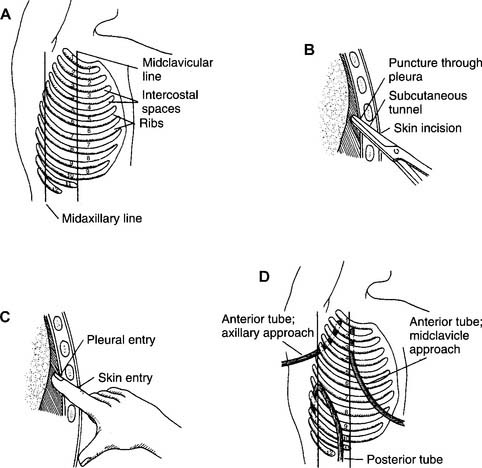
In an emergency when the patient has a tension pneumothorax and rapidly worsening vital signs, the trapped pleural air must be rapidly removed from the chest. This is done by inserting a large-bore needle (16 gauge or larger) through the second or third intercostal space in the midclavicular line of the affected lung. Place the needle over the top of the rib to avoid injury to the blood vessels and nerves below the ribs. The intrapleural air leaves the chest, allowing the lung to expand. A pleural chest tube is then inserted for a long-term solution to the problem. If necessary, review the discussion in Chapters 1 and 15 on the signs and symptoms of a pneumothorax.
b. Assist with chest tube insertion (Code: III J5) [Difficulty: ELE: R, Ap; WRE: An]
A chest tube (also called tube thoracostomy) may be inserted into either one or both pleural spaces around the lungs, the mediastinal space, or the pericardial space around the heart. This procedure is indicated when air or fluid, or both, in any of these spaces interferes with normal lung or heart function. Box 18-4 lists the indications for the insertion of a chest tube.
General steps in inserting a pleural chest tube follow:
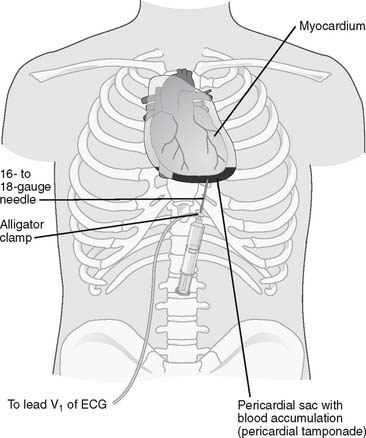
Figure 18-7 Pericardiocentesis procedure.
(From Black JM, Hawks JH: Medical-surgical nursing, clinical management for positive outcomes, ed 8, St Louis, 2009, Saunders.)
Every past examination has included at least one question that relates to identifying a patient having a tension pneumothorax, requiring the insertion of a large-bore needle or a pleural chest tube. Know the indications of a tension pneumothorax, including sudden deterioration of vital signs and hypoxemia, decreased breath sounds over the affected lung, decreased chest wall movement over the affected lung, hyperresonant percussion noted over the affected lung, and shift of the mediastinal structures away from the affected lung. See Figure 1-2 for a chest radiograph showing a pneumothorax.
c. Manipulate a pleural drainage system by order or protocol (ELE code: IIA21) [ELE difficulty: R, Ap, An]
2. Assemble a pleural drainage system, ensure that it works properly, and identify any problems with it
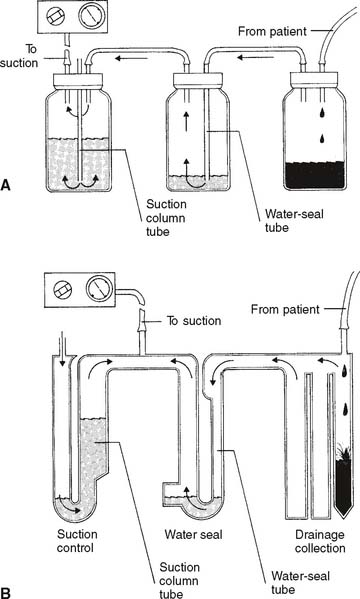
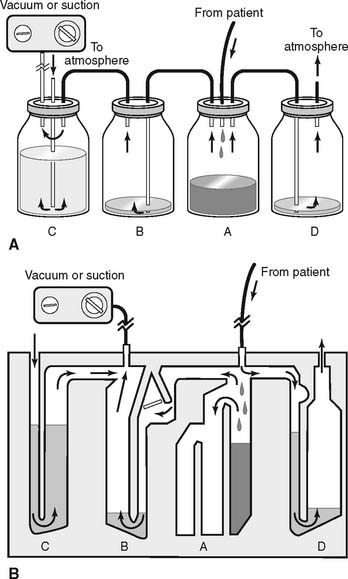
Refer to Figure 18-8 for the assembly and operation of the three-chamber drainage system. The four-chamber drainage system is shown in Figure 18-9 and is discussed concurrently.
a. Vacuum level.
The operation of the wall or central vacuum systems was discussed in Chapter 13. It is common practice to set a partial vacuum of −15 to −20 cm H2O pressure to the pleural space.
b. Suction control.
It is normal to have room air drawn into the opening on top and bubbling through the water column. This corresponds to bottle or chamber C in Figure 18-9. The constant air bubbling causes the water level to gradually decrease from evaporation. Water must be added occasionally.