STEMI Reperfusion (Primary PCI and Thrombolysis)
Vijay S. Ramanath MD, FACC
Craig A. Thompson MD
In this chapter, we will discuss the indications, contraindications, and techniques for both PCI and fibrinolysis (also known as thrombolytics) in the management of ST-segment elevation myocardial infarction (STEMI).
When deciding on the optimal reperfusion strategy for a patient presenting with STEMI, the following conditions must be considered: (a) time from onset of symptoms, (b) risk of STEMI as not all patients presenting with STEMI are at equal risk of death or other adverse outcomes, (c) risk of bleeding, and (d) time required to transport the patient to a skilled PCI laboratory. We will briefly touch upon each of these factors, followed by an in-depth discussion of the key points regarding PCI and fibrinolysis.
TIME FROM THE ONSET OF SYMPTOMS
Knowledge of the association between duration of coronary occlusion and infarct size dates back to the 1970s (1). Thus, time from symptom onset to reperfusion is a strong predictor of both MI size and clinical outcomes, whether thrombolytic therapy and/or PCI is employed. If thrombolytic therapy can be administered within the first 2 hours of symptom onset, the risk of mortality can be dramatically reduced. If primary PCI is performed, lesser durations from symptom onset to initial coronary balloon inflation have been associated with reduced mortality.
RISK OF STEMI
A number of predictive tools have been developed to aide clinicians in determining the risk of STEMI. For example, the widely embraced thrombolysis in myocardial infarction (TIMI) risk score for STEMI uses eight variables (age of ≥65 years, presence of CAD risk factors or angina, systolic blood pressure of <100, hazard ratio of >100, Killip class 2 to 4, weight <67 kg, anterior ST-segment elevation or new LBBB, and time to treatment) and has been shown to be predictive of 30-day mortality (2). Other risk models such as the GRACE scoring system employ additional variables such as serum creatinine in predicting in-hospital mortality up to 6 months (3).
RISK OF BLEEDING
The choice of reperfusion is also dependent on the patient’s risk of serious bleeding. Assuming that both fibrinolytics and percutaneous coronary intervention (PCI) are readily available should a patient’s risk of significant bleeding be considered high with fibrinolysis (e.g., patients older than 80 years), the decision for reperfusion therapy should favor PCI. If a PCI-capable facility is not readily accessible, then the risk-benefit ratio of fibrinolysis should be evaluated.
TIME NEEDED FOR TRANSPORT TO A PCI FACILITY
When a PCI facility is available within reasonable time (i.e., 90 minutes), this strategy should be strongly considered, as the data show superiority of PCI over thrombolytic therapy (discussed in detail below). However, in instances where transfer to a PCI facility is going to significantly delay coronary reperfusion, an initial strategy with thrombolytic therapy should be undertaken barring any contraindications.
PCI versus Thrombolytic Therapy
The advantage of thrombolytic therapy is its widespread availability and ease of administration. However, thrombolytic therapy fails to open the infarct-related artery in nearly one-fifth of cases and thus often provides incomplete reperfusion. In contrast, primary PCI has a high rate of reperfusion success, improved clinical outcomes, and few contraindications, but <25% of US hospitals have the means to perform primary PCI, and even fewer provide 24-hour coverage (4).
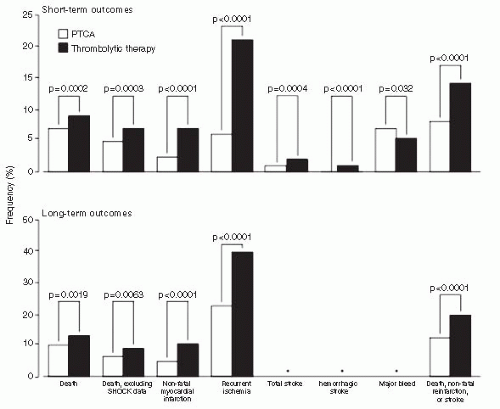
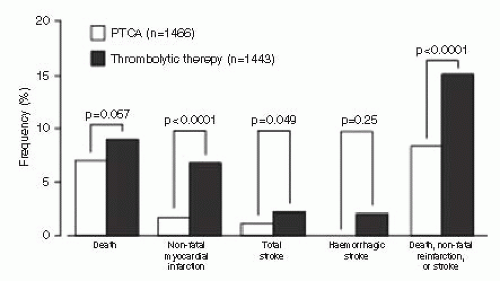
The Atlantic C-PORT trial randomized 450 patients from 11 community hospitals without on-site cardiac surgery to either thrombolytic therapy or primary PCI for acute myocardial infarction (MI) (5). The primary endpoint was the incidence of the composite of death, recurrent MI, or stroke 6 months after the index MI. Patients treated with primary PCI had a 42% reduction in the primary endpoint compared with those treated with thrombolytics. Women and the elderly had 50% and 40% reductions, respectively, in the primary endpoint as well. Interestingly, outcomes at low-volume centers (fewer than 1 primary PCI/month) had similar outcomes to thrombolytic therapy. Keeley et al. performed a large meta-analysis on 23 trials encompassing 7,700 patients randomized to percutaneous transluminal coronary angioplasty (PTCA) versus thrombolytic therapy (6). Nearly half of the trials invoked the use of coronary stenting and nearly one-third used platelet glycoprotein (GP) IIb/IIIa inhibitors. Only 3% of thrombolytic therapy patients crossed over to primary PTCA, while 0.6% randomized to PTCA crossed over to thrombolytic therapy. Short-term and longterm clinical outcomes are detailed in Figure 18-1. Patients receiving primary PTCA had fewer rates of short-term death (7% vs. 9%; p = 0.0002), nonfatal reinfarction (3% vs. 7%; p < 0.0001), stroke (1% vs. 2%; p = 0.0004), and the combined endpoint of death, nonfatal reinfarction, and stroke (8% vs. 14%; p < 0.0001). The significant reductions in death, nonfatal reinfarction, and the combined endpoint remained regardless of which thrombolytic agent was used. Five trials were analyzed, comparing on-site thrombolytic therapy to emergent transfer for primary PTCA. Despite the delays associated with patient transfer to a PCI facility (mean time, 39 minutes), primary PTCA was associated with significant reductions in nonfatal reinfarction, total stroke, and the combined endpoint (Fig. 18-2). In patients with cardiogenic shock, PCI appeared to have its greatest mortality benefit with an absolute 9% reduction in 30-day mortality, as reported in the SHOCK trial (7).
As the time delay for performing PCI increases, the clinical benefits associated with PCI over thrombolytics diminish (Fig. 18-3). This is particularly true in regard to mortality when delays are in excess of 60 minutes (8). In addition, the improved mortality benefit with PCI diminishes when PCI is performed in low-volume centers, where delays in door-to-balloon times are more likely to occur (9). Thrombolytic therapy is similarly limited in its efficacy as the duration from symptom onset to presentation increases, though a benefit still may be seen up to 18 hours of symptom onset (10, 11). Furthermore, there are a number of absolute and relative contraindications to thrombolytic therapy that the clinician must be mindful of before administering to a patient (Table 18-1). In contrast, a few contraindications exist for PCI such as patient refusal or when the patient’s risk for complication may be considered too high by the caring physician.
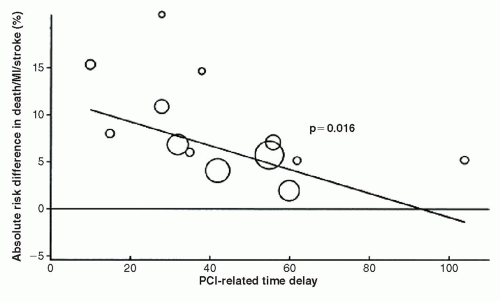 FIGURE 18-3 Absolute risk reduction in the 4 to 6 week combined endpoint of death, reinfarction, or stroke with primary PCI. (From: Nallamothu, et al. Am J Cardiol. 2003;97(7):824-826, with permission.) |
PCI AFTER FIBRINOLYSIS
PCI following fibrinolysis depends on PCI availability, type of triage, and transfer capabilities, as well as the pharmacologic therapy employed, and this approach has allowed the evolution of a number of terms including “facilitated” PCI, “rescue” PCI, and the “pharmacoinvasive” approach.
TABLE 18-1 Contraindications for Thrombolysis Use in STEMI | ||
|---|---|---|
|