Splenic Artery Aneurysm
TIMOTHY E. NEWHOOK, JOSHUA D. ADAMS, and GILBERT R. UPCHURCH Jr
Presentation
A 78-year-old grand multiparous woman with a past medical history significant for hypertension, aortic valve disease, Parkinson’s disease, and sigmoid diverticulosis presented to the emergency department with a 5-month history of abdominal pain. She described the pain as being throughout her epigastrium and radiating to her left lower abdominal quadrant. Her abdominal pain is sharp in character and intermittent since onset. Furthermore, her pain does not change with eating and nothing makes it better or worse. She denies any changes in bowel habits, appetite, chest pain, cough, back pain, or shortness of breath. Her medications included clopidogrel. Her social history was negative for alcohol or tobacco use. Review of systems was negative for any other pathology. On physical examination, vital signs were normal other than moderate hypertension. She was appropriate on questioning. A parkinsonian tremor was observed. A systolic ejection murmur was noted on auscultation, and her heart rate and rhythm were regular. Her abdomen was obese, soft, and mildly distended; however, she reported tenderness to palpation over her epigastrium and left upper quadrant. Despite this, no rebound tenderness or guarding was detected. She had two-plus pitting edema in her lower extremities.
Differential Diagnosis
This patient presents with a complex and nebulous history of present illness. The differential diagnosis for chronic abdominal pain in an elderly patient with a history of hypertension, cardiovascular disease, and diverticulosis is broad. Despite this, a conservative differential diagnosis must include abdominal aortic aneurysm; acute, chronic, or acute-on-chronic mesenteric ischemia; diverticulitis; nephrolithiasis; urinary tract infection; malignancy; median arcuate ligament syndrome; and visceral artery aneurysms.
Case Continued
A chest and abdominal x-ray series are performed, which demonstrate no abnormalities. Due to her presentation and comorbidities, a surgical consultation is requested. A computed tomography arteriogram (CTA) is performed. Furthermore, a complete blood count with differential is indicated to rule out other diagnoses, such as infection or lymphoma. The exams and labs are within normal limits, except that a 2-cm splenic artery aneurysm (SAA), that is nonruptured, is noted (Figs. 1 and 2).
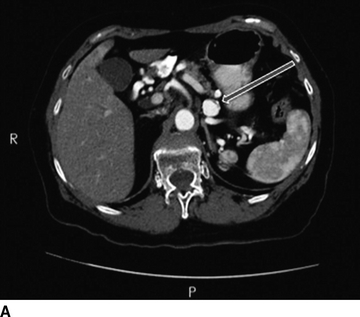
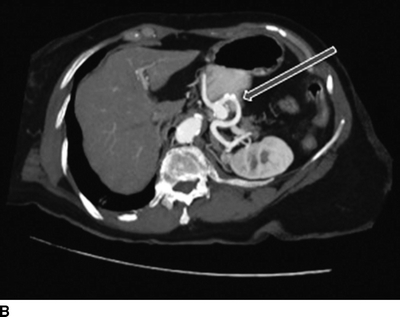
FIGURE 1 A,B: CTA abdomen and pelvis demonstrating no evidence of aortic aneurysm.The celiac, superior mesenteric, and inferior mesenteric arteries are all widely patent. Aortic bifurcation, common, internal, and external iliac as well as common femoral arteries are widely patent without evidence of aneurysm disease. No evidence of mesenteric ischemia is observed. A 2-cm SAA arising 4 cm distal to the origin of the splenic artery is noted adjacent to the mid-pancreatic body (arrows). Multiple noninflamed diverticula arise from the sigmoid colon. No other abnormalities are present.
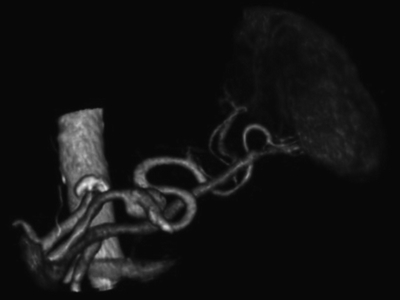
FIGURE 2 A three-dimensional reconstruction of the CTA revealing a 2-cm SAA arising 4 cm distal to the splenic artery origin.
Discussion
Aneurysms of the splenic artery are the most common aneurysm of the splanchnic arterial circulation. Specifically, SAAs account for approximately 60% of all splanchnic arterial aneurysms and are the third most common intra-abdominal arterial aneurysm behind infrarenal aortic and arterial aneurysms. Despite this, SAAs are relatively rare and often insidious with an estimated incidence of 0.8% in retrospective reviews of nonselective arteriograms. SAAs occur in women four times more frequently than men and typically within the sixth decade of life. Moreover, SAAs are frequently multiple and most often occur in the distal segment of the splenic artery.
SAAs are most often asymptomatic; however, patients presenting with vague epigastric or left upper quadrant abdominal pain radiating to the left scapula may attribute their symptoms to this entity. Physical examination rarely yields any remarkable findings. Abdominal x-ray may reveal a curvilinear signet-ring calcification in the left upper quadrant; however, most SAAs are found incidentally during imaging studies, such as CT, CTA, or magnetic resonance imaging (MRI) for other pathologies. SAAs have been associated with three major risk factors: pregnancy, systemic arterial dysplasia, and portal hypertension. In regard to pregnancy, the majority of females diagnosed with SAA are multiparous with a mean number of pregnancies being between 4 and 5 in multiple series. It is believed that SAA formation in this population may be due to increased splenic arterial flow occurring during pregnancy, as well as hormonal effects on arterial elastic tissue. Furthermore, many patients with renal artery fibrodysplasia also harbor SAA. Finally, 1% to 20% of patients with portal hypertension have SAA for reasons that are incompletely understood. Increased splenic arterial flow and hormonal imbalance increasing with end-stage cirrhosis may influence SAA formation in this population. Other factors that may contribute to SAA formation include pancreatitis, collagen vascular disease, atherosclerosis, and autoimmune disease (lupus).
SAAs have potential to rupture, which is often a lethal complication. Although rupture of SAA occurs in less than 2% of patients, it is imperative to recognize this as most SAA series report a high mortality after rupture. Patients believed to be at higher risk for SAA rupture include patients status post liver transplantation, women of childbearing age, pregnant women, and younger (less than 60 years) patients. SAA in a pregnant patient is of particular concern as rupture has been reported in over 90% of cases, resulting in a reported maternal mortality of almost 75% and fetal mortality over 95% of cases. Finally, SAA diameter greater than 2 cm is associated with a higher risk of rupture. In order to prevent rupture, it is recommended that all symptomatic SAAs be repaired, as well as asymptomatic pregnant women and women of childbearing age because of the aforementioned risk of rupture and associated mortality. Moreover, patients with SAA over 2 cm should be offered elective repair.
Recommendations
Given the patient’s presentation, risk factors, and subsequent radiologic studies, a diagnosis of symptomatic SAA is suspected. Therefore, a selective celiac arteriogram with consideration for endovascular repair is indicated.
Case Continued
After discussion of radiologic findings with the patient, consent was obtained to perform a selective celiac and splenic arteriogram with possible endovascular treatment of her SAA. The patient underwent intravenous conscious sedation and retrograde puncture of the right common femoral artery. First, the celiac artery was catheterized, and a selective celiac arteriogram was performed, after which a glidewire was utilized to catheterize the splenic artery. A selective splenic arteriogram was performed (Fig. 3A). A 2-cm saccular SAA was visualized arising from the inferior aspect of the mid-splenic artery, and the splenic artery was otherwise patent.
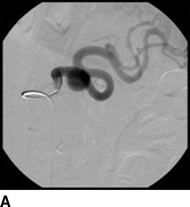




FIGURE 3 A: A selective splenic arteriogram was performed. A 2-cm saccular SAA was visualized arising from the inferior aspect of the mid–splenic artery, and the splenic artery was otherwise patent. B: A Rosen wire was placed beyond the SAA, followed by the advancement of a 10-French long sheath into the proximal splenic artery. C, D:An 8 mm × 40 mm covered stent was placed beyond the SAA and deployed, which successfully excluded the SAA. E: A post–stent placement arteriogram revealed that the SAA was completely excluded, the splenic artery remained fully patent, and perfusion of the spleen was preserved.



