6
Sleep EEG
Sleep is the state of natural rest observed in humans and animals, and even invertebrates such as the fruitfly Drosophila. It is an interesting and not perfectly known physiological phenomenon. The sleep state is one of the most important items of evidence for diagnosing mental disease. Sleep is characterized by a reduction in voluntary body movement, decreased reaction to external stimuli, an increased rate of anabolism (the synthesis of cell structures), and a decreased rate of catabolism (the breakdown of cell structures). Sleep is necessary and essential for the life of most creatures. The capability for arousal from sleep is a protective mechanism and also necessary for health and survival. Technically, sleep is different from unconsciousness [1].
Sleep is therefore defined as a state of unconsciousness from which a person can be aroused. In this state, the brain is relatively more responsive to internal stimuli than external stimuli. Sleep should be distinguished from coma. Coma is an unconscious state from which a person cannot be aroused.
Historically, sleep was thought to be a passive state. However, sleep is now known to be a dynamic process, and human brains are active during sleep. Sleep affects physical and mental health and the immune system.
States of brain activity during sleep and wakefulness result from different activating and inhibiting forces that are generated within the brain. Neurotransmitters (chemicals involved in nerve signalling) control whether some-one is asleep or awake by acting on nerve cells (neurons) in different parts of the brain. Neurons located in the brainstem actively cause sleep by inhibiting other parts of the brain that keep a person awake.
In humans, it has been demonstrated that the metabolic activity of the brain decreases significantly after 24 hours of sustained wakefulness. Sleep deprivation results in a decrease in body temperature, a decrease in immune system function as measured by a white blood cell count (the soldiers of the body), and a decrease in the release of growth hormone. Sleep deprivation can also cause increased heart rate variability [2].
Sleep is necessary for the brain to remain healthy. Sleep deprivation makes a person drowsy and unable to concentrate. It also leads to impairment of memory and physical performance and reduced ability to carry out mathematical calculations and other mental tasks. If sleep deprivation continues, hallucinations and mood swings may develop.
The release of growth hormone in children and young adults takes place during deep sleep. Most cells of the body show increased production and reduced breakdown of proteins during deep sleep. Sleep helps humans maintain optimal emotional and social functioning while we are awake by giving rest during sleep to the parts of the brain that control emotions and social interactions.
6.1 Stages of Sleep
Sleep is a dynamic process. Loomis provided the earliest detailed description of various stages of sleep in the mid-1930s, and in the early 1950s Aserinsky and Kleitman identified rapid eye movement (REM) sleep [1]. There are two distinct states that alternate in cycles and reflect differing levels of neuronal activity. Each state is characterized by a different type of EEG activity. Sleep consists of nonrapid eye movement (NREM) and REM sleep. NREM is further subdivided into four stages of I (drowsiness), II (light sleep), III (deep sleep), and IV (very deep sleep).
During the night the NREM and REM stages of sleep alternate. Stages I, II, III, and IV are followed by REM sleep. A complete sleep cycle, from the beginning of stage I to the end of REM sleep, usually takes about one and a half hours. However, generally, the ensuing sleep is relatively short and, for most practical purposes, a duration of 10–30 minutes suffices.
6.1.1 NREM Sleep
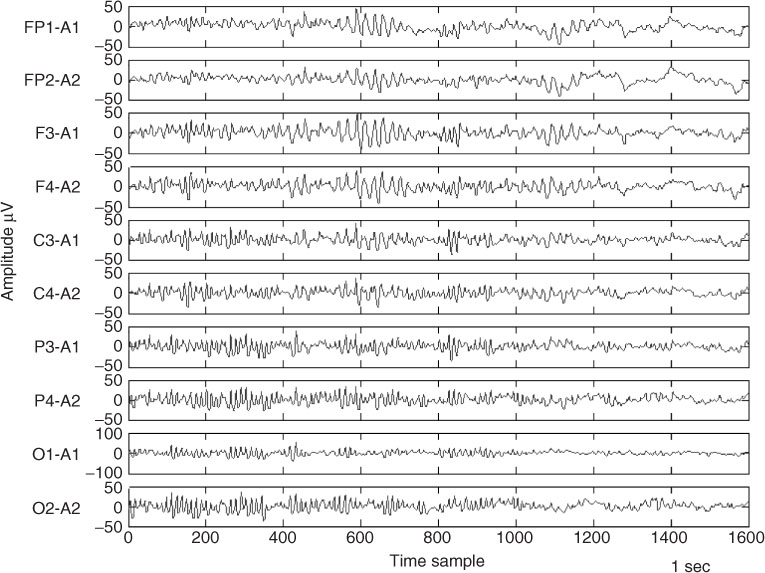
Stage I is the stage of drowsiness and very light sleep, and is considered a transition between wakefulness and sleep. During this stage, the muscles begin to relax. It occurs upon falling asleep and during brief arousal periods within sleep, and usually accounts for 5–10% of the total sleep time. An individual can be easily awakened during this stage. Drowsiness shows marked age-determined changes. Hypnagogic rhythmical 4–6 cycles/s theta activity of late infancy and early childhood is a significant characteristic of such ages. Later in childhood and, in several cases, in the declining years of life, the drowsiness onset involves larger amounts of slow activity mixed with the posterior alpha rhythm [3]. In adults, however, the onset of drowsiness is characterized by gradual or brisk alpha dropout [3]. The slow activity increases as the drowsiness becomes deeper. Other findings show that in light drowsiness the P300 response increases in latency and decreases in amplitude [4], and the inter- and intrahemispheric EEG coherence alter [5]. Figure 6.1 shows a set of EEG signals recorded during the state of drowsiness. The seizure-type activity within the signal is very clear.
Deep drowsiness involves the appearance of vertex waves. Before the appearance of the first spindle trains, vertex waves occur (the transition from stage I to II). These sharp waves are also known as parietal humps [6]. The vertex wave is a compound potential, a small spike discharge of positive polarity followed by a large negative wave, which is a typical discharge wave. It may occur as an isolated event with larger amplitude than that of normal EEG. In aged individuals they may become small, inconspicuous, and hardly visible. Another signal feature for deep drowsiness is the positive occipital sharp transients (POST) of sleep.
Spindles (also called sigma activity), the trains of barbiturate-induced beta activity, occur independently at approximately 18–25 cycles/s, predominantly in the frontal lobe of the brain. They may be identified as a ‘group of rhythmic waves characterized by progressively increasing, then gradually decreasing amplitude [3]. However, the use of middle electrodes shows a very definite maximum of the spindles over the vertex during the early stages of sleep.
Figure 6.1 Examplar EEG signals recorded during drowsiness
Stage II of sleep occurs throughout the sleep period and represents 40–50% of the total sleep time. During stage II, brain waves slow down with occasional bursts of rapid waves. Eye movement stops during this stage. Slow frequencies ranging from 0.7 to 4 cycles/s are usually predominant; their voltage is high, with a very prominent occipital peak in small children and gradually fall as age increases.
K-complexes appear in stage II and constitute a significant response to arousing stimuli. For topographical distribution over the brain, the K-complex shows a maximum over the vertex and has presence around the frontal midline [3]. For wave morphology, the K-complex consists of an initial sharp component, followed by a slow component that fuses with a superimposed fast component.
In stage III, delta waves begin to appear. They are interspersed with smaller, faster waves. Sleep spindles are still present at approximately 12–14 cycles/s but gradually disappear as the sleep becomes deeper.
In stage IV, delta waves are the primary waves recorded from the brain. Delta or slow wave sleep (SWS) usually is not seen during routine EEG [7]. However, it is seen during prolonged (>24 hours) EEG monitoring.
Stages III and IV are often distinguished from each other only by the percentage of delta activity. Together they represent up to 20% of total sleep time. During stages III and IV all eye and muscle movement ceases. It is difficult to wake up someone during these two stages. If someone is awakened during deep sleep, he or she does not adjust immediately and often feels groggy and disoriented for several minutes after waking up. Generally, analysis of EEG morphology during stage IV has been of less interest.
6.1.2 REM Sleep
REM sleep including 20–25% of the total sleep follows NREM sleep and occurs 4–5 times during a normal 8–9 hour sleep period. The first REM period of the night may be less than 10 minutes in duration, while the last period may exceed 60 minutes.
In an extremely sleepy individual, the duration of each bout of REM sleep is very short or it may even be absent. REM sleep is usually associated with dreaming. During REM sleep, the eyeballs move rapidly, the heart rate and breathing become rapid and irregular, blood pressure rises, and there is loss of muscle tone (paralysis), i.e. the muscles of the body are virtually paralysed. The brain is highly active during REM sleep, and the overall brain metabolism may be increased by as much as 20%. The EEG activity recorded in the brain during REM sleep is similar to that recorded during wakefulness.
In a patient with REM sleep behaviour disorder (RBD), the paralysis is incomplete or absent, allowing the person to act out dreams, which can be vivid, intense, and violent. These dream-acting behaviours include talking, yelling, punching, kicking, sitting, jumping from the bed, arm flailing, and grabbing. Although the RBD may occur in association with different degenerative neurological conditions the main cause is still unknown.
Evaluation of REM sleep involves a long waiting period since the first phase of REM does not appear before 60–90 minutes after the start of sleep. The EEG in the REM stage shows low voltage activity with a slower rate of alpha.
6.2 The Influence of Circadian Rhythms
Biological variations that occur in the course of 24 hours are called circadian rhythms. Circadian rhythms are controlled by the biological clock of the body. Many bodily functions follow the biologic clock, but sleep and wakefulness comprise the most important circadian rhythm. The circadian sleep rhythm is one of several body rhythms modulated by the hypothalamus (a part of the brain as shown in Chapter 2).
Light directly affects the circadian sleep rhythm. Light is called zeitgeber, a German word meaning time-giver, because it sets the biological clock.
Body temperature cycles are also under the control of the hypothalamus. An increase in body temperature is seen during the course of the day and a decrease is observed during the night. The temperature peaks and troughs are thought to mirror the sleep rhythm. People who are alert late in the evening (i.e. evening types) have body temperature peaks late in the evening, while those who find themselves most alert early in the morning (i.e. morning types) have body temperature peaks early in the morning.
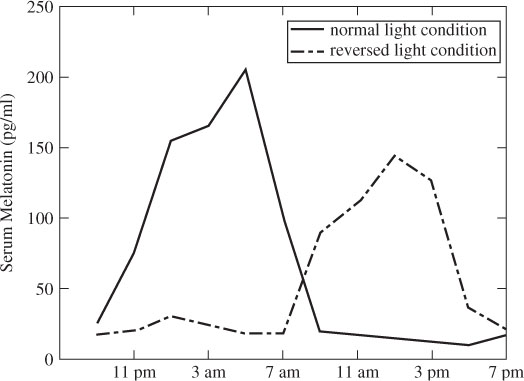
Melatonin (a chemical produced by the pineal gland in the brain and a hormone associated with sleep) has been implicated as a modulator of light entrainment. It is secreted maximally during the night. Prolactin, testosterone, and growth hormone also demonstrate circadian rhythms, with maximal secretion during the night. Figure 6.2 shows a typical concentration of melatonin in a healthy adult man.
Figure 6.2 A typical concentration of melatonin in a healthy adult man. (Extracted from Reference [8])
Sleep and wakefulness are influenced by different neurotransmitters in the brain. Some substances can change the balance of these neurotransmitters and affect sleep and wakefulness. Caffeinated drinks (for example coffee) and medicines (for example diet pills) stimulate some parts of the brain and can cause difficulty in falling asleep. Many drugs prescribed for the treatment of depression suppress REM sleep.
People who smoke heavily often sleep very lightly and have reduced duration of REM sleep. Heavy smokers tend to wake up after three or four hours of sleep due to nicotine withdrawal.
Some people who have insomnia may use alcohol. Even though alcohol may help people to fall into a light sleep, it deprives them of REM sleep and the deeper and more restorative stages of sleep. Alcohol keeps them in the lighter stages of sleep from which they can be awakened easily. During REM sleep, some of the ability to regulate body temperature is lost. Therefore, abnormally hot or cold temperatures can disrupt our sleep. If REM sleep is disturbed, the normal sleep cycle progression is affected during the next sleeping time, and there is a possibility of slipping directly into REM sleep and going through long periods of REM sleep until the duration of REM sleep that is lost is caught up.
Generally, sleep disruption by any cause can be a reason for an increase in seizure frequency or severity. It can also have a negative effect on short-term memory, concentration, and mood. Seizure, itself, during the night can disrupt sleep and using any anticonvulsant drug may affect sleep in different ways. Both the frequency of seizure and the locality of seizure sources within the brain may change in different sleep stages and wakefulness.
6.3 Sleep Deprivation
Sleep deprivation is evaluated in terms of the tasks impaired and the average duration. In tasks requiring judgement, increasingly risky behaviours emerge as the total sleep duration is limited to five hours per night. The high cost of an action is seemingly ignored as the sleep-deprived person focuses on limited benefits. These findings can be explained by the fact that metabolism in the prefrontal and parietal associational areas of the brain decrease in individuals deprived of sleep for 24 hours. These areas of the brain are important for judgement, impulse control, attention, and visual association.
Sleep deprivation is a relative concept. Small amounts of sleep loss (for example one hour per night over many nights) produce subtle cognitive impairment, which may go unrecognized. More severe restriction of sleep for a week leads to profound cognitive deficits, which may also go unrecognized by the individual. If you feel drowsy during the day, fall asleep for very short periods of time (5 minutes or so), or regularly fall asleep immediately after lying down, you are probably sleep-deprived.
Many studies have made it clear that sleep deprivation is dangerous. With decreased sleep, higher-order cognitive tasks are impaired early and disproportionately. On tasks used for testing coordination, sleep-deprived people perform as poorly as or worse than people who are intoxicated. Total sleep duration of seven hours per night over one week has resulted in decreased speed in tasks of both simple reaction time and more demanding computer-generated mathematical problem solving. Total sleep duration of five hours per night over one week shows both a decrease in speed and the beginning of accuracy failure.
Using sleep deprivation for detection and diagnosis of some brain abnormalities has been reported by some researchers [9–11]. It consists of sleep loss for 24–26 hours. This was used by Klingler et al. [12] to detect the epileptic discharges that could otherwise be missed. Based on these studies it has also been concluded that sleep depravation is a genuine activation method [13]. Its efficacy in provoking abnormal EEG discharges is not due to drowsiness. Using the information in stage III of sleep, the focal and generalized seizure may be classified [14].
6.4 Psychological Effects
Sleep measurements and studies are often polygraphically oriented and use EEG in combination with a variety of other physiological parameters. EEG studies have documented abnormalities in sleep patterns in psychiatric patients with suicidal behaviour, including longer sleep latency, increased rapid eye movement (REM) time and increased phasic REM activity. Sabo et al. [15] compared sleep EEG characteristics of adult depressives with and without a history of suicide attempts and noted that those who attempted suicide had consistently more REM time and phasic activity in the second REM period but less delta wave counts in the fourth non-REM period. Another study [16] conducted at the same laboratory replicated the findings with psychotic patients. On the basis of two studies, the authors [16] suggested that the association between REM sleep and suicidality may cut across diagnostic boundaries and that sleep EEG changes may have a predictive value for future suicidal behaviour. REM sleep changes were later replicated by other studies in suicidal schizophrenia [17] and depression [18].
Three cross-sectional studies examined the relationship between sleep EEG and suicidality in depressed adolescents. Dahl et al. [19] compared sleep EEG between a depressed suicidal group, a depressed nonsuicidal group, and normal controls. Their results indicated that suicidal depressed patients had significantly prolonged sleep latency and increased REM phasic activity, with a trend for reduced REM latency compared to both nonsuicidal depressed and control groups. Goetz et al. [20] and McCracken et al. [21] replicated the finding of greater REM density among depressive suicidal adolescents.
Study of normal ageing and transient cognitive disorders in the elderly has also shown that the most frequent abnormality in the EEG of elderly subjects is slowing of alpha frequency whereas most healthy individuals maintain alpha activity within 9–11 Hz [22,23].
6.5 Detection and Monitoring of Brain Abnormalities During Sleep by EEG Analysis
EEG provides important and unique information about the sleeping brain. Polysomnography (PSG) has been the well-established method of sleep analysis and the main diagnostic tool in sleep medicine, which interprets the sleep signal macrostructure based on the criteria explained by Rechtschaffen and Kales (R&K) [24]. The spindles and slow-wave activities, arousals, and associated activities are detected from the EEG signals and monitored during sleep. The description of these activities relies on the division of the temporal domain signals into fixed segments of 20–30 seconds. For analysis and monitoring of sleep disorders the main stage is detection of the waveforms during different stages of sleep. A good example is diagnosis of sleep apnea syndrome (SAS), described in the following section.
6.5.1 Detection of the Rhythmic Waveforms and Spindles Incorporating Blind Source Separation
SAS with a high prevalence of approximately 2% in women and 4% in men between the ages of 30 to 60 years is the cause of many road accidents [16,25]. This syndrome is often treated by means of continuous positive airway pressure therapy or by surgery. An early diagnosis of the disease is important since adequate treatment can be provided. Diagnosis of this disease is normally by standard PSG techniques with overnight recordings of sleep stage, respiratory efforts, oronasal airflow, electrocardiographic findings, and oxyhemoglobin saturation parameters in an attended laboratory setting [17]. In order to facilitate recording of the EEGs during sleep with a small number of electrodes a method to best select the electrode positions and separate the ECG, EOG, and EMG has been proposed [18].
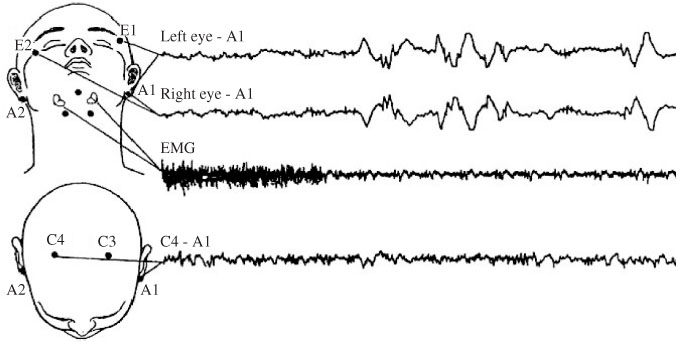
In this work, in order to investigate adequately the sleep signals and establish a night sleep profile, the electrophysiological activities manifested within the above signals have to be studied. Therefore a number of recording channels are needed and the signals have to be separately archived [26]. For the EEG the signals from C4-A1 or C3-A2 are used. For eye movement (EOG) two temporal electrodes located near each eye (E1 and E2), slightly moved relative to the median plain, are used so that horizontal and vertical eye movements relative to the same electrode A1 (or A2) located on the mastoids can be simultaneously observed. Muscular activity is obtained by processing two electrodes located on the chin.
Figure 6.3 The configuration for sleep EEG recording proposed in Reference [18]. The position of the C3 and C4 electrodes is based on the conventional 10–20 EEG electrode positions. Reproduced with permission from Porée, F., Kachenoura, A., Gavrit, H., Morvan, C., Garrault, G., and Senhadji, L., ‘Blind source separation for ambulatory sleep recording’, IEEE Trans. Information Technol. Biomed., 10(2), 2006, 293–301. © 2006 IEEE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


