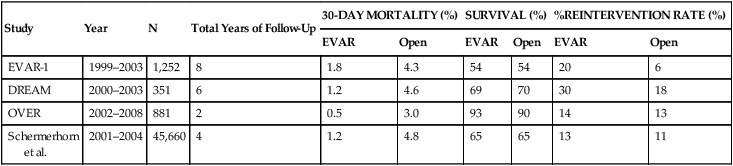
Over the years, hundreds of studies have been published reporting outcomes of open and endovascular aneurysm repair. However, only recently several long-term randomized, comparative trials have been reported. Before the publication of these studies, there was significant concern that late complications of EVAR would lead to substantial late mortality and perhaps long-term outcomes that are unfavorable compared to those of open repair. A summary of the findings of the most significant of these recent reports follows and is shown in Table 1. TABLE 1 Sentinel Trials of Open Surgical Repair versus Endovascular Repair to Treat Large Abdominal Aortic Aneurysm∗
Selection of Patients with Aortic Aneurysms for Open Surgical or Endovascular Repair
Open Versus Endovascular Aneurysm Repair: The Data
Study
Year
N
Total Years of Follow-Up
30-DAY MORTALITY (%)
SURVIVAL (%)
%REINTERVENTION RATE (%)
EVAR
Open
EVAR
Open
EVAR
Open
EVAR-1
1999–2003
1,252
8
1.8
4.3
54
54
20
6
DREAM
2000–2003
351
6
1.2
4.6
69
70
30
18
OVER
2002–2008
881
2
0.5
3.0
93
90
14
13
Schermerhorn
et al.
2001–2004
45,660
4
1.2
4.8
65
65
13
11
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
