Chapter 106 Segmental Anatomy
SEGMENTAL SETS OR COMBINATIONS
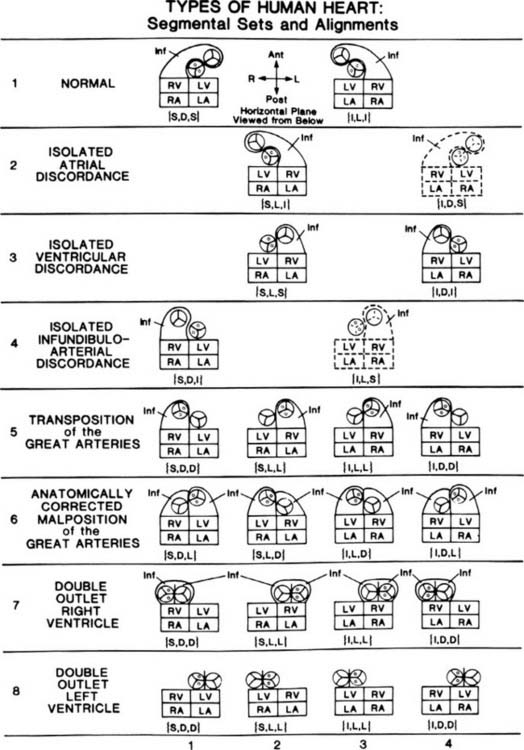
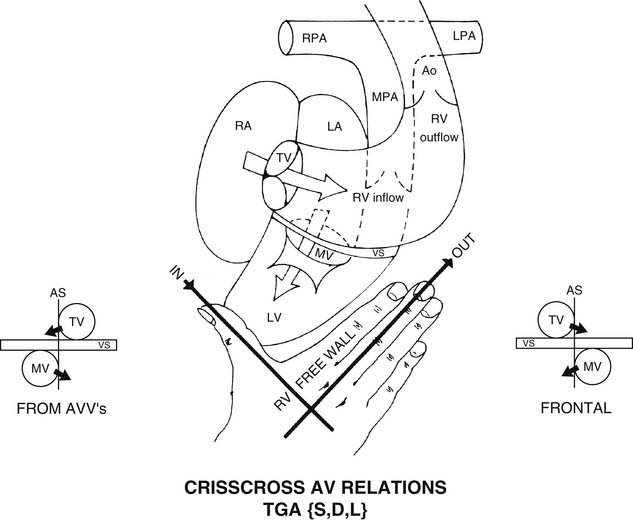
The cardiac segments are the anatomic and developmental building blocks out of which all human hearts, normal and abnormal, are made.1–8 The three main cardiac segments are the atria, the ventricles, and the great arteries (Fig. 106-1). The two connecting cardiac segments are the atrioventricular canal or junction, and the infundibulum, or conus arteriosus (see Fig. 106-8). Understanding segmental anatomy1 requires an understanding of morphologic anatomy3: the anatomic features of the morphologically right atrium (RA) (Fig. 106-2), of the morphologically left atrium (LA) (Fig. 106-3), of the morphologically right ventricle (RV) (Fig. 106-4), and of the morphologically left ventricle (LV) (Fig. 106-5). As Figure 106-1 illustrates, the morphologically RA, LA, RV, and LV can positionally be anywhere. A combination of morphologic anatomy and segmental anatomy is the basis of accurate diagnosis in congenital heart disease (see Fig. 106-1), which in turn is basic to successful open-heart surgery.
Figure 106–3 Morphologically left atrium (LA). A, Exterior. B, Interior. In A, the left atrial appendage (LAA) is relatively long and thin, like a pointing finger. It is also small and posterior, compared with the right atrial appendage (RAA). Normally, the LAA is not incorporated into the main cavity of the LA, whereas the RAA is incorporated to a major degree into the main cavity of the RA. The pulmonary veins (PV) normally connect with the LA; however, abnormally, the PV do not return to the LA, as in totally anomalous pulmonary venous connection. Hence, the pulmonary veins are not a highly reliable diagnostic marker of the LA. To our knowledge, the IVC never connects directly with the LA. Rarely, the IVC can connect with the left sinus horn (an enlarged coronary sinus [CoS]), and if a coronary sinus septal defect coexists, unroofing the CoS, then the bloodstream of the IVC can flow into the LA. However, note that the IVC connects with the left sinus horn, not with the LA directly. In B, note that septum primum (Sept I) normally is the dominant morphologic feature of the LA’s septal surface. Septum secundum (Sept II) is partly covered by the more leftward Sept I. The pectinate muscles of the LA are largely confined to the small fingerlike LAA and do not normally extend out into the main cavity of the LA. Consequently, the pectinate muscles of the LA do not approach the mitral valve (MV), whereas the pectinate muscles of the RA closely approach the tricuspid valve (see Fig. 106-2B). This characteristic difference in distribution of papillary muscles in the LA compared with the RA reflects the different degrees of incorporation of the atrial appendages and their pectinate muscles into the main chamber: in the LA, pectinate incorporation is minimal; in the RA, pectinate incorporation is maximal. Differing degrees of incorporation of the atrial appendages are reflected by differing pectinate patterns; this understanding is important in the heterotaxy syndromes with asplenia and polysplenia.
(From Van Praagh R, Vlad P. Dextrocardia, mesocardia, and levocardia: the segmental approach to diagnosis in congenital heart disease. In: Keith JD, Rowe RD, Vlad P, editors. Heart disease in infancy and childhood. 3rd ed. New York: Macmillan; 1978, p. 638-95.)
Figure 106–5 Morphologically left ventricle (LV). A, Exterior, drawing. B, Interior drawing. C, Interior, photograph. In A, note that the external shape of the LV is conical, like a bullet or a torpedo. The lateral margin of the LV is described as the obtuse margin because it forms an angle of more than 90 degrees (as opposed to the acute margin of the right ventricle, Fig. 106-4A). The anterior descending (AD) coronary artery and the posterior descending coronary artery (not seen) externally indicate the location of the ventricular septum. The diagonal (D) branches of the left coronary artery, also known as the obtuse marginal branches, externally indicate the locations of the left ventricular papillary muscles. The superior diagonal supplies the region of the anterolateral (AL) papillary muscle group and the adjacent LV free wall. The inferior diagonal supplies the region of the posteromedial papillary (PP) muscle group and the adjacent LV free wall. Also seen are the characteristic external shape of the left atrium (LA), the leftward and anterior location of the normally arising main pulmonary artery (PA), and the more rightward and posteroinferior location of the normally originating ascending aorta (Ao). In B and C, the noncoronary (NC) and left coronary (LC) leaflets of the aortic valve are in direct fibrous continuity with the anterior leaflet of the mitral valve (AL of MV), reflecting the normal absence of the subaortic conal free-wall myocardium. The anterosuperior portion of the left ventricular septal (S) surface is smooth or nontrabeculated. The inferior and apical portions of the left ventricular septal and free-wall (FW) surfaces are characterized by a lattice-like mesh of small, fine, oblique trabeculae carneae (very different from the coarse, few, straight trabeculations of the RV). The ostia of the right coronary (RC) and LC arteries are seen in their respective sinuses of Valsalva. The noncoronary–left coronary commissure normally is located above the middle of the anterior mitral leaflet. The noncoronary–right coronary commissure normally is located above the membranous septum, which in turn is immediately above the left bundle of the atrioventricular (AV) conduction system.
(From Van Praagh R, Vlad P. Dextrocardia, mesocardia, and levocardia: the segmental approach to diagnosis in congenital heart disease. In: Keith JD, Rowe RD, Vlad P, editors. Heart disease in infancy and childhood.3rd ed. New York: Macmillan; 1978, p. 638-95.)
For each type of heart (see Fig. 106-1), the atria, ventricles, and great arteries may be regarded as the members of a set or combination: {atria, ventricles, great arteries}. Braces {} are a mathematical symbol meaning “the set of.” The main cardiac segments are the members of a segmental set or combination. Each segmental set is recorded in venoarterial sequence, {atria, ventricles, great arteries}, this being the natural or blood-flow order.
MORPHOLOGIC ANATOMY
Beginning with the atria, two types of visceroatrial situs are shown in Figure 106-1.9 Situs means the pattern of anatomic organization. We speak of visceroatrial situs because the situs of the viscera and the situs of the atria are almost always the same. The two types of visceroatrial situs (see Fig. 106-1) are (1) situs solitus, the usual, ordinary, customary situs—hence the normal; and (2) situs inversus, a mirror-image of situs solitus. In a mirror image, there is right–left reversal without anteroposterior or superoinferior change. Visceroatrial situs solitus and situs inversus are stereoisomers.
A third possibility is situs ambiguus,3,10–12 the uncertain or indeterminate type of visceroatrial situs that may characterize the heterotaxy syndromes with asplenia, with polysplenia, or with a normally formed but often right-sided spleen. Visceroatrial situs ambiguus, which can occur with these anomalies of laterality—the heterotaxy syndromes,12 is not regarded as a specific type of visceroatrial situs. Instead, situs ambiguus appears to be a scrambled form either of visceroatrial situs solitus or of visceroatrial situs inversus. As noted earlier, this is why there appear to be only two types of visceroatrial situs: solitus and inversus (see Fig. 106-1).
It should be understood that the concepts of atrial isomerism and atrial appendage isomerism are considered to be erroneous.12,13 To be accurate, atrial isomerism has never been documented—neither bilateral RA, with bilateral inferior venae cavae, bilateral superior venae cavae, bilateral coronary sinus ostia, bilateral septa secunda, and bilateral broad triangular appendages; nor bilateral LA with bilateral pulmonary veins, bilateral septa prima, and bilateral fingerlike appendages.
Similarly, isomerism of parts of the atria, such as isomerism of the pectinate muscles (only), is regarded as a contradiction in terms.13 Isomerism applies to a whole structure, not just to a few of its parts. For example, the molecules D-glucose and L-glucose would not be regarded as isomers if only some of the hydroxyl groups, or some of the hydrogen atoms, or only the carboxyl groups were mirror images but nothing else was. Thus, pectinate isomerism is considered to be an erroneous concept because isomerism applies to whole structures, such as the RA and the LA, not just to parts of a structure, such as the pectinate muscles.
The realization that atrial-level isomerism is an erroneous concept facilitates the diagnosis of atrial situs, even in the heterotaxy syndromes.12 However, when atrial situs cannot be diagnosed with confidence, we make the diagnosis of atrial situs ambiguus, meaning that the atrial situs is undiagnosed, but without the implication that atrial-level isomerism is present.
In visceroatrial situs solitus, symbolized as {S,-,-} (see Fig. 106-1, columns 1 and 2), the RA (see Fig. 106-2) is right-sided and the LA (see Fig. 106-3) is left-sided. In visceroatrial situs inversus, symbolized as {I,-,-} (see Fig. 106-1, columns 3 and 4), the mirror-image RA is left-sided and the mirror-image LA is right-sided.
There are two types of ventricular situs (isomeric patterns of anatomic organization): D-loop ventricles (see Fig. 106-1, columns 1 and 4) and L-loop ventricles (see Fig. 106-1, columns 2 and 3). D-loop ventricles are solitus or noninverted ventricles that are normally associated with dextral or rightward looping of the straight heart tube, placing the RV (see Fig. 106-4) to the right of the LV (see Fig. 106-5). L-loop ventricles are inverted or mirror-image ventricles that are typically associated with levo or leftward looping of the straight heart tube, placing the mirror-image RV to the left of the mirror-image LV.
CHIRALITY OR HANDEDNESS
The D-loop, or solitus RV, is right-handed (Fig. 106-6).14 Figuratively speaking, the thumb of the right hand goes through the tricuspid valve. The fingers of the right hand go into the RV outflow tract. The palm of only the right hand faces the RV septal surface. The dorsum of only the right hand faces the RV free-wall surface.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree