Saphenous Vein Ablation and Stab Phlebectomy
Kathleen J. Ozsvath
Stephanie S. Saltzberg
Varicose Veins and Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) affects millions of people in this country and worldwide. In a study of 1,566 patients, the prevalence of CVI was found to be 9% in men and 7% in women. The presence of symptoms are correlated with the severity of CVI, impacting the quality of life in affected patients. Patient complaints include asymptomatic telangiectasias, unsightly, bulging varicose veins, complaints of pain, swelling, skin changes, and discoloration. In the worst cases, patients may develop skin ulceration seen in 0.3% of the adult populations. It is estimated that up to one billion dollars are spent on wound care in patients with venous ulcers. Affected patients suffer from loss of work hours due to frequent wound care treatments. These patients can feel stigmatized socially because of complicated dressings and malodorous wounds. A classification system used to define the severity of venous disease was developed and published called the CEAP (clinical, etiologic, anatomic, pathophysiologic) classification. This classification system allows clinicians to summarize and standardize the severity of venous disease in patients. Furthermore, treatment options and algorithms have been defined based on the CEAP classificiation.
Venous insufficiency is a complex problem thought to be due to a combination of diseased connective tissue synthesis, venous hypertension, inflammation, and valvular damage or failure. Affected veins become engorged leading to swelling and inflammation. Both superficial and deep veins can be involved. The deep veins are found within the muscular compartments of the lower extremities. The superficial veins include the axial veins found in the subcutaneous tissue located above the muscle fascia: Greater and small saphenous veins and their associated tributaries. Veins connecting the superficial and deep systems are referred to as perforating veins. These veins can also become incompetent leading to further pooling of blood in the superficial tissue above the muscle fascia. Risk factors associated with venous incompetence include obesity, ambulatory occupations, history of phlebitis, history of pregnancy, and family history.
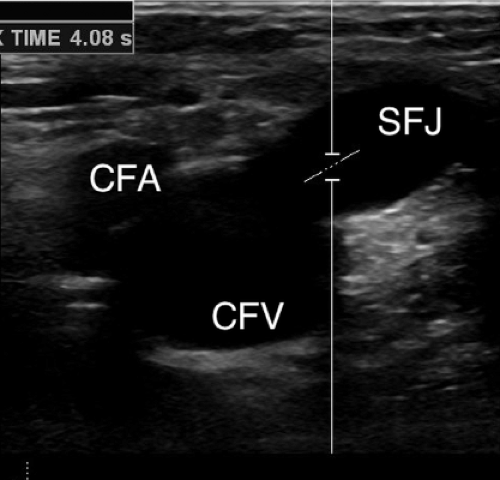
Venous duplex ultrasound has become the gold standard test to evaluate venous disease. Spectral analysis and B mode imaging using a 5- to 7.5-MHz transducer provides
reproducible, noninvasive means to define the anatomic, hemodynamic, and physiologic aspects of the venous anatomy. Reflux, defined as blood flowing toward the foot, that is greater than or equal to 0.5 ms is considered pathologic. In patients suspected of venous insufficiency, duplex ultrasound is performed of the deep veins and superficial veins of the affected lower extremity. Veins are assessed for patency and presence or absence of reflux, as well as other pertinent anatomic or pathologic findings (Figs. 14.1–14.3).
reproducible, noninvasive means to define the anatomic, hemodynamic, and physiologic aspects of the venous anatomy. Reflux, defined as blood flowing toward the foot, that is greater than or equal to 0.5 ms is considered pathologic. In patients suspected of venous insufficiency, duplex ultrasound is performed of the deep veins and superficial veins of the affected lower extremity. Veins are assessed for patency and presence or absence of reflux, as well as other pertinent anatomic or pathologic findings (Figs. 14.1–14.3).
Compression management is the first line of treatment in patients with CVI. This is thought to keep the superficial veins of the lower extremity from becoming engorged and to manage swelling. If patients fail conservative compression treatment, either surgical or endovascular management can be undertaken. In the past, surgical vein stripping in patients with axial venous reflux was performed in the operating room under anesthesia. Avulsion phlebectomy was performed either alone or in combination with surgical vein stripping to remove protruding varicosities. As endovascular techniques have developed in the treatment of arterial disease, similar catheter-based techniques were concurrently developing to treat venous disease. With the use of duplex ultrasonography, catheter-directed thermal energy is used to burn the endothelium of axial veins. Either radiofrequency or laser can be used and has essentially replaced surgical vein stripping. By direct thermal injury to the venous endothelium, occlusion of the treated vein occurs due to inflammation, thrombosis, and scarring. Additionally, ambulatory phlebectomy has been used in the office setting to remove varicosities either, concurrently with axial venous ablation or at a separate appointment, depending on the clinical situation. Small pieces of varicosities are removed through tiny incisions causing the remaining segments
to clot and ultimately to scar down. Patients are encouraged to continue to use graded compression stockings after treatment to minimize the risk of recurrence.
to clot and ultimately to scar down. Patients are encouraged to continue to use graded compression stockings after treatment to minimize the risk of recurrence.
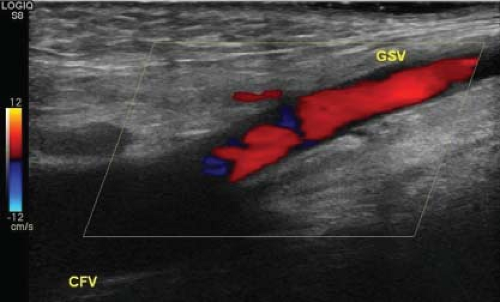 Figure 14.2 Ultrasound image of saphenofemoral junction with reflux shown with color flow. CFV, common femoral vein; GSV, greater saphenous vein. |
Contraindications
The clearest contraindication of axial vein ablation is the presence of normal venous flow and lack of reflux. History of deep venous thrombosis (DVT) should alert the clinician to carefully evaluate the deep system and consider the possibility of a higher risk of phlebitis postprocedure. Personal history of DVT, or thrombophilia, or family history of DVT or thrombophilia should alert the treating physician of a potentially higher risk of periprocedure thrombosis. Certain medications are associated with a higher incidence of phlebitis. Consideration is given to anticoagulation in the periprocedure period. Early on, anticoagulation was thought to be a contraindication due to risk of recanalization; however, patients are now routinely treated without stopping anticoagulants. Hemophilia, or other conditions which lead to excessive bleeding, should be carefully considered. Scheduling cases in a hospital setting may benefit the patient and may outweigh the possible bleeding risks. Patients who were treated in the past with ablation can be treated again in recanalized segments without issue.
All patients presenting with venous system complaints and pathology should undergo careful questioning of their medical history, family history, and medications. A trial of compression stockings is recommended with a scheduled follow-up visit. If the patient fails conservative management, then duplex ultrasound is used to study the venous anatomy and assess pathology; the presence or absence of reflux as well as patency in the deep and superficial veins are documented.
The day of the procedure, patients are discouraged to use moisturizers or oils on their skin. Patients do not require administration of antibiotics, unless preexisting medical conditions require prophylaxis. Antiplatelet agents do not need to be discontinued. Anticoagulants such as warfarin can be continued as long as the patient remains within reasonable therapeutic range. Once admitted to the office, patients are brought into a designated treatment room. An ultrasound is done prior to the beginning of the procedure to confirm and document the anatomy at the saphenofemoral or the saphenopopliteal junction. If the patient is undergoing phlebectomy in addition to the ablation, the




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree