INDICATIONS/CONTRAINDICATION
Indications
Thymectomy is one of the rare indications in thoracic surgery. Thymectomy is most commonly considered to be a part of the complex treatment of myasthenia gravis (MG) and thymoma. Ectopic thymic tissue can be located at various locations throughout the anterior mediastinum; therefore, the radicality of thymectomy is crucial for tumor resection and complete remission of MG. Robotic thymectomy is the latest advancement in the surgery of the thymus gland. This is primarily due to the fact that it allows for a complete radical thymectomy, which improves the complete remission rate for MG when compared to the conventional thoracoscopic technique. The oncologic outcome in terms of overall survival and thymoma-related survival is promising, but a longer follow-up is needed to consider robotic thymectomy as a standard approach.
The first robotic thymectomy was published in 2001 though it was only a partial thymectomy for thymoma in this particular case. In 2003, a complete robotic thymectomy was described and after that many thoracic centers have started or switched to the robotic approach. Since that time, there were more than 3,500 robotic thymectomies registered by Intuitive Surgical.
MG is an antibody-mediated autoimmune disease of the neuromuscular junction. In the majority of patients (80% to 85%), autoantibodies to the muscle nicotinic acetylcholine receptor (AChR) are present. These antibodies lead to failure of neuromuscular transmission with muscle weakness. The minority of MG patients are seronegative for AChR antibodies. A second category of MG is due to autoantibodies against the muscle-specific kinase (MuSK) protein. These are present in 3% to 5% of MG patients. Thymectomy is considered for patients with seropositive AChR and negative for MuSK.
Other factor with relevance for the indication of thymectomy for MG is the clinical classification according to the Myasthenia Gravis Foundation of America (MGFA). According to the severity of the MG we distinguish two relevant groups, only ocular form (MGFA I) or generalized form (MGFA ≥II). According to the meta-analyses from Gronseth and Barohn, patients with moderate till severe form of generalized MG (MGFA ≥IIb) benefit from the thymectomy but not the ocular form. However, there is a controversy because 50% of MG patients initially have only an ocular form which in 50% to 70% of the cases change to generalized form in the first 2 to 3 years. In this case, a thymectomy is not possible in the first 2 years of the diagnoses of MG where benefit from thymectomy could be reached. Therefore, and according to retrospective studies, thymectomy is also indicated for patients with ocular MG.
Thymectomy is performed in all age categories according to many studies. Though many text books restrict the indication to “mainly patients between 8 and 60 years” there is no evidence on that. Our series contains successfully selected cases of patients down to the age of 4 years or beyond 60 years up to the age of 85 years.
Surgery is the mainstay of treatment for thymoma. When the tumor is at an early stage (Masaoka/Koga I through IIB), surgery is the first choice of treatment. If the tumor is apparently invasive and large (Masaoka/Koga II through III), preoperative (neoadjuvant) chemotherapy and/or radiotherapy may be used to decrease the size and improve resectability, before surgery is attempted.
Generally, thymectomy for MG without thymoma is relatively indicated when three of the following five factors are present: Generalized form of MG, seropositive AChR, suspicious thymic hyperplasia, initial diagnosis less than 2 years, and patient age between 8 and 60.
Contraindications
There is still doubt on the indication for thymectomy for patients with seronegative AChR antibodies, ocular MG, and MuSK positive antibodies. However, with the exception of MUSK-antibody-positive patients, there is some data that show benefit from thymectomy for these groups.
Due to unstable MG or patients in myasthenic crisis thymectomy always requires preparation with stabilization of MG by plasma exchange strategies or intravenous immunoglobulin treatment.
The principal contraindication to the performance of a thymectomy is advanced stage thymoma (Masaoka III through IVB). However, for Masaoka stage III, resectability should be judged upon the invaded organs.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
All patients with MG should be evaluated by a neurologist, ideally in a center specialized for MG. All tests to diagnose MG should be reviewed. The antibody status for AChR and MuSK should be evaluated. All patients should undergo a contrast-enhanced CT scan of the thoracic cavity. Pulmonary function tests and arterial blood gas analyses are necessary. Beside these tests all patients have to be checked for operability due to other diseases. Optimally patients with a thymoma are discussed in a tumor board in large centers.
 SURGERY
SURGERY
The Left-Sided Robotic Thymectomy
Positioning
The left-sided minimally invasive thoracoscopic surgery employing the da Vinci telemetric robotic system is used. Surgery is performed under general anesthesia with one-lung ventilation. The patient is placed in a supine position on a vacuum mattress with the operating table slightly tilted to the right patient’s side. The left arm is positioned below the table level with flexion at the elbow. The initial position of the surgeon and his assistant is on the left side of the patient. The operation field is always prepared and draped for a conversion to median sternotomy or additional cervical approach or right-sided, thoracoscopy, respectively. The 12-mm trocar for the binocular camera is placed in the fourth intercostal space at the left anterior axillary line. A thoracoscopic 10-mm camera with a 30-degree optic is introduced to evaluate the operation field and help positioning the other two 8-mm trocars. The cranial trocar is introduced in the third intercostal space whereas the caudal trocar is located in the fifth intercostal space, both between the anterior axillary line and the midclavicular line. Thus, all three trocars are placed exactly along the submammary fold. The special da Vinci trocars are connected with the three robotic arms of the table cart. A harmonic scalpel is placed in the upper trocar whereas a bipolar forceps in the lower one.
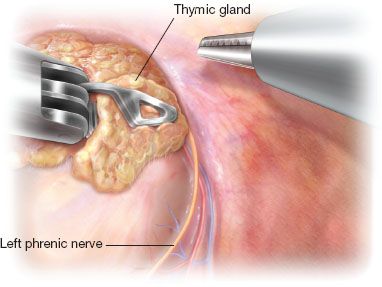
Figure 26.1 Operation field after mobilization of the thymic gland along the left phrenic nerve.
Technique
Step 1 (Fig. 26.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


