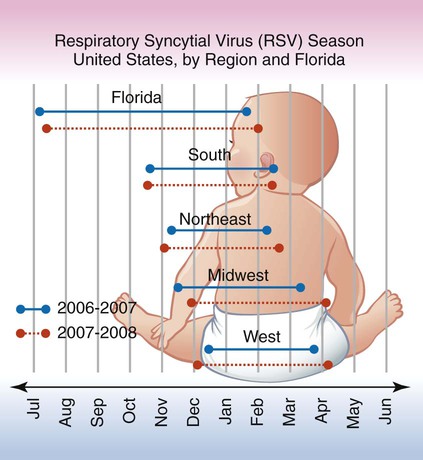
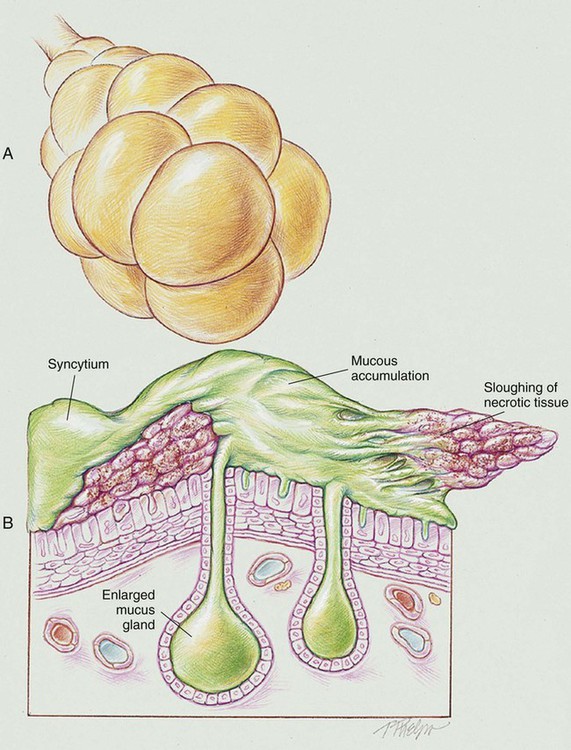
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with respiratory syncytial virus (RSV) infection. • Describe the causes of respiratory syncytial virus infection. • List the cardiopulmonary clinical manifestations associated with respiratory syncytial virus infection. • Describe the general management of respiratory syncytial virus infection. • Describe the clinical strategies and rationales of the SOAP presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. RSV infection causes peribronchiolar mononuclear infiltration and necrosis of the epithelium of the small airways. This condition leads to edema of the small airways and increased production of mucus. As the condition worsens, the epithelium of the small airways becomes necrotic and proliferates into the airway lumen. The combination of sloughing necrotic tissue, airway edema, and accumulation of mucus leads to (1) a decreased airway lumen, (2) a partially obstructed airway, or (3) a completely obstructed airway. Partial airway obstruction leads to alveolar hyperinflation as a result of a “ball-valve” mechanism (see Figure 36-1). Complete airway obstruction leads to alveolar collapse or atelectasis. Pneumonic consolidation is common. RSV is also referred to as bronchiolitis or pneumonitis. The following major pathologic or structural changes are associated with RSV infection: Although the outbreak of RSV cases varies by location each year, the number of RSV cases typically increases during the fall, winter, and early spring months. It is not fully known why RSV outbreaks occur in certain regions more than in others, but temperature, climate, and humidity appear to play a role. Figure 36-2 shows the typical RSV season in the United States by region and in Florida according to the Centers for Disease Control and Prevention.
Respiratory Syncytial Virus Infection (Bronchiolitis or Pneumonitis)
Anatomic Alterations of the Lungs
Etiology and Epidemiology