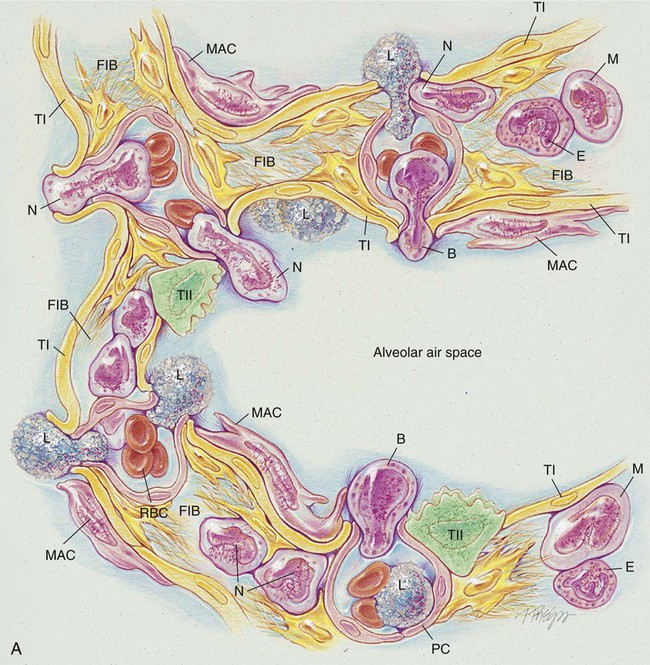
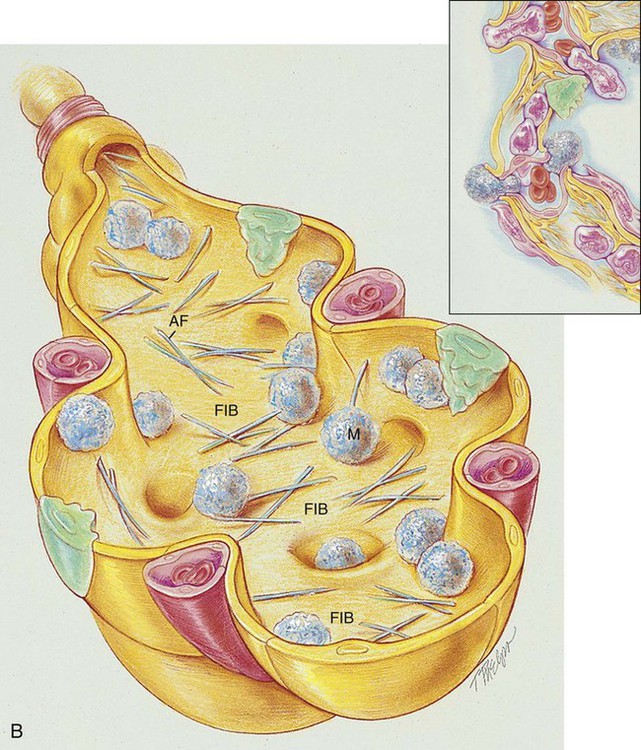
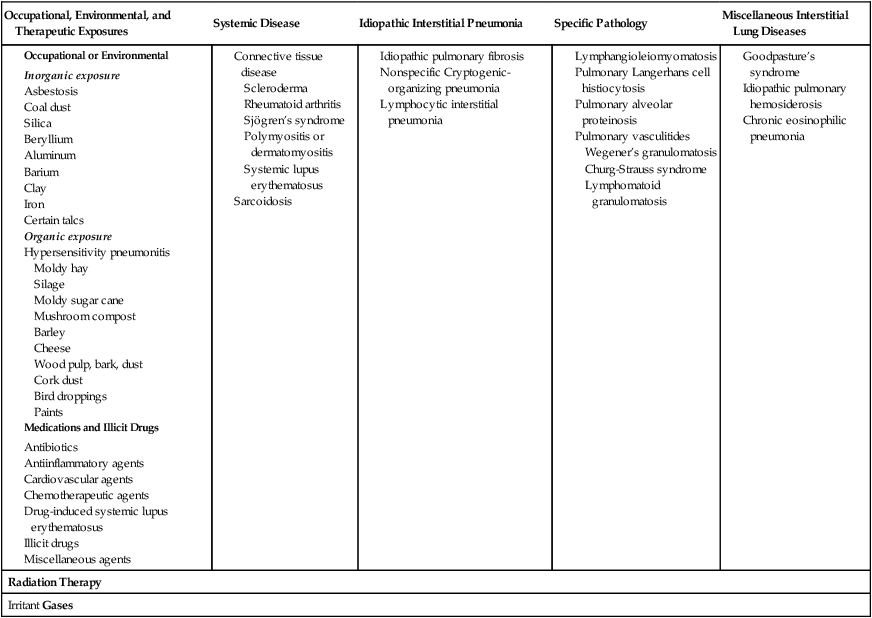
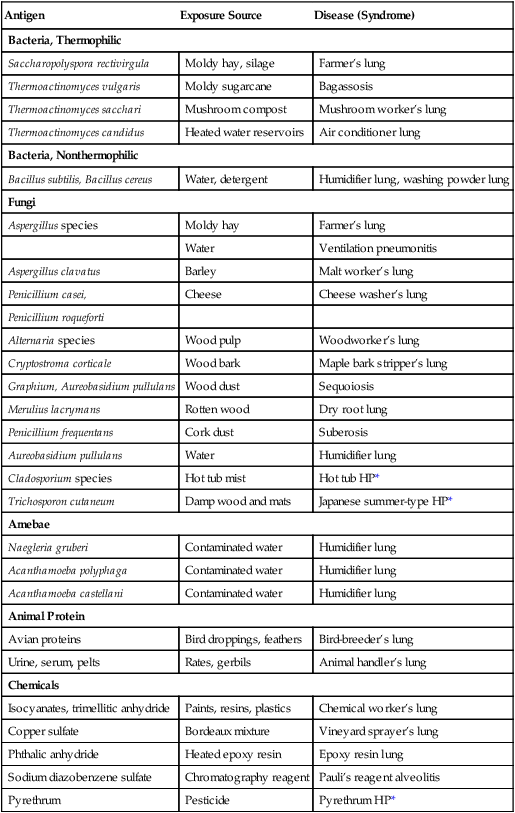
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with chronic interstitial lung disease. • Describe the causes of chronic interstitial lung disease. • List the cardiopulmonary clinical manifestations associated with chronic interstitial lung disease. • Describe the general management of chronic interstitial lung disease. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. The anatomic alterations of ILD may involve the bronchi, alveolar walls, and adjacent alveolar spaces. In severe cases the extensive inflammation leads to pulmonary fibrosis, granulomas, honeycombing, and cavitation. During the acute stage of any ILD, the general inflammatory condition is characterized by edema and the infiltration of a variety of white blood cells (e.g., neutrophils, eosinophils, basophils, monocytes, macrophages, and lymphocytes) in the alveolar walls and interstitial spaces (see Figure 25-1, A). Bronchial inflammation and thickening and increasing airway secretions may be also present. The major pathologic or structural changes associated with chronic ILDs are as follows: • Destruction of the alveoli and adjacent pulmonary capillaries • Fibrotic thickening of the respiratory bronchioles, alveolar ducts, and alveoli • Honeycombing and cavity formation • Fibrocalcific pleural plaques (particularly in asbestosis) • Excessive bronchial secretions (caused by inflammation of airways) Because there are over 180 different pulmonary disorders classified as ILD, it is helpful to group them according to their occupational or environmental exposure, disease associations, and specific pathology. Table 25-1 provides an overview of common ILD groups. A discussion of the more common ILDs follows. Table 25-1 Overview of Interstitial Lung Diseases Exposure to asbestos may cause asbestosis—a common form of ILD. Asbestos fibers are a mixture of fibrous minerals composed of hydrous silicates of magnesium, sodium, and iron in various proportions. There are two primary types: the amphiboles (crocidolite, amosite, and anthophyllite) and chrysotile (most commonly used in industry). Asbestos fibers typically range from 50 to 100 µm in length and are about 0.5 µm in diameter. The chrysotiles have the longest and strongest fibers. Box 25-1 lists common sources associated with asbestos fibers. As shown in Figure 25-1, B, asbestos fibers can be seen by microscope within the thickened septa as brown or orange baton-like structures. The fibers characteristically stain for iron with Perls’ stain. The pathologic process may affect only one lung, a lobe, or a segment of a lobe. The lower lobes are most commonly affected. Pleural calcification is common and diagnostic in patients with an asbestos exposure history. Complicated silicosis is characterized by nodules that coalesce and form large masses of fibrous tissue, usually in the upper lobes and perihilar regions. In severe cases the fibrotic regions may undergo tissue necrosis and cavitate. Box 25-2 lists common occupations associated with silica exposure. Hypersensitivity pneumonitis (also called allergic alveolitis or extrinsic allergic alveolitis) is a cell-mediated immune response of the lungs caused by the inhalation of a variety of offending agents or antigens. Such antigens include grains, silage, bird droppings or feathers, wood dust (especially redwood and maple), cork dust, animal pelts, coffee beans, fish meal, mushroom compost, and molds that grow on sugar cane, barley, and straw. The immune response to these allergens causes production of antibody and an inflammatory response. The lung inflammation, or pneumonitis, develops after repeated and prolonged exposure to the allergen. The term hypersensitivity pneumonitis (or allergic alveolitis) is often renamed according to the type of exposure that caused the lung disorder. For example, the hypersensitivity pneumonitis caused by the inhalation of moldy hay is called farmer’s lung. Table 25-2 provides common causes, exposure sources, and disease syndromes associated with hypersensitivity pneumonitis. Table 25-2 Causes of Hypersensitivity Pneumonitis *HP, Hypersensitivity pneumonitis. From Selman M: Hypersensitivity pneumonitis. In Schwarz MI, Kin TE, eds: Interstitial lung disease, ed 4, Hamilton, 2003, BC Decker. As the list of medications and illicit drugs continues to grow, so does the list of possible side effects (Box 25-4). Unfortunately, the lungs are major target organs affected by these side effects. Although it is impossible to discuss in detail the various lung-related side effects of every drug, it is possible to describe some of the general concerns related to drug-induced lung disease and to list some of the pharmacologic agents that may be responsible.
Interstitial Lung Diseases
Anatomic Alterations of the Lungs
Etiology and Epidemiology
Occupational, Environmental, and Therapeutic Exposures
Systemic Disease
Idiopathic Interstitial Pneumonia
Specific Pathology
Miscellaneous Interstitial Lung Diseases
Radiation Therapy
Irritant Gases
Interstitial Lung Diseases of Known Causes or Associations
Occupational, Environmental and Therapeutic Exposures
Inorganic particulate (dust) exposure
Asbestos
Silica
Organic materials exposure
Hypersensitivity pneumonitis
Antigen
Exposure Source
Disease (Syndrome)
Bacteria, Thermophilic
Saccharopolyspora rectivirgula
Moldy hay, silage
Farmer’s lung
Thermoactinomyces vulgaris
Moldy sugarcane
Bagassosis
Thermoactinomyces sacchari
Mushroom compost
Mushroom worker’s lung
Thermoactinomyces candidus
Heated water reservoirs
Air conditioner lung
Bacteria, Nonthermophilic
Bacillus subtilis, Bacillus cereus
Water, detergent
Humidifier lung, washing powder lung
Fungi
Aspergillus species
Moldy hay
Farmer’s lung
Water
Ventilation pneumonitis
Aspergillus clavatus
Barley
Malt worker’s lung
Penicillium casei,
Cheese
Cheese washer’s lung
Penicillium roqueforti
Alternaria species
Wood pulp
Woodworker’s lung
Cryptostroma corticale
Wood bark
Maple bark stripper’s lung
Graphium, Aureobasidium pullulans
Wood dust
Sequoiosis
Merulius lacrymans
Rotten wood
Dry root lung
Penicillium frequentans
Cork dust
Suberosis
Aureobasidium pullulans
Water
Humidifier lung
Cladosporium species
Hot tub mist
Hot tub HP*
Trichosporon cutaneum
Damp wood and mats
Japanese summer-type HP*
Amebae
Naegleria gruberi
Contaminated water
Humidifier lung
Acanthamoeba polyphaga
Contaminated water
Humidifier lung
Acanthamoeba castellani
Contaminated water
Humidifier lung
Animal Protein
Avian proteins
Bird droppings, feathers
Bird-breeder’s lung
Urine, serum, pelts
Rates, gerbils
Animal handler’s lung
Chemicals
Isocyanates, trimellitic anhydride
Paints, resins, plastics
Chemical worker’s lung
Copper sulfate
Bordeaux mixture
Vineyard sprayer’s lung
Phthalic anhydride
Heated epoxy resin
Epoxy resin lung
Sodium diazobenzene sulfate
Chromatography reagent
Pauli’s reagent alveolitis
Pyrethrum
Pesticide
Pyrethrum HP*
Medications and illicit drugs
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree