Aggressive low-density lipoprotein cholesterol (LDL-C)–lowering strategies are recommended for prevention of cardiovascular events in high-risk populations. Guidelines recommend a 30% to 50% reduction in at-risk patients even when LDL-C concentrations are between 70 and 130 mg/dl (1.8 to 3.4 mmol/L). However, calculation of LDL-C by the Friedewald equation is the primary laboratory method for routine LDL-C measurement. We compared the accuracy and reproducibility of calculated LDL-C <130 mg/dl (3.4 mmol/L) to LDL-C measured by β quantification (considered the gold standard method) in 15,917 patients with fasting triglyceride concentrations <400 mg/dl (4.5 mmol/L). Both variation and bias of calculated LDL-C increased at lower values of measured LDL-C. The 95% confidence intervals for a calculated LDL-C of 70 mg/dl (1.8 mmol/L) and 30 mg/dl (0.8 mmol/L) were 60 to 86 mg/dl (1.6 to 2.2 mmol/L) and 24 to 60 mg/dl (0.6 to 1.6 mmol/L), respectively. Previous recommendations have emphasized the requirement for a fasting sample with triglycerides <400 mg/dl (4.5 mmol/L) to calculate LDL-C by the Friedewald equation. However, no recommendations have addressed the appropriate lower reportable limit for calculated LDL-C. In conclusion, calculated LDL-C <30 mg/dl (0.8 mmol/L) should not be reported because of significant deviation from the gold standard measured LDL-C results, and caution is advised when using calculated LDL-C F values <70 mg/dl (1.8 mmol/L) to make treatment decisions.
Calculation of low-density lipoprotein cholesterol (LDL-C) by the Friedewald equation (total cholesterol – low-density lipoprotein cholesterol [HDL-C] – [triglycerides/5], referred to as LDL-C F ) has been the standard of practice for decades and remains the primary laboratory method for routine LDL-C orders. Surprisingly, the analytical performance of the Friedewald equation at low LDL-C concentrations has not been previously defined in a large cross-sectional outpatient population. Here we report on the accuracy and reproducibility of calculated LDL-C F <130 mg/dl (3.4 mmol/L) compared with LDL-C measured by β quantification (LDL-C ßQ ), which is considered the gold standard LDL-C method and is the foundation on which the Friedewald equation was based.
Methods
Patient data were accessed in compliance with the Mayo Clinic Institutional Review Board. The present study included 15,917 patients with clinically ordered LDL-C ßQ . Serum LDL-C ßQ measurement included quantitation of HDL-C and triglycerides that were subsequently used to calculate LDL-C F . Inclusion criteria were total serum triglycerides <400 mg/dl (4.5 mmol/L) and LDL-C F <130 mg/dl (3.4 mmol/L). The mean patient age was 50 ± 19 years; 46% were women ( Table 1 ). Patients were directed to fast for a minimum of 8 hours before sample collection. Cholesterol (Cholesterol Generation 2; Roche Diagnostics, Indianapolis, Indiana) and triglycerides (Roche Diagnostics) were measured using a Cobas c501 (Roche Diagnostics). To determine LDL-C ßQ , 1.0 ml serum was centrifuged for 15 hours at 86,000 g (Beckman LE-80K ultracentrifuge, Type 25 rotor; Beckman Coulter, Inc., Brea, California). The very low–density layer was removed according to volumetric guide (275 μl). The remaining fraction was weighed (required density 1.00 to 1.07 g/ml) and then reconstituted to 1.0 ml using distilled water. Cholesterol was measured before and after precipitation of LDL using a dextran sulfate solution (Pointe Scientific, Canton, Michigan). LDL-C F was calculated as described earlier. The Mayo Clinic Cardiovascular Medicine clinical testing laboratory is certified by the Centers for Disease Control and Prevention Lipid Standardization Program for quantitation of cholesterol, HDL-C, triglycerides, and LDL-C ßQ . LDL-C precision was determined by daily repeat analysis (n = 37) of pooled serum (LDL-C ßQ mean 109 mg/dl, SD 4.2 mg/dl, %CV 3.9%; LDL-C F mean 107 mg/dl, SD 3.2 mg/dl, %CV 3.1%). Graphical regression and statistical analyses were performed using JMP software (SAS Inc., Cary, North Carolina).
| LDL-C F Category | < 30 mg/dL | 30-69 mg/dL | 70-99 mg/dL | 100-129 mg/dL | Overall |
|---|---|---|---|---|---|
| N | 187 | 3,049 | 6,306 | 6,375 | 15,917 |
| Female, N (%) | 66 (35%) | 1,145 (38%) | 2,800 (44%) | 3,202 (50%) | 7,213 (46%) |
| Age, mean±SD | 48±23 | 53±22 | 50±21 | 50±19 | 50±19 |
| Lipids, mg/dL; median (IQR) | |||||
| Measured LDL-C ßQ | 33 (27 – 39) | 64 (57 – 71) | 90 (82 – 98) | 116 (108 – 124) | 97 (79 – 113) |
| Calculated LDL-C F | 22 (15 – 27) | 58 (49 – 64) | 86 (78.2 – 93) | 113 (106 – 121) | 93 (74 – 110) |
| Total Cholesterol | 86 (70 – 102) | 125 (112 – 139) | 158 (146 – 171) | 190 (177 – 203) | 167 (144 – 188) |
| HDL Cholesterol | 32 (22 – 43) | 39 (31 – 48) | 43 (36 – 53) | 46 (38 – 55) | 43 (35 – 53) |
| Triglycerides | 155 (67 – 255) | 120 (81 – 189) | 121 (83 – 183) | 127 (89 – 189) | 123 (85 – 187) |
Results
LDL-C F results were significantly lower than LDL-C ßQ across the entire cohort. LDL-C F values ranged from −16 to 129 mg/dl (−0.4 to 3.3 mmol/L), whereas LDL-C ßQ ranged from 7 to 164 mg/dl (0.2 to 4.2 mmol/L). Among patients with LDL-C F between 70 and 99 mg/dl (1.8 to 2.6 mmol/L), the median difference between LDL-C F and LDL-C ßQ was −4 mg/dl with an IQR of −9 to 0 mg/dl (0.1 mmol/L; −0.2 to 0 mmol/L). Underestimation of LDL-C F was exacerbated at lower LDL-C F ranges, with a median difference of −11 mg/dl (IQR −21 to −5 mg/dl [−0.3 mmol/L, IQR −0.5 to −0.1 mmol/L]) for patients with LDL-C F <30 mg/dl (<0.8 mmol/L).
Overall, the median triglyceride concentration was 123 mg/dl (1.4 mmol/L). LDL-C F underestimation worsened with increasing triglycerides; however, there was no significant correlation between LDL-C F and triglycerides. Serum triglycerides were <200 mg/dl (2.26 mmol/L) in 12,528 patients (79%) and in 2,485 patients (77%) with LDL-C F <70 mg/dl (1.8 mmol/L).
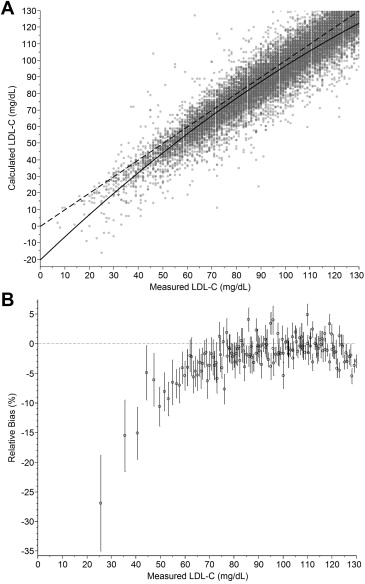
Increased discordance between LDL-C F and LDL-C ßQ at low concentrations was because of both increased variation and increased bias in the calculated LDL-C F results ( Figure 1 ). The 95% confidence interval for an LDL-C F of 70 mg/dl (1.8 mmol/L) was 60 to 86 mg/dl (1.6 to 2.2 mmol/L), and the 95% confidence interval for an LDL-C F of 30 mg/dl (0.8 mmol/L) increased to 24 to 60 mg/dl (0.6 to 1.6 mmol/L), further demonstrating the increased variability with lower LDL-C F .
Results
LDL-C F results were significantly lower than LDL-C ßQ across the entire cohort. LDL-C F values ranged from −16 to 129 mg/dl (−0.4 to 3.3 mmol/L), whereas LDL-C ßQ ranged from 7 to 164 mg/dl (0.2 to 4.2 mmol/L). Among patients with LDL-C F between 70 and 99 mg/dl (1.8 to 2.6 mmol/L), the median difference between LDL-C F and LDL-C ßQ was −4 mg/dl with an IQR of −9 to 0 mg/dl (0.1 mmol/L; −0.2 to 0 mmol/L). Underestimation of LDL-C F was exacerbated at lower LDL-C F ranges, with a median difference of −11 mg/dl (IQR −21 to −5 mg/dl [−0.3 mmol/L, IQR −0.5 to −0.1 mmol/L]) for patients with LDL-C F <30 mg/dl (<0.8 mmol/L).
Overall, the median triglyceride concentration was 123 mg/dl (1.4 mmol/L). LDL-C F underestimation worsened with increasing triglycerides; however, there was no significant correlation between LDL-C F and triglycerides. Serum triglycerides were <200 mg/dl (2.26 mmol/L) in 12,528 patients (79%) and in 2,485 patients (77%) with LDL-C F <70 mg/dl (1.8 mmol/L).
Increased discordance between LDL-C F and LDL-C ßQ at low concentrations was because of both increased variation and increased bias in the calculated LDL-C F results ( Figure 1 ). The 95% confidence interval for an LDL-C F of 70 mg/dl (1.8 mmol/L) was 60 to 86 mg/dl (1.6 to 2.2 mmol/L), and the 95% confidence interval for an LDL-C F of 30 mg/dl (0.8 mmol/L) increased to 24 to 60 mg/dl (0.6 to 1.6 mmol/L), further demonstrating the increased variability with lower LDL-C F .




