The present study aimed to determine the predictors of patient-reported quality of life and restrictive right ventricular (RV) physiology in adolescents and adults with repaired tetralogy of Fallot. A total of 62 patients (median age 28.5 years, range 14 to 69) undergoing cardiovascular magnetic resonance imaging completed the Short Form 36-item questionnaire, version 2, a validated quality of life assessment. RV inflow curves were generated from the sum of tricuspid inflow and pulmonary insufficiency. The patient-reported quality of life was comparable to population norms. Patients repaired after 1 year of age showed a strong trend toward a greater likelihood of physical component summary age-adjusted z-score ≤−1 (odds ratio 7.50, 95% confidence interval 0.90 to 62.3, p = 0.06). Patients with a RV ejection fraction of <45% reported decreased physical component summary (p = 0.02) and physical functioning (p = 0.02) scores. The RV end-diastolic volume, pulmonary regurgitation, and diastolic indexes did not predict the quality of life. The indexed RV end-diastolic volume was related to diastolic abnormalities, correlating with a greater peak early filling rate (r = 0.71, p <0.0001), ratio of peak early to atrial filling rates (r = 0.45, p = 0.006), and showing a strong trend with the end-diastolic forward flow in the pulmonary trunk (odds ratio 2.67 for moderate dilation and 3.50 for severe dilation, p = 0.06). Patients who underwent repair before 1 year old were more likely to have end-diastolic forward flow (15 of 17 vs 25 of 42, p = 0.03). In conclusion, the RV ejection fraction and age of repair were the best predictors of quality of life in this population, in whom end-diastolic forward flow and associated diastolic parameters appeared to reflect an overdistended ventricle, which might suggest a role for early pulmonary valve replacement.
Tetralogy of Fallot (TOF) is the most common form of cyanotic congenital heart disease, with excellent long-term outcomes after repair, leading to a growing adult population. The physiologic factors that influence the quality of life in this patient population have not been delineated. The use of the Short Form 36-item questionnaire, a quality of life assessment clinically validated for patients aged ≥14 years, has been reported for patients with repaired TOF ; however, the data from version 2, which includes population-based normative data, has not. The right ventricular (RV) size and systolic function in these patients has been the subject of much attention, particularly in the context of severe pulmonary regurgitation. RV diastolic dysfunction, often defined as restrictive physiology by the presence of end-diastolic forward flow (EDFF) in the pulmonary trunk, is common in this population and has been correlated with decreased exercise tolerance and increased pulmonary regurgitation. The potential etiology and significance of restrictive physiology, including its influence on quality of life, remains unclear. The present study therefore aimed to determine the relation of systolic and diastolic parameters to quality of life in patients with repaired TOF and to determine the predictors of restrictive RV physiology in this population.
Methods
Patients with repaired TOF, age ≥14 years, were prospectively enrolled after clinical referral for cardiovascular magnetic resonance imaging (MRI) from June 2008 to December 2009. Subjects were excluded if they had additional significant cardiac malformations (e.g., atrioventricular septal defect) or contraindications to MRI or gadolinium, required anesthesia, or could not complete the Short Form 36-item questionnaire because of cognitive impairment. The institutional review board approved the study, and all subjects and parents of minors provided informed consent.
MRI was performed using a commercially available 1.5 T scanner (Philips Intera Achieva, Best, The Netherlands). Cine images were obtained with a breath-hold, electrocardiographic-gated, segmented k-space, steady-state free precession sequence. The left ventricular and RV end-systolic volume and end-diastolic volume (EDV) were measured in the short axis plane using commercially available software (ViewForum, Philips, Best, The Netherlands). Phase-contrast imaging was performed at the tricuspid valve annulus and the main pulmonary artery, using a free-breathing, electrocardiographic-gated, cine velocity-encoded sequence with 40 phases per cardiac cycle and encoding velocity of 150 cm/s (increased if aliasing occurred or dephasing was seen on the preceding cine images). Late gadolinium enhancement imaging was performed approximately 15 minutes after injection of 0.2 mmol/kg of gadopentetate dimeglumine (Magnevist, Bayer Pharmaceuticals, Leverkusen, Germany) or gadoteridol (Prohance, Bracco Diagnostics, Princeton, New Jersey), and was quantified in the RV as has been previously described.
Graphs of the RV inflow rate versus time were generated from the sum of the tricuspid inflow and pulmonary insufficiency, as previously described, with peak early and atrial filling rates, early filling fraction (percentage of RV filling occurring within first 1/3 of diastole), and deceleration time defined as in Figure 1 .
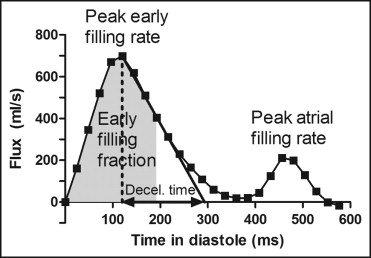
Restrictive physiology was defined categorically as the presence of EDFF in the pulmonary trunk on phase contrast imaging. Restrictive physiology was also evaluated as a pattern of increased peak early filling rate, early filling fraction, and ratio of peak early to atrial filling rate, and decreased peak atrial filling rate and deceleration time.
On enrollment or on the day of MRI, the subjects completed the Short Form 36-item questionnaire, version 2. The scores were normalized for age and compared to the population-based normative data. The physical component summary score and the subscales of physical functioning, role physical, and general health ( Table 1 ) were chosen to represent the physical effect of disease.
| Two summary scores |
| Physical component summary score |
| Mental component summary score |
| Eight subscales |
| Physical functioning: ability to perform physical activities |
| Role physical: participation in work or usual activities without physical limitations |
| Bodily pain: absence of pain that impacts normal activities |
| General health: perception of general health and its likelihood to change |
| Vitality: feeling of energy and subjective well-being |
| Social functioning: ability to participate in social activities |
| Role emotional: participation in work or usual activities without emotional limitations |
| Mental health: overall feeling of peace, happiness, and calm |
The data are presented as the mean ± SD, unless otherwise noted. A test for normal distribution was performed using the D’Agostino-Pearson test. Continuous variables were compared using Student’s t test or Wilcoxon rank sum test. Correlation was evaluated using linear regression analysis or Spearman’s rank correlation coefficient. Categorical variables were compared using chi-square analysis or Fisher’s exact test, when the expected value of any category was <5. The RVEDV was categorized by size and evaluated as a group linear variable using logistic regression analysis for the odds ratio of EDFF. The odds ratio and prevalence difference were calculated for an age-adjusted z score of ≤−1 (to represent a clinically significant difference in quality of life), with 95% confidence intervals calculated using the Taylor series. p Values of ≤0.05 were considered statistically significant.
Results
From June 2008 through December 2009, 67 patients met the inclusion criteria. Of these 67 patients, 62 were enrolled (2 patients did not complete MRI, 1 declined participation, and an investigator was not available for consent for 2 patients). The patient characteristics are listed in Table 2 .
| Characteristic | Value |
|---|---|
| Males | 37 (60%) |
| Age (years) | |
| Median | 28.5 |
| Range | 14–69 |
| Age at repair (years) | |
| Median | 3.4 |
| Range | 0.01–37 |
| Right ventricular end-diastolic volume (mL/m 2 ) | 146 ± 48 |
| Type of repair | |
| Transannular patch | 33 (55%) |
| Right ventricle to pulmonary artery conduit | 8 (13%) |
| Valve-sparing | 6 (10%) |
| Unspecified | 15 (24%) |
| Pulmonary regurgitant fraction (%) | 31 ± 21 |
| Indexed pulmonary regurgitant volume (ml/m 2 ) | 22 ± 18 |
| Left ventricular ejection fraction (%) | 54 ± 8 |
| Right ventricular ejection fraction (%) | 47 ± 8 |
| Presence of late gadolinium enhancement | 55/60 (92%) |
| Presence of end-diastolic forward flow | 40/59 (68%) |
The patient-reported quality of life in this population was similar to the population-derived norms. No statistically significant difference was found in the physical component summary (49.7 ± 10.1 vs 50.0 ± 10.0, p = 0.83) or mental component summary (51.0 ± 11.0 vs 49.9 ± 10.1, p = 0.44) scores. Although a statistically significant difference was found in the subscales of general health (47.3 ± 11.1 vs 50.0 ± 10.0, p = 0.04) and bodily pain (54.8 ± 8.6 vs 50.0 ± 10.0, p = 0.0003) from the population norms, no clinically significant difference was apparent.
Figure 2 shows the patient-reported quality of life scores stratified by normal or abnormal RV systolic function and left ventricular systolic function ( Figure 2 ). RV systolic dysfunction was associated with lower physical component summary (median 50.0, interquartile range 40.6 to 52.9, vs median 54.2, interquartile range 46.6 to 59.7, p = 0.02) and physical functioning (median 50.7, interquartile range 40.2 to 52.8, vs median 52.8, interquartile range 46.5 to 57.0) scores (p = 0.02).
Patient age at repair correlated inversely with the physical component summary score (r = −0.33, p = 0.008). The patients who underwent repair after 1 year showed a strong trend toward greater odds of a lower age-adjusted physical component summary score (p = 0.06; Figure 3 ). The absolute difference in the prevalence of a lower physical component summary score was 27% (95% confidence interval 8.9% to 45%).
The RVEDV, pulmonary regurgitant fraction, EDFF, diastolic indexes, and late gadolinium enhancement were not predictive of patient-reported quality of life. EDFF was further analyzed quantitatively by the volume of EDFF indexed to the body surface area and to forward flow and continued to show no relation to the quality of life.
EDFF correlated with the other indexes of restriction ( Table 3 ), with an increased early filling fraction and trend toward lower peak atrial filling rate and greater early to atrial filling ratio, as has been previously reported.
| Variable | All Patients | EDFF | No EDFF | p Value |
|---|---|---|---|---|
| Peak early filling rate (ml/s) | 517 ± 201 | 524 ± 184 | 503 ± 238 | 0.74 |
| Peak atrial filling rate (ml/s) | 320 ± 123 | 295 ± 98 | 369 ± 154 | 0.07 |
| Early/atrial filling ratio | 0.07 | |||
| Median | 1.6 | 1.7 | 1.4 | |
| Interquartile range | 1.2–2.0 | 1.3–2.5 | 0.8–1.8 | |
| Early filling fraction (ml/s) | 40 ± 14 | 44 ± 15 | 33 ± 9 | 0.001 |
| Deceleration time (ms) | 208 ± 96 | 210 ± 106 | 205 ± 76 | 0.85 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


