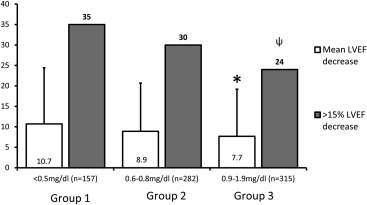
Myocardial injury because of oxidative stress manifesting through reductions in left ventricular ejection fraction (LVEF) may occur after the administration of anthracycline-based chemotherapy (A-bC). We hypothesized that bilirubin, an effective endogenous antioxidant, may attenuate the reduction in LVEF that sometimes occurs after receipt of A-bC. We identified 751 consecutively treated patients with cancer who underwent a pre-A-bC LVEF measurement, exhibited a serum total bilirubin level <2 mg/dl, and then received a post-A-bC LVEF assessment because of symptomatology associated with heart failure. Analysis of variance, Tukey’s Studentized range test, and chi-square tests were used to evaluate an association between bilirubin and LVEF changes. The LVEF decreased by 10.7 ± 13.7%, 8.9 ± 11.8%, and 7.7 ± 11.5% in group 1 (bilirubin at baseline ≤0.5 mg/dl), group 2 (bilirubin 0.6 to 0.8 mg/dl), and group 3 (bilirubin 0.9 to 1.9 mg/dl), respectively. More group 1 patients experienced >15% decrease in LVEF compared with those in group 3 (p = 0.039). After adjusting for age, coronary artery disease/myocardial infarction, diabetes mellitus, hematocrit, and the use of cardioactive medications, higher precancer treatment bilirubin levels and lesser total anthracycline doses were associated with LVEF preservation (p = 0.047 and 0.011, respectively). In patients treated with anthracyclines who subsequently develop symptoms associated with heart failure, pre-anthracycline treatment serum bilirubin levels inversely correlate with subsequent deterioration in post-cancer treatment LVEF. In conclusion, these results suggest that increased levels of circulating serum total bilirubin, an intrinsic antioxidant, may facilitate preservation of LVEF in patients receiving A-bC for cancer.
Leukemia, lymphoma, and tumors of the breast and skeletal muscle are frequently treated with anthracycline-based chemotherapy (A-bC) ; however, its use is limited by dose-dependent cardiotoxic effects including heart failure (HF). The mechanism for A-bC–mediated cardiac damage and HF is not fully elucidated. Cellular injury by increased oxidative stress within the cardiac myocytes is thought to play a central role in left ventricular ejection fraction (LVEF) reductions. For many years, bilirubin was considered a toxic by-product of heme metabolism due to the jaundice and brain damage it caused in newborns with severe hyperbilirubinemia. However, recent studies have demonstrated that higher levels of total serum bilirubin are associated with reduced risk of cardiovascular (CV) disease. Bilirubin’s cardioprotective effects are thought to be mediated through its endogenous antioxidant properties. Because bilirubin exhibits antioxidant properties, we sought to determine if an association was present between serum bilirubin levels and change in LVEF in those receiving A-bC. To address this question, we compared precancer treatment serum bilirubin levels to subsequent changes in LVEF that occurred in individuals who developed HF symptoms after receipt of A-bC.
Methods
This retrospective cohort study was approved by the Institutional Review Board at Wake Forest Health Sciences. Because the study posed minimum risk to the participants, informed consent was waived to gather data from previous health records. We identified all patients with cancer who received A-bC at Wake Forest Baptist Medical Center from January 2002 to January 2012 and underwent 2 measurements of LVEF, the first before receipt of treatment for their cancer and the second after experiencing symptoms suggestive of HF. We excluded those subjects with a diagnosis of congestive HF ( International Classification of Diseases, Ninth Revision , code 428.x) before receipt of A-bC or serum total bilirubin levels ≥2 mg/dl due to intrinsic liver disease before A-bC administration. We identified 751 patients who met the inclusion/exclusion criteria ( Figure 1 ).

Baseline demographic data, such as age, gender, race, weight, height, CV co-morbidities, cancer type, anthracycline dose, and CV medications, were obtained from medical records. The anthracycline dose was determined by reviewing all the medications that were dispensed from the hospital pharmacy for each participant. After summing the A-bC doses, they were converted to doxorubicin isotoxic equivalents as previously described (total doxorubicin dose × 1, total daunorubicin dose × 0.833, total epirubicin dose × 0.67, total idarubicin dose × 5, total mitoxantrone dose × 4).
The LVEF was measured by transthoracic echocardiography, multigated acquisition scan, or cardiac magnetic resonance scan as determined from the medical records. The change in LVEF was calculated as the difference between the pre-anthracycline LVEF and the lowest post-anthracycline LVEF during the follow-up period. Systemic arterial hypertension, coronary artery disease/myocardial infarction (CAD/MI), and diabetes mellitus were considered present if their respective International Classification of Diseases, Ninth Revision , codes were listed in the participants’ charts at the time of the first anthracycline dose. Serum total bilirubin, aspartate aminotransferase, alanine aminotransferase, albumin, and hematocrit levels from assessments obtained before initiation of their A-bC were recorded. Also, potentially CV-active concurrent medications, such as β blockers, angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), and statins, administered with cancer treatment were recorded. We documented whether participants received mediastinal, chest, or whole-body ionizing radiation as part of their cancer treatment regimen.
The data were analyzed using the SAS statistical software system (Cary, North Carolina). Participants were assigned to 1 of 3 groups according to their precancer treatment serum bilirubin levels (group 1 [bilirubin ≤0.5 mg/dl], group 2 [bilirubin 0.6 to 0.8 mg/dl], and group 3 [bilirubin 0.9 to 1.9 mg/dl]). The total bilirubin limits for each group were chosen to have similar numbers in each group. Participants with ≥2.0 mg/dl were excluded to avoid inclusion of those with dramatic elevations in serum bilirubin because of severe liver disease. Continuous data were presented as mean ± SD, whereas categorical data were presented as number (percent). Analysis of variance was used to test for the difference in the mean LVEF change across these groups. Tukey’s Studentized range and Bonferroni (Dunn) t tests were used in pairwise comparisons. The chi-square test was used for differences in categorical variables across the 3 groups. Cochran-Armitage trend test was used to assess for trends across the 3 groups.
Because the distribution of bilirubin levels was highly skewed toward higher values, logarithmically transformed values of bilirubin were used in the quantitative models of analysis. The correlation between the precancer treatment serum bilirubin levels and the serial pre- to post-chemotherapy changes in LVEF was analyzed using linear regression models. Adjustments for age, gender, potentially CV-active medications, thoracic radiation, and CV co-morbidities (hypertension, CAD/MI, diabetes) were performed to account for their potential influence on change in LVEF after receipt of A-bC. A p value <0.05 was considered significant in all analyses.
Results
The demographic data for the study participants are listed in Table 1 . Participants averaged 54 ± 16 years in age, 52% were men, 85% were Caucasian, and 13% were African-American. The most common locations of the cancers were the blood and bone marrow, lymph nodes, and breast in 80%, 10%, and 5% of the cases, respectively. There were no differences in the pre-anthracycline measures of LVEF between the groups ( Table 1 ).
| Bilirubin (mg/dl) | ||||
|---|---|---|---|---|
| Measure | ≤0.5 (n=186) | 0.6-0.8 (n=287) | 0.9- 1.9 (n=281) | p |
| Age (years) | 54±16 | 55±17 | 54±15 | 0.1 |
| Female | 46% | 49% | 59% | 0.0071 |
| White | 84% | 90% | 82% | 0.18 |
| Black | 15% | 9% | 16% | |
| Body mass index (kg/m 2 ) | 28 ± 8 | 29 ± 4 | 30 ± 7 | 0.011 |
| Albumin (g/dl) | 3.5 ± 0.6 | 3.4 ± 0.6 | 3.2 ± 0.6 | 0.15 |
| Hematocrit (%) | 29 ± 6 | 28 ± 5 | 27 ± 5 | 0.0062 |
| Prior coronary artery disease/myocardial infarction | 11% | 12% | 13% | 0.92 |
| Prior diabetes mellitus | 15% | 18% | 14% | 0.37 |
| Prior hypertension | 35% | 38% | 48% | 0.009 |
| On angiotensin converting enzyme inhibitor | 9% | 9% | 6% | 0.23 |
| On angiotensin receptor blocker | 2% | 4% | 4% | 0.47 |
| On β-blocker | 9% | 6% | 7% | 0.52 |
| On statin | 15% | 13% | 11% | 0.51 |
| Pre-anthracycline-based chemotherapy left ventricular ejection fraction (%) | 59.5 ± 7.0 | 58.9 ± 6.7 | 58.1 ± 7.2 | 0.10 |
| Doxorubicin equivalent (mg/m 2 ) | 392 ± 180 | 408 ± 230 | 406 ± 165 | 0.70 |
The time between the LVEF measurements averaged 496 ± 625 days (median: 285 days, minimum: 14 days, and maximum: 3,502 days). The participants with the lowest precancer treatment serum bilirubin levels (group 1) sustained the largest reduction in LVEF when presenting with symptoms warranting a repeat LVEF assessment ( Figure 2 ). Conversely, the lowest LVEF reductions observed between the precancer and post-cancer treatment assessments were observed in group 3 (p = 0.041, Figure 2 ). Using pairwise comparisons, there was a significant difference between the average reduction in LVEF when groups 1 and 3 were compared (difference between means of 2.9%, 95% confidence limits 0.2 to 5.6; p <0.05). The LVEF change was related to the bilirubin groups when the Cochran-Armitage trend test was applied (p = 0.011).
After adjusting for age, gender, and the use of potentially CV-active medications, the pre-A-bC serum bilirubin level and the cumulative doxorubicin equivalent dose of anthracycline administered were the only variables independently associated with a reduction in LVEF (p = 0.017 and 0.0085, respectively; Table 2 ). Total bilirubin and cumulative doxorubicin equivalent dose remained associated with LVEF reduction (p = 0.047 and 0.011, respectively, Table 3 ) after adjusting for age, gender, hypertension, CAD, diabetes, and thoracic radiation.



