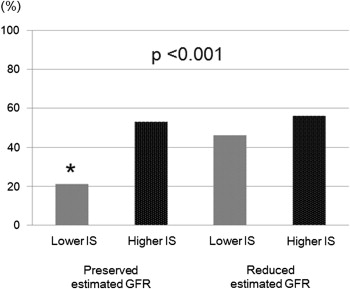
The prognosis of patients with diastolic heart failure (HF) is as poor as that of patients with systolic HF. Greater chronic kidney disease-associated mortality occurs in patients with left ventricular (LV) diastolic HF than in those with systolic HF. Indoxyl sulfate (IS), a uremic toxin, directly affects cardiac cells adversely in in vitro experiments. We investigated the association of IS, a uremic toxin, and chronic kidney disease with LV diastolic dysfunction in the clinical setting. The present study included 204 consecutive patients with preserved LV systolic function. To evaluate LV function, all patients underwent echocardiography. To measure the plasma IS levels and estimated glomerular filtration rate (eGFR), blood samples were obtained. Of the 204 patients, 75 (37%) had LV diastolic dysfunction. A significantly lower prevalence of LV diastolic dysfunction was present in patients with lower plasma IS levels (≤1.0 μg/ml) than those with greater plasma IS levels (38 [29%] vs 37 [51%], p <0.001). Furthermore, a significantly lower prevalence of LV diastolic dysfunction was present in patients with lower plasma IS levels and preserved eGFR than those with greater plasma IS levels and preserved eGFR, those with lower plasma IS levels and a reduced eGFR, or those with greater plasma IS levels and reduced eGFR (20 [21%] vs 18 [53%], p = 0.001; 20 [21%] vs 18 [46%], p = 0.004; and 20 [21%] vs 19 [56%], p <0.001, respectively). In conclusion, greater plasma IS levels or a reduced eGFR, or both, represent an increased risk of LV diastolic dysfunction.
Indoxyl sulfate (IS) is a protein-bound uremic toxin generated by metabolism of dietary tryptophan. One study in a clinical setting revealed high blood IS levels to be an independent predictor of cardiovascular disease. Although IS has reportedly both vascular toxicity and nephrotoxicity, the mechanisms underlying its association with a poor prognosis has not been fully elucidated. In patients with heart failure (HF), poor outcomes were still a major clinical problem. It is known that of all patients with HF, about ½ have preserved left ventricular (LV) systolic function. The prognosis of patients with diastolic HF is as threatening as that of patients with systolic HF. Recently, an association between chronic kidney disease (CKD) and an increased mortality in patients with HF has been validated. Furthermore, greater CKD-associated mortality occurs in patients with diastolic HF than in those with systolic HF. Lekawanvijit et al showed that IS also exerts profibrotic, prohypertrophic, and proinflammatory effects on cardiac cells in vitro, which might contribute adversely to cardiac function. Recent developments in echocardiographic techniques have allowed us to evaluate cardiac function noninvasively and in detail in vivo. In the present study, we tested our hypothesis that high plasma IS levels are associated with a high prevalence of LV diastolic dysfunction.
Methods
We prospectively screened consecutive patients referred for percutaneous coronary intervention (PCI) from May 2009 to December 2010 at Nagoya University Hospital. We included patients with both stable angina pectoris and successful PCI. Patients with a history of acute coronary syndrome before screening for inclusion were excluded. Stable angina pectoris was diagnosed by the cardiologist in charge according to the previous report. Successful PCI was defined as a final angiographic residual stenosis of <30% as determined by quantitative coronary angiography without flow-limiting dissection or occlusion of the large branch (>1 mm) and a resulting Thrombolysis In Myocardial Infarction grade of 3. Patients who experienced periprocedural myocardial injury, defined as an increase in troponin T 3 times greater than the upper limit of the reference range 24 hours after PCI, were excluded. Also excluded were patients with moderate to severe valvular heart disease diagnosed according to a previous report or LV systolic dysfunction, defined as an LV ejection fraction ≤50% and LV end-diastolic volume index ≥97 ml/m 2 . The local institutional ethics committee of Nagoya University Hospital approved the study protocol. All patients provided written informed consent.
To evaluate the renal profiles, fasting blood samples were obtained from a peripheral vein the morning of the day 1 month after PCI. For determination of the plasma IS levels, the samples were filtered through a 0.20-μm membrane. Next, 10-μl aliquots were analyzed by reverse-phase high-performance liquid chromatography (Shiseido Capcell Pak MF Ph-1 SG80 MF, 150 mm × 4.6 mm, Shiseido, Tokyo, Japan). The mobile phase, 0.1 M KH 2 PO 4 /tetrahydrofuran (95/5), was delivered at a flow rate of 1.0 ml/min at 35°C. The plasma concentrations were determined by fluorescence detection (excitation 295 nm, emission 390 nm). Greater plasma IS levels were defined as those of >1.00 μg/ml (the highest tertile). The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease study equation modified with the Japanese coefficient (0.741 × Modification of Diet in Renal Disease). We used a modified National Kidney Foundation classification of CKD. We divided the enrolled patients into preserved or reduced eGFR groups according to the cutoff value of ≥60 ml/min/1.73 m 2 . Hypertension was defined as a baseline blood pressure ≥140/90 mm Hg or the need for antihypertensive agents. Dyslipidemia was diagnosed when patients had low-density lipoprotein cholesterol ≥140 mg/dl, triglycerides ≥150 mg/dl, or high-density lipoprotein cholesterol <40 mg/dl or were taking lipid-modifying agents.
Immediately after blood sampling, echocardiography was performed using a commercially available system (Vivid 7, GE Healthcare, Milwaukee, Wisconsin) with a 1.5- to 4.0-MHz transducer immediately after blood sampling. The left atrial volumes were measured using the biplane area-length method on an apical 4-chamber view and were indexed to the body surface area. The LV end-diastolic and end-systolic dimensions were measured using M-mode echocardiography, as previously reported. The LV ejection fractions were calculated from the apical 4-chamber views using the modified Simpson method. The LV mass was calculated using a 2-dimensional method and indexed to the body surface area. To assess mitral inflow, pulsed-wave Doppler imaging was performed with apical 4-chamber views, as previously described. The peak E and peak A velocity and deceleration time were determined. The mitral annular diastolic velocity (e′) was measured using Doppler tissue imaging by placing a sample volume on the septal from the apical 4-chamber view. LV systolic dysfunction was defined as LV ejection fraction ≤50% and LV end-diastolic volume index ≥97 ml/m 2 . In patients with preserved LV systolic function, LV diastolic dysfunction was defined as E/e′ >15 or >8 but <15 plus an E/A <0.5 and deceleration time >280 ms, left atrial volume index >40 ml/m 2 , LV mass index >122 g/m 2 for women or >149 g/m 2 for men, or electrocardiographic evidence of atrial fibrillation, in line with the findings from a previous report.
All statistical analyses were performed using SPSS, version 18 (SPSS, Chicago, Illinois). Continuous variables are presented as the mean SD, and differences between pairs of groups were evaluated using the Student unpaired t test. If the distribution was not normal, the variables are presented as the median and interquartile range, and the differences were evaluated using the Mann-Whitney U test. Categorical variables are described as numbers and percentages, and comparisons across the groups were analyzed using the chi-square test or Fisher’s exact test. All variables in Table 1 were entered into the univariate logistic analyses. The predictive variables with p <0.01 were entered into the multivariate logistic analysis to determine the independent predictors of LV diastolic dysfunction. A 2-tailed p value <0.05 was considered statistically significant.
| Variable | LV Diastolic Dysfunction | p Value | |
|---|---|---|---|
| Yes (n = 75) | No (n = 129) | ||
| Age (yrs) | 72 ± 8 | 66 ± 10 | <0.001 |
| Men | 54 (72%) | 99 (77%) | 0.504 |
| Hypertension | 63 (84%) | 84 (65%) | 0.006 |
| Diabetes mellitus | 38 (51%) | 45 (35%) | 0.038 |
| Dyslipidemia | 50 (67%) | 97 (75%) | 0.199 |
| Cigarette smoking | 17 (23%) | 39 (30%) | 0.260 |
| Multiple vessel coronary disease | 36 (48%) | 57 (44%) | 0.662 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 60 ± 23 | 70 ± 20 | 0.001 |
| Plasma indoxyl sulfate level (μg/ml) | 0.94 (0.57–1.5) | 0.72 (0.45–1.0) | 0.002 |
| Medications | |||
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers | 46 (61%) | 72 (56%) | 0.465 |
| β Blockers | 25 (33%) | 30 (23%) | 0.141 |
| Statins | 47 (63%) | 92 (71%) | 0.215 |
Results
We investigated 204 consecutive patients with both stable angina pectoris and successful PCI. Their mean age was 68 ± 10 years and 154 (75%) were men. Of the 204 patients, 75 (37%) had LV diastolic dysfunction, as determined by an E/e′ >15 in 50 patients, E/e′ <8 but >15, with an E/A <0.5 plus deceleration time >280 ms in 0, left atrial volume index >40 ml/m 2 in 30, LV mass index >122 g/m 2 for women or >149 g/m 2 for men in 47, and electrocardiographic evidence of atrial fibrillation in 8 patients (some patients met multiple criteria). The patient characteristics of both groups are listed in Table 1 . The echocardiographic findings are listed in Table 2 .
| Variable | LV Diastolic Dysfunction | p Value | |
|---|---|---|---|
| Yes (n = 75) | No (n = 129) | ||
| Left atrial volume index (ml/m 2 ) | 37 ± 9 | 30 ± 5 | <0.001 |
| Left ventricular end-diastolic volume index (ml/m 2 ) | 54 ± 6 | 52 ± 6 | 0.006 |
| Left ventricular end-systolic volume index (ml/m 2 ) | 16 ± 3 | 15 ± 2 | 0.108 |
| Left ventricular ejection fraction (%) | 68 ± 8 | 66 ± 6 | 0.076 |
| Peak E-wave velocity (m/s) | 7.8 ± 2.2 | 6.3 ± 1.6 | <0.001 |
| Peak A-wave velocity ∗ | 9.3 ± 2.5 | 7.8 ± 1.6 | <0.001 |
| E-wave/A-wave ratio ∗ | 0.87 ± 0.32 | 0.83 ± 0.28 | 0.327 |
| Deceleration time (ms) | 239 ± 65 | 236 ± 75 | 0.718 |
| Septal e′ (cm/s) | 4.7 ± 1.3 | 6.2 ± 1.9 | <0.001 |
| E-wave/septal e′ | 17.3 ± 5.2 | 10.4 ± 2.4 | <0.001 |
| Left ventricular mass index | 143 ± 39 | 112 ± 24 | <0.001 |
∗ Five patients with LV diastolic dysfunction were excluded because of atrial fibrillation (leaving 70 with LV diastolic dysfunction).
The prevalence of LV diastolic dysfunction was significantly lower in the lower IS (≤1.0 μg/ml) group than in the higher IS group (>1.0 μg/ml; 38 [29%] vs 37 [51%], p <0.001), supporting a theory based on the results of an in vitro experiment showing the direct toxicity of IS on cardiac cells. A significantly reduced eGFR was evident in the lower IS group than those in the higher IS group (53 ± 21 vs 72 ± 19 ml/min/1.73 m 2 , p <0.001). The relation among plasma IS levels, eGFR, and the prevalence of LV diastolic dysfunction is shown in Figure 1 . A significantly lower prevalence of LV diastolic dysfunction was obtained from patients with lower plasma IS levels and preserved eGFR than from those with was greater plasma IS levels and preserved eGFR, those with lower plasma IS levels and reduced eGFR, and those with greater plasma IS levels and reduced eGFR (20 [21%] vs 18 [53%], p = 0.001; 20 [21%] vs 18 [46%], p = 0.004; and 20 [21%] vs 19 [56%], p <0.001, respectively). In patients with reduced eGFR, no significant difference was found of the incidence of LV diastolic dysfunction between the lower and higher IS groups (18 [46%] vs 19 [56%], p = 0.484).