Warfarin decreases risk of stroke for patients with atrial fibrillation (AF) dependent on percent time in the therapeutic range (TTR) with an international normalized ratio (INR) of 2 to 3. We hypothesized that gender differences in ischemic stroke risk are related to TTR. From the AFFIRM database of 4,060 patients with AF, we determined the incidence of ischemic stroke by gender. We evaluated the INR at time of ischemic stroke and calculated TTR. We determined the relation between gender and ischemic stroke by TTR. Women had CHADS 2 Scores (3.7 ± 1.3 vs 2.5 ± 1.3, p <0.0001) and more ischemic strokes than men (5% vs 3%, odds ratio 1.6, 95% confidence interval 1.19 to 2.26, p = 0.002). Mean INR near time of ischemic stroke was 2 for women and men; median values were subtherapeutic (1.7 and 1.8, respectively). Women spent more time outside the therapeutic range (40 ± 0.7% vs 37 ± 0.5%, p = 0.0001), with more time below the therapeutic range (29 ± 0.7% vs 26 ± 0.5%, p = 0.0002). A higher TTR protected against ischemic stroke for women but not for men. Women who had a comparably high TTR (≥66%) still had more ischemic strokes (p = 0.009). A fitted Cox proportional hazard regression model showed that gender, TTR <46% versus >80%, age, and previous stroke were significantly related to stroke incidence. In conclusion, women in AFFIRM were at greater risk of ischemic stroke than men, in part related to differences in TTR. Women with AF may benefit from more aggressive or novel anticoagulation to decrease their risk of stroke.
Warfarin anticoagulation can decrease the risk of all-cause mortality and stroke in patients with atrial fibrillation (AF) but merely taking the drug does not decrease the risk. Rather, the quality of anticoagulation, as measured by percent time in the therapeutic range (TTR) with a target international normalized ratio (INR) of 2 to 3, has been associated with improved outcomes. We tested the hypothesis that gender differences in risk of ischemic stroke are related to TTR.
Methods
After securing University of Iowa Institutional Review Board and National Institutes of Health approval, data from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) trial were analyzed. This trial included 4,060 patients with AF at risk for stroke, randomized to a rate or rhythm control strategy, to determine if either strategy affected mortality and several secondary end points including stroke. Warfarin anticoagulation (with dose adjustments) was left to physician discretion. AFFIRM was conducted before refinement of risk stratification tools such as CHADS 2 score. For patients in the rhythm control arm, if sinus rhythm was maintained for ≥4 weeks and preferably 12 weeks, warfarin could be discontinued. Although INR evaluation was not a mandatory part of the trial, available INRs were collected at each 4-month visit for a mean of 3.5 years. New transient or permanent neurologic deficits were classified by a member of the AFFIRM stroke events subcommittee who was blinded to randomization arm.
To complete our analyses, we tabulated the incidence of ischemic stroke by gender. We evaluated INR at time of stroke for women and men. We calculated the TTR for each gender using the standard method of Rosendaal based on linear interpolation between 2 INR values for participants taking warfarin who had ≥5 INR values during the study. We related TTR to gender-specific incidence of ischemic stroke.
A chi-square test was used to test the incidence of stroke between women and men. The INR mean, median, and interquartile range was assessed at time of stroke. A t test was used to assess gender differences in TTR. A gender-stratified unadjusted Cox proportional hazard model, based on a pooled analysis of percent TTR, was used to determine how the hazard of ischemic stroke varied according to TTR. A fitted Cox proportional hazard regression model was used to determine the hazard of specific risk factors to the incidence of stroke. SAS 9.2 (SAS Institute, Cary, North Carolina) was used for the analyses.
Results
Baseline characteristics of AFFIRM participants are listed in Table 1 . Nearly 40% were women, randomized equally to rate and rhythm control strategies. Women were older (71.3 ± 7.5 vs 68.3 ± 8.3, p < 0.0001) than men and more likely to be hypertensive (73% vs 69.4%, p = 0.01). There was no difference between women and men regarding history of stroke or transient ischemic attack (13.3% vs 13.4%, p = 0.94). Although not calculated previously in the AFFIRM trial, the CHADS 2 score was found to be higher for women than for men (3.7 ± 1.3 vs 2.5 ± 1.3, p <0.0001). Warfarin use was similar for women and men within their randomization arm over the course of the study.
| Variable | Women | Men | p Value |
|---|---|---|---|
| (n = 1,594) | (n = 2,466) | ||
| Rate control | 51.6% | 48.8% | 0.08 |
| Age (years) | 71.3 ± 7.5 | 68.3 ± 8.3 | <0.0001 |
| CHADS 2 ⁎ | 3.7 ± 1.3 | 2.5 ± 1.3 | <0.0001 |
| Heart failure | 22.5% | 23.6% | 0.42 |
| Hypertension | 73% | 69.4% | 0.01 |
| Age ≥75 years | 34.8% | 21.9% | <0.000001 |
| Diabetes mellitus | 19.1% | 20.6% | 0.25 |
| Stroke/transient ischemic attack | 13.3% | 13.4% | 0.94 |
| Warfarin use—rate | 87% | 86% | 0.7 |
| Warfarin use—rhythm | 71% | 68% | 0.2 |
| Aspirin | 25.1% | 27.6% | 0.07 |
⁎ CHADS 2 score is comprised of 1 point each for congestive heart failure, hypertension, age ≥75 years, diabetes, and 2 points for previous stroke or transient ischemic attack.
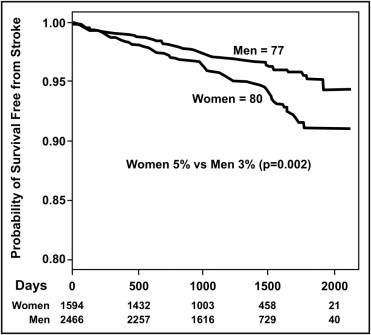
AFFIRM trial participants had 157 first-time ischemic strokes on or off warfarin anticoagulation ( Figure 1 ). Women had 80 ischemic strokes (5% overall incidence) and men had 77 ischemic strokes (3% overall incidence, odds ratio 1.6, 95% confidence interval 1.19 to 2.26, p = 0.002).
INR values were available for 83 participants who were prescribed warfarin at the time of ischemic stroke. The mean INR value was 2 for women (n = 44) and men (n = 39); median INR values were 1.7 (interquartile range 1.4 to 2.3) and 1.8 (interquartile range 1.3 to 2.5), respectively. Participants were excluded from this analysis if they were not prescribed warfarin at the time of first ischemic stroke or if INR values were unavailable. Women spent a greater percent time outside the therapeutic range compared to men (40 ± 0.7% vs 37 ± 0.5%, p = 0.001). Women were more likely to have subtherapeutic INRs (29 ± 0.7% vs 26 ± 0.5%, p = 0.0002; Table 2 ).
| Outside (%) | Below (%) | |
|---|---|---|
| Women (n = 1,499) | 40 ± 0.7 | 29 ± 0.7 |
| Men (n = 2,337) | 37 ± 0.5 | 26 ± 0.5 |
| p value | 0.0001 | 0.0002 |
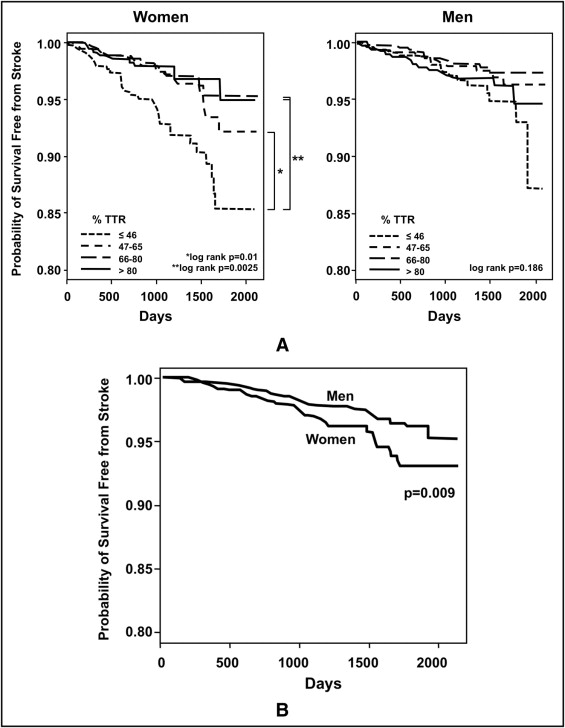
Quartiles of study participants based on a pooled analysis of percent TTR were constructed (first quartile <46%, second quartile 47% to 65%, third quartile 66% to 80%, fourth quartile >80%; Figure 2 ). Hazard ratios for ischemic stroke were lower for each successive quartile of higher TTR for women (p = 0.01 to 0.0025, log-rank test). In comparison, higher TTR was not significantly associated with lower risk of ischemic stroke in men (lowest p = 0.186, log-rank test). Compared to men, women were more likely to have an ischemic stroke even if their TTR was ≥66% (p = 0.009; Figure 2 ). Female gender (hazard ratio 1.54, confidence interval 1.10 to 2.16, p = 0.012) conferred increased risk of ischemic stroke even after adjustment for other clinical factors found related to ischemic stroke ( Table 3 ).