There is little information on the effect of contrast-induced nephropathy (CIN) on long-term mortality after percutaneous coronary intervention in patients with or without chronic kidney disease (CKD). Of 4,371 patients who had paired serum creatinine (SCr) measurements before and after percutaneous coronary intervention and were discharged alive in the Coronary REvascularization Demonstrating Outcome Study in Kyoto registry, the incidence of CIN (an increase in SCr of ≥0.5 mg/dl from the baseline) was 5% in our study cohort. The rate of CIN in patients with CKD was 11%, although it was 2% without CKD (p <0.0001). During a median follow-up of 42.3 months after discharge, 374 patients (8.6%) died. After adjustment for prespecified confounders, CIN was significantly correlated with long-term mortality in the entire cohort (hazard ratio [HR] 2.26, 95% confidence interval [CI] 1.62 to 2.29, p <0.0001) and in patients with CKD (HR 2.62, 95% CI 1.91 to 3.57, p <0.0001) but not in patients without CKD (HR 1.23, 95% CI 0.47 to 2.62, p = 0.6). Sensitivity analyses confirmed these results using the criteria defined as elevations of the SCr by ≥25% and 0.3 mg/dl from the baseline, respectively. In conclusion, CIN was significantly correlated with long-term mortality in patients with CKD but not in those without CKD.
Recent studies have shown that contrast-induced nephropathy (CIN) is the third leading cause of all hospital-acquired renal insufficiency, accounting for 10%. The incidence of CIN in patients with chronic kidney disease (CKD) was reported to be greater compared with that in those without CKD. Although an association between CIN and death was previously suggested, it has not been fully evaluated whether the effect of CIN on long-term mortality is different between patients with CKD and those without CKD. In this report, we sought to clarify the incidence of CIN after percutaneous coronary intervention (PCI) and the effect of CIN on long-term mortality in patients with or without CKD using a large observational database of patients who underwent their first PCI in Japan.
Methods
The Coronary REvascularization Demonstrating Outcome Study in Kyoto (CREDO-Kyoto) is a multicenter registry in Japan that enrolled consecutive patients who underwent their first PCI or coronary artery bypass grafting from January 2000 to December 2002, excluding patients with acute myocardial infarction within a week before the index procedure. The relevant review board or ethics committees in all 30 participating centers approved the research protocol. The study design and patient enrollment of the CREDO-Kyoto registry were previously described in detail.
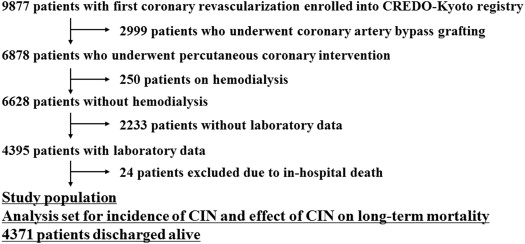
Of the 9,877 patients who underwent PCI or coronary artery bypass grafting enrolled during the study period, we excluded 2,999 patients receiving coronary artery bypass grafting, 250 patients on hemodialysis, and 2,233 patients without paired serum creatinine (SCr) measurements before and after PCI. After excluding 24 patients who died during the index hospitalization, 4,371 patients finally made up the study population to assess the incidence of CIN and effect of CIN on long-term mortality ( Figure 1 ).
Demographic, angiographic, and procedural data were collected from hospital charts or databases in each center by independent clinical research coordinators, as previously described. Follow-up data were obtained from hospital charts or by contacting patients or referring physicians.
In this study, we primarily defined CIN as an increase in the peak SCr concentration of ≥0.5 mg/dl after PCI from the SCr concentration before PCI. We also defined CIN-25% and CIN-0.3 as elevations in the SCr concentration ≥25% and ≥0.3 mg/dl after PCI, respectively, for sensitivity analyses. CKD was defined as an estimated glomerular filtration rate of <60 ml/min/1.73 m 2 using the new equation in Japanese patients.
The primary outcome of this study was all-cause mortality after discharge. We excluded patients with in-hospital death at index PCI because most patients who died during index hospitalization were severely ill on admission and/or after PCI, which predisposed them to acute deterioration of the kidney function related to several factors including CIN.
Categorical variables are expressed as numbers and percentages and were compared using the chi-square test. Continuous variables of each group are presented with the mean ± SD and were compared using the Student t test or Wilcoxon rank-sum test based on their distributions. The cumulative incidence of all-cause death was estimated by the Kaplan-Meier method, and differences were assessed with the log-rank test. The adjusted relationships between CIN and death after discharge were evaluated using Cox proportional hazard models. In the CREDO-Kyoto registry, we previously identified 14 confounders correlated with death after discharge, including age ≥75 years, CKD, hemodialysis, history of heart failure, chronic obstructive lung disease, malignancy, anemia, peripheral vascular disease, stroke, left ventricular dysfunction, body mass index ≤25.0 kg/m 2 , diabetes with insulin, absence of statin use, and use of angiotensin-converting enzyme inhibitors. In this study, we excluded only 1 factor, hemodialysis, and adjusted the mortality with the remaining 13 confounders for analysis of the entire cohort. For the analysis of patients with or without CKD, we adjusted the mortality with the 12 confounders other than hemodialysis and CKD. The results of analyses are shown as the hazard ratio (HR) given with 95% confidence intervals (CIs) and p values. Results were considered significant with a p value of <0.05. We used JMP 8.0 (SAS Institute Inc., Cary, North Carolina) for all analyses. The investigators had full access to the data and take responsibility for its integrity. All the investigators have read and approved the report as written.
Results
Baseline characteristics were significantly different between patients discharged alive and those who died in hospital ( Supplementary Material ). Patients discharged alive were younger and more likely to have a preserved ejection fraction and renal function and a current smoking habit. The in-hospital death group more often had a history of heart failure, diabetes, stroke, anemia, triple-vessel disease, proximal left anterior descending coronary artery disease, and total occlusion. Of the 255 patients who showed an increase in the peak SCr concentration of ≥0.5 mg/dl after PCI from the baseline SCr concentration, 237 patients (93%) were discharged alive.
Of the 4,371 patients discharged alive in the present study, 1,650 patients had CKD. Baseline characteristics were significantly different between patients with CKD and those without CKD ( Table 1 ). The CKD group included more elderly and high-risk patients.
| Variable | Entire Cohort (n = 4371) | Chronic Kidney Disease | p Value ∗ | |
|---|---|---|---|---|
| Yes (n = 1650) | No (n = 2721) | |||
| Age (years) | 67.7 ± 10.3 | 71.6 ± 8.7 | 65.2 ± 10.4 | <0.0001 |
| ≥75 | 1172 (27%) | 630 (38%) | 542 (20%) | <0.0001 |
| ≥80 | 489 (11%) | 316 (19%) | 173 (6.4%) | <0.0001 |
| Female | 1338 (31%) | 563 (34%) | 775 (28%) | <0.0001 |
| Body mass index (kg/m 2 ) | 23.6 (21.6–25.6) | 23.5 (21.4–25.7) | 23.6 (21.8–25.6) | 0.1 |
| >25.0 | 1334 (31%) | 506 (31%) | 828 (30%) | 0.9 |
| Ejection fraction (%) | 62.7 ± 13.2 | 60.7 ± 14.2 | 63.9 ± 12.5 | <0.0001 |
| ≤40% | 262 (6.0%) | 144 (8.7%) | 118 (4.3%) | <0.0001 |
| Heart failure | 586 (13%) | 365 (22%) | 221 (8.1%) | <0.0001 |
| Functional class 3/4 | 199 (4.6%) | 123 (7.5%) | 76 (2.8%) | <0.0001 |
| Prior myocardial infarction | 1042 (24%) | 455 (28%) | 587 (22%) | <0.0001 |
| Atrial fibrillation | 304 (7.0%) | 169 (10%) | 135 (5.0%) | <0.0001 |
| Diabetes mellitus | 1626 (37%) | 616 (37%) | 1010 (37%) | 0.9 |
| Insulin-treated | 327 (7.5%) | 166 (10%) | 161 (5.9%) | <0.0001 |
| Oral drug-treated | 724 (17%) | 263 (16%) | 461 (17%) | 0.4 |
| Hemoglobin A1c (%) | 7.3 ± 1.6 | 7.1 ± 1.4 | 7.4 ± 1.6 | 0.0005 |
| Hypertension | 3036 (69%) | 1247 (76%) | 1789 (66%) | <0.0001 |
| Blood pressure (mm Hg) | ||||
| Systolic | 137.3 ± 22.2 | 138.8 ± 23.6 | 136.4 ± 21.2 | 0.0005 |
| Diastolic | 75.8 ± 13.3 | 75.9 ± 13.4 | 75.7 ± 13.2 | 0.7 |
| Current smoker | 1238 (28%) | 349 (21%) | 889 (33%) | <0.0001 |
| Stroke | 664 (15%) | 315 (19%) | 349 (13%) | <0.0001 |
| Peripheral vascular disease | 271 (6.2%) | 150 (9.1%) | 121 (4.5%) | <0.0001 |
| Chronic pulmonary disease | 118 (2.7%) | 56 (3.4%) | 62 (2.3%) | 0.03 |
| Malignancy | 307 (7.0%) | 137 (8.3%) | 170 (6.3%) | 0.01 |
| Baseline renal function | ||||
| Serum creatinine (mg/dL) | 0.94 ± 0.51 | 1.26 ± 0.70 | 0.74 ± 0.14 | <0.0001 |
| Estimated glomerular filtration rate (mL/min/1.73 m 2 ) | 65.9 ± 21.7 | 45.7 ± 11.7 | 78.2 ± 16.5 | |
| <30 mL/min/1.73 m 2 | 180 (4.1%) | 180 (11%) | 0 (0%) | |
| Anemia | 959 (22%) | 551 (33%) | 408 (15%) | <0.0001 |
| Emergency procedure | 298 (6.8%) | 98 (5.9%) | 200 (7.4%) | 0.07 |
| Triple vessel coronary disease | 996 (23%) | 461 (28%) | 535 (20%) | <0.0001 |
| Left main coronary artery narrowing | 103 (2.4%) | 42 (2.6%) | 61 (2.2%) | 0.5 |
| Proximal left anterior descending coronary artery narrowing | 1624 (37%) | 655 (40%) | 969 (36%) | 0.007 |
| Total coronary occlusion | 1095 (25%) | 463 (28%) | 632 (23%) | 0.0004 |
| Treatment of ≥2 vessels | 1069 (24%) | 440 (27%) | 629 (23%) | 0.008 |
| Number of target vessels | 1 (1–1) | 1 (1–2) | 1 (1–1) | 0.009 |
| 1.27 ± 0.53 | 1.30 ± 0.54 | 1.26 ± 0.52 | ||
| Medication at hospital discharge | ||||
| Statins | 1423 (33%) | 518 (31%) | 905 (33%) | 0.2 |
| Aspirin | 3861 (88%) | 1427 (86%) | 2434 (89%) | 0.003 |
| Thienopyridines | 3400 (78%) | 1253 (76%) | 2147 (79%) | 0.02 |
| Angiotensin-converting enzyme inhibitors | 1161 (27%) | 487 (30%) | 674 (25%) | 0.0006 |
| Angiotensin-II receptor antagonists | 640 (15%) | 289 (18%) | 351 (13%) | <0.0001 |
| Beta-blockers | 892 (20%) | 362 (22%) | 530 (19%) | 0.05 |
| Calcium channel blockers | 2476 (57%) | 936 (57%) | 1540 (57%) | 0.9 |
| Nitrates | 3127 (72%) | 1157 (70%) | 1970 (72%) | 0.1 |
In our study population, the incidence of CIN was 5% in the entire cohort. The incidence of CIN was significantly greater in patients with CKD than in those without CKD (11% vs 2%, p <0.0001; Table 2 ).
| Definition of CIN | Entire Cohort (n = 4371) | Chronic Kidney Disease | p Value ∗ | |
|---|---|---|---|---|
| Yes (n = 1650) | No (n = 2721) | |||
| CIN | 237 (5%) | 181 (11%) | 56 (2%) | <0.0001 |
| CIN-25% | 943 (22%) | 341 (21%) | 602 (22%) | 0.3 |
| CIN-0.3 | 604 (14%) | 362 (22%) | 242 (9%) | <0.0001 |
The baseline clinical characteristics of patients who developed CIN revealed a high prevalence of the high-risk factors, such as advanced age, heart failure, insulin-treated diabetes, CKD, and triple-vessel disease ( Supplementary Material ).
During a median follow-up of 42.3 months (interquartile range 31.4 to 52.0) after discharge, 374 patients (8.6%) died.
The unadjusted survival probability of patients with CIN was significantly less than that of patients without CIN in the entire cohort ( Figure 2 ). In patients with CKD, the unadjusted survival rate of patients with CIN was significantly lower compared with that of those without CIN ( Figure 2 ), whereas it was not significantly different in patients without CKD ( Figure 2 ).




