Whether the association between platelet count (PC) and thrombotic and bleeding risk is independent of or varies by residual platelet reactivity to antiplatelet therapies is unclear. We sought to investigate the independent and combined effects of PC and platelet reactivity on thrombotic and bleeding risk after coronary artery implantation of drug-eluting stents (DES). Patients enrolled in the prospective, multicenter Assessment of Dual AntiPlatelet Therapy with Drug-Eluting Stents study were stratified by PC tertiles. The study cohort comprised 8,402 patients. By linear regression analysis, lower PC was strongly and independently associated with higher platelet reactive units (PRUs) on clopidogrel. After multivariable adjustment (including PRU and aspirin reactive units), high, but not low, PC tertile was independently associated with higher risk of thrombotic complications, including spontaneous myocardial infarction and stent thrombosis. Although no independent association was observed between PC tertiles and hemorrhagic risk, both high and low PC tertiles were associated with increased risk for all-cause mortality. After stratification of PC tertiles by tertiles of PRUs, the crude risk of thrombotic complications was highest in patients in the high PC and high PRU tertiles. By multivariable adjustment, PRU increases were uniformly associated with higher risk of thrombotic events across PC tertiles, without evidence of interaction. In conclusion, higher PCs and higher PRUs act independently and synergistically in determining thrombotic risk. Alongside PRU, PCs could be a simple hematological parameter to consider for risk stratification and in tailoring duration and potency of pharmacologic platelet inhibition after DES implantation.
Platelets are highly specialized blood cellular components developed in mammals to promote hemostasis and blood vessel repair. However, platelet activation and aggregation is a key component of pathologic arterial thrombosis in the presence of native ulcerated atherosclerotic plaques (causing atherothrombosis) or partially endothelialized intracoronary stents (causing stent thrombosis [ST]). Therefore, an accurate control of platelet activity by means of tailored pharmacologic platelet inhibition is desirable to maintain coagulation homeostasis and to prevent thrombotic complications without increasing bleeding risk. P2Y 12 reaction units (PRUs) independently correlate with both thrombosis and bleeding risk. Dual antiplatelet therapy (DAPT) with aspirin and a P2Y 12 receptor inhibitor is, to date, the main therapeutic option to prevent coronary thrombotic complications in patients undergoing percutaneous coronary intervention (PCI) with drug-eluting stents (DES). Platelet count (PC) has been previously described as an important predictor of adverse events across the entire clinical spectrum of coronary artery disease (CAD) managed with PCI. Whether the association between PC and thrombotic and bleeding risk is independent or is modulated by residual platelet reactivity on clopidogrel has not yet been explored. Therefore, in the present post hoc analysis from the large, all-comers Assessment of Dual AntiPlatelet Therapy with Drug-Eluting Stents (ADAPT-DES) study, we sought to evaluate the relation between PC and PRU and their combined and independent effect on thrombotic and bleeding outcomes after intracoronary DES implantation.
Methods
ADAPT-DES was a prospective, nonrandomized, international, multicenter study designed to determine the incidence, timing, and predictors of ST after DES implantation. The major exclusion criteria were the occurrence of a serious adverse event during PCI or before platelet reactivity testing and planned bypass surgery after PCI. All patients received aspirin and clopidogrel before PCI. Platelet function tests were performed after successful PCI the day after the procedure by means of the VerifyNow Aspirin, P2Y12, and IIb/IIIa assays (Accumetrics, San Diego, California). After PCI, aspirin was recommended indefinitely in all patients, and clopidogrel was recommended for at least 1 year. Clinical follow-up was carried out at 30 days, 1 year, and 2 years by means of telephone contact. The study was approved by the institutional review board at each participating center, and all eligible patients signed written informed consent. The study was monitored by an independent committee during its entire duration. Study monitors traveled regularly among enrolling centers to evaluate the accuracy of data entry and adverse event reporting. An independent committee of 3 physicians routinely met to adjudicate ST, myocardial infarction (MI), and deaths through clinical chart review and other additional data when needed. Conversely, bleeding was not adjudicated by an independent committee.
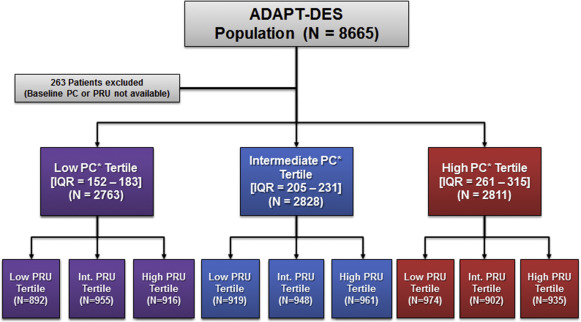
For the present investigation, the ADAPT-DES population was stratified according to PC tertiles ( Figure 1 ). Patients with baseline PC <100,000/mm 3 were excluded from the ADAPT-DES study, as it was demonstrated to interfere with the VerifyNow P2Y12 test.
The objectives of the present post hoc analysis from the ADAPT-DES study were to investigate the unadjusted and adjusted relation between PC and PRU and to evaluate the combined and independent effect of PC and PRU on 2-year thrombotic, hemorrhagic, and mortality risk. Thrombotic end points included definite or probable ST, MI, and the composite of cardiac death, MI, or ST (major adverse cardiac events [MACE]). Bleeding end points included non–coronary artery bypass graft-related major bleeding. Mortality end points included all-cause mortality and cardiac mortality. Outcomes were reported at 2-year follow-up. End point definitions used in the ADAPT-DES study have been previously described.
Categorical variables were reported as percentage and compared by the chi-square test or Fisher’s exact test, when appropriate. Continuous variables are reported as mean and SD and compared by analysis of variance. Crude event-free survival was reported through Kaplan–Meier estimates and compared with the log-rank test. The adjusted association between PC and PRU was estimated using a multivariate linear regression analysis and reported with the standardized estimate and SD; the adjusted association between PC and PRU >208 (high platelet reactivity) was estimated with logistic regression analysis and reported with odds ratio and 95% CI. For the logistic regression models, covariates were chosen by stepwise selection procedure with 0.1 entry and removal criteria. Baseline PC (100 k/mm 3 increase) was forced into the model. The adjusted associations between PC tertiles and 2-year outcomes were estimated by means of Cox proportional hazard regression models selected by a stepwise process with entry and exit thresholds set to 0.1; intermediate PC was set as the reference group (full list of candidate covariates is included in the table footnotes). An interaction testing was performed to explore the effect of PRU (per 50 units increase) on outcomes across PC tertiles. Schoenfeld residuals were assessed to verify that the proportional hazards assumption was satisfied. A p value of <0.05 was considered statistically significant. SAS, version 9.4 (SAS Institute, Cary, North Carolina) was used to carry out the statistical analysis.
Results
Overall, 8,402 patients were included in the study cohort. Of them, 2,763 (32.9%), 2,828 (33.7%), and 2,811 patients (33.5%) were distributed across the lowest, intermediate, and highest PC tertile, respectively. PC interquartile range in the lowest tertile was 152 to 183, in the intermediate was 205 to 231, and in the highest was 261 to 315 (per 10 3 /mm 3 ). Baseline clinical characteristics are described in Table 1 . Patients in the low tertile were older, more commonly men, of Caucasian ethnicity and with a higher prevalence of cardiovascular and noncardiovascular co-morbidities. Patterns of clinical manifestations of CAD varied across the study groups. Asymptomatic CAD and stable angina were more common in patients in the low PC tertile. Conversely, acute CAD presentations were more prevalent in patients in the high PC tertile. Procedural data are reported in Table 2 . Patients in the low PC tertile more commonly had calcified lesions, had more vessels treated, received more stents, and had a higher final stent length. Conversely, patients in the high PC tertile had more thrombotic lesions and lower Thrombolysis In Myocardial Infarction flow grade at baseline.
| Variable | Low tertile IQR = 152–183 (n=2763) | Intermediate tertile IQR = 205–231 (n=2828) | High tertile IQR = 261–315 (n=2811) | p value ∗ |
|---|---|---|---|---|
| Age (years) | 66.1 ± 10.3 | 63.2 ± 10.8 | 61.7 ± 10.9 | <0.0001 |
| Men | 2334 (84.5%) | 2118 (74.9%) | 1801 (64.1%) | <0.0001 |
| Caucasian | 2481 (89.8%) | 2118 (74.9%) | 1801 (64.1%) | 0.01 |
| Non-caucasian | 282 (10.2%) | 319 (11.3%) | 349 (12.4%) | 0.01 |
| Body mass index (kg/m 2 ) | 29.3 ± 5.3 | 29.4 ± 5.6 | 29.7 ± 6.2 | 0.012 |
| Diabetes mellitus | 955 (34.6%) | 881 (31.2%) | 887 (31.6%) | 0.01 |
| Insulin-dependent | 350 (12.7%) | 289 (10.2%) | 338 (12.0%) | 0.11 |
| Peripheral artery disease | 336 (12.2%) | 259 (9.2%) | 264 (9.4%) | <0.0001 |
| Congestive heart failure | 299 (10.8%) | 199 (7.0%) | 189 (6.7%) | <0.0001 |
| Previous myocardial infarction | 787 (28.5%) | 707 (25.0%) | 627 (22.3%) | <0.0001 |
| Previous coronary bypass | 638 (23.1%) | 459 (16.2%) | 338 (12.0%) | <0.0001 |
| Previous percutaneous coronary intervention | 1315 (47.6%) | 1217 (43.0%) | 1076 (38.3%) | <0.0001 |
| Arterial hypertension | 2266 (82.0%) | 2264 (80.1%) | 2170 (77.2%) | <0.0001 |
| Chronic kidney disease † | 501 (18.2%) | 433 (15.3%) | 433 (15.4%) | 0.002 |
| Anemia ‡ | 699 (25.3%) | 550 (19.5%) | 566 (20.1%) | <0.0001 |
| Hyperlipidemia | 2181 (78.9%) | 2114 (74.8%) | 1977 (70.3%) | <0.0001 |
| Current smoker | 482 (17.4%) | 637 (22.5%) | 786 (28.0%) | |
| Previous smoker | 1023 (37.0%) | 978 (34.6%) | 826 (29.4%) | |
| Clinical presentation | ||||
| Asymptomatic coronary artery disease | 397 (14.4%) | 324 (11.5%) | 330 (11.7%) | 0.0006 |
| Stable angina pectoris | 841 (30.4%) | 889 (31.4%) | 735 (26.2%) | 0.01 |
| Unstable angina pectors | 796 (28.8%) | 770 (27.3%) | 743 (26.4%) | 0.04 |
| Non-STEMI | 390 (14.1%) | 392 (13.9%) | 435 (15.5%) | 0.30 |
| STEMI | 193 (7.0%) | 245 (8.7%) | 341 (12.1%) | <0.0001 |
| NYHA II–IV Class | 1942 (70.3%) | 1896 (67.0%) | 1821 (64.8%) | <0.0001 |
| Ejection fraction (%) | 53.9 ± 12.4 | 54.9 ± 12.4 | 55.8 ± 12.3 | <0.0001 |
| White blood cell count (K/mL) | 7.1 ± 3.0 | 7.9 ± 3.4 | 8.9 ± 2.9 | <0.0001 |
| VerifyNow testing results | ||||
| Platelet reactivity units | 190.3 ± 93.7 | 188.9 ± 95.5 | 184.4 ± 100.9 | 0.06 |
| ≥230 | 960 (34.7%) | 1000 (35.4%) | 982 (34.9%) | 0.77 |
| >208 | 1191 (43.1%) | 1214 (42.9%) | 1183 (42.1%) | 0.51 |
| Aspirin reactivity units | 432.0 ± 63.1 | 416.5 ± 52.2 | 409.3 ± 46.9 | <0.0001 |
| ≥550 | 249 (9.1%) | 137 (4.9%) | 84 (3.0%) | <0.0001 |
† Creatinine clearance <60 ml/min.
| Variable | Low tertile IQR = 152–183 (n=2763) | Intermediate tertile IQR = 205–231 (n=2828) | High tertile IQR = 261–315 (n=2811) | p value ∗ |
|---|---|---|---|---|
| Femoral access site | 2621 (94.9%) | 2707 (95.7%) | 2682 (95.4%) | 0.20 |
| Thrombotic lesion | 328 (11.9%) | 414 (14.6%) | 493 (17.5%) | <0.0001 |
| Calcific lesion | 937 (33.9%) | 891 (31.5%) | 776 (27.6%) | <0.0001 |
| Bifurcation lesion | 457 (16.5%) | 420 (14.9%) | 422 (15.0%) | 0.07 |
| Chronic total occlusion | 146 (5.3%) | 126 (4.5%) | 126 (4.5%) | 0.11 |
| Lesion within a graft | 190 (6.9%) | 127 (4.5%) | 104 (3.7%) | <0.0001 |
| In-stent restenotic lesion | 296 (10.7%) | 300 (10.6%) | 286 (10.2%) | 0.58 |
| TIMI flow (pre-procedure) 0/1 | 234 (8.5%) | 243 (8.6%) | 293 (10.4%) | 0.04 |
| TIMI flow (post-procedure) 3 | 2748 (99.5%) | 2802 (99.1%) | 2795 (99.4%) | 0.49 |
| Stents implanted per patient | 1.8 ± 1.1 | 1.7 ± 1.0 | 1.7 ± 1.0 | 0.008 |
| Lesions treated per patient | 1.5 ± 0.8 | 1.5 ± 0.8 | 1.5 ± 0.7 | 0.02 |
| Vessels treated per patient | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 0.009 |
| Total lesion length (mm) | 27.6 ± 20.6 | 27.2 ± 20.3 | 26.5 ± 19.4 | 0.13 |
| Total stent length (mm) | 33.1 ± 22.8 | 32.5 ± 22.6 | 31.9 ± 21.9 | 0.15 |
| DES type | ||||
| New-generation drug-eluting stent | 1818 (63.1%) | 1762 (63.2%) | 1827 (63.7%) | 0.62 |
| Early-generation drug-eluting stent | 785 (27.3%) | 766 (27.5%) | 739 (25.8%) | 0.21 |
Results from the P2Y12 VerifyNow tests are reported in Table 1 and Figure 2 . After multivariate adjustment for baseline covariates, PC (for each decrease of 100,000/mm 3 ) was significantly and inversely associated with high on-clopidogrel platelet reactivity using a cutoff of >208 (adjusted odds ratio 1.19, 95% CI 1.11 to 1.28; p <0.0001). Results were similar using a PRU cutoff of ≥230. The association between PC and PRU remained strong after multivariate linear regression analysis, with increases in PC inversely related to PRU (−10.83 ± 1.91; p <0.0001). Patients in the low PC tertile had also the highest values of mean aspirin reaction units (432.0 ± 63.1 vs 416.5 ± 52.2 vs 409.3 ± 46.9; p <0.0001).
Unadjusted 2-year event rates across PC tertiles are reported in Table 3 . After adjustment for clinical and procedural covariates, including PRU and aspirin reactive units, high PC was associated with a significantly higher risk of MI (adjusted hazard ratio 1.47, 95% CI 1.1 to 2.0; p = 0.01) and MACE (adjusted hazard ratio 1.41, 95% CI 1.1 to 1.8; p = 0.008), and a trend to higher risk of ST ( Table 4 ; adjusted hazard ratio 1.75, 95% CI 1.0 to 3.1; p = 0.053). The effects of higher PCs were consistent between patients presenting with ST-segment elevation MI and all others clinical presentations, without evidence of interaction. We observed no significant associations between high or low PCs and risk of major bleeding. Both low and high PC tertiles were associated with a higher risk of all-cause mortality ( Table 4 ). Finally, results remained consistent after inclusion of DAPT status as time-dependent covariate in the multivariate model.
| Variable | Low tertile IQR = 152–183 (n=2763) | Intermediate tertile IQR = 205–231 (n=2828) | High tertile IQR = 261–315 (n=2811) | Trend p value ∗ |
|---|---|---|---|---|
| All-cause death | 132 (4.7%) | 81 (3.0%) | 100 (3.8%) | 0.007 |
| Cardiac death | 71 (2.7%) | 41 (1.5%) | 53 (2.0%) | 0.01 |
| Major adverse cardiac events † | 187 (7.1%) | 148 (5.4%) | 182 (6.8%) | 0.04 |
| Stent thrombosis ‡ | 26 (1.0%) | 24 (0.9%) | 41 (1.5%) | 0.05 |
| Myocardial infarction | 129 (4.9%) | 111 (4.1%) | 143 (5.4%) | 0.10 |
| Peri-procedural | 36 (1.3%) | 48 (1.7%) | 42 (1.5%) | 0.48 |
| Spontaneous | 94 (3.6%) | 64 (2.4%) | 102 (3.9%) | 0.006 |
| Major bleeding | 253 (9.5%) | 248 (9.2%) | 220 (8.2%) | 0.19 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


