The neutrophil-to-lymphocyte ratio (NLR) has been proved as a reliable inflammatory marker for the atherosclerotic process and as a predictor for clinical outcomes in patients with various cardiovascular diseases. A recent study reported that elevated NLR is associated with impaired myocardial perfusion in patients with ST-segment elevation myocardial infarction (STEMI). We investigated whether NLR is associated with coronary microcirculation as assessed by the index of microcirculatory resistance (IMR) in patients with STEMI who had undergone primary percutaneous coronary intervention (PCI). A total of 123 patients with STEMI who underwent successful primary PCI were enrolled in this study. NLR was obtained on admission, and patients were divided into 3 groups by NLR tertile. IMR was measured using an intracoronary thermodilution-derived method immediately after index PCI. Symptom onset-to-balloon time was significantly longer (p = 0.005), and IMR was significantly higher in the high NLR group than that in the low and intermediate groups (21.94 ± 12.87 vs 23.22 ± 12.73 vs 32.95 ± 20.60, p = 0.003). Furthermore, in multiple linear regression analysis, NLR showed an independent positive correlation with IMR ( r = 0.205, p = 0.009). In conclusion, NLR has shown positive correlation with IMR, whereas negative association with infarct-related artery patency in patients with STEMI who underwent primary PCI. Therefore, NLR at admission could reflect myocardial damage and the status of coronary microcirculation in patients with STEMI ( ClinicalTrials.gov number, NCT02828137 ).
It has been shown that the inflammatory process plays a central role in the stages of atherosclerosis. Inflammation is associated with early phase atherogenesis, progression of atherosclerosis, atherosclerotic plaque destabilization, and the development of thrombosis in cardiovascular disease. At present, the white blood cell (WBC) count and its subtypes are known to be inflammatory markers and are associated with increased cardiovascular risk, as well as predicting clinical outcomes of coronary artery disease. Previous studies have found that the neutrophil-to-lymphocyte ratio (NLR) is a reliable inflammatory biomarker for the atherosclerotic process and a predictor for clinical outcomes in patients with various cardiovascular diseases. Furthermore, recent studies have reported that elevated NLR is associated with a lower prevalence of infarct-related artery (IRA) patency in patients with ST-segment elevation myocardial infarction (STEMI). However, sufficient evidence demonstrating the relation between NLR and coronary microcirculatory function has not yet been presented. Therefore, we sought to investigate whether NLR is associated with the status of microvascular function as assessed by the index of microcirculatory resistance (IMR) in patients with STEMI who had undergone primary percutaneous coronary intervention (PCI).
Methods
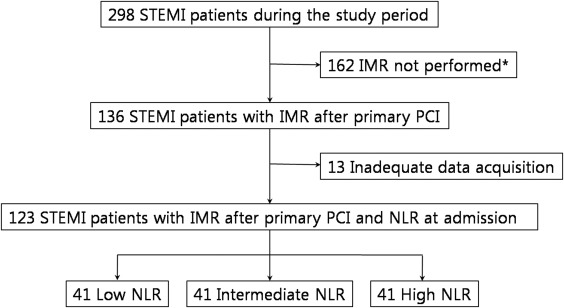
The study protocol was approved by the Institutional Review Board of Inha University Hospital, Inha University College of Medicine (INHAUH 2016-06-012), and written consent was obtained from each patient. A total of 123 consecutive patients with STEMI who underwent successful primary PCI and coronary physiologic study immediately after PCI from May 2009, to October 2014, at Inha University Hospital were retrospectively enrolled in this study ( Figure 1 ). STEMI was defined using current guidelines. Patients with medical conditions that could affect the total or differential WBC counts (such as hematologic disorders, malignancies, a history of chemotherapy or radiation therapy, evidence of inflammatory or infectious diseases, and use of corticosteroids) were excluded from the study. Patients with unprotected left main coronary artery disease, stent thrombosis presentation, a history of coronary artery bypass graft surgery, previous intravenous thrombolytic therapy before PCI, high-degree atrioventricular block, persistent cardiogenic shock after PCI, contraindication for the use of adenosine, and post-PCI Thrombolysis In Myocardial Infarction (TIMI) flow grades 0 or 1 were also excluded from this study. This study is registered on ClinicalTrials.gov under the identifier NCT02828137 .
Complete blood counts including total and differential WBC counts were obtained at the time of admission. Total counts for WBCs, neutrophils, and lymphocytes were assessed using an automated blood cell counter (XE-2100; Sysmex Inc., Kobe, Japan). NLR was calculated as the ratio of the neutrophil-to-lymphocyte counts. All patients received a loading dose of aspirin (300 mg) and P2Y12 inhibitors: clopidogrel (600 mg) or ticagrelor (180 mg). A heparin bolus (5,000 U) was administered intravenously at the time of admission before transfer to the catheter laboratory. An additional heparin bolus was administered after arterial puncture where necessary. The use of aspiration thrombectomy or glycoprotein IIb/IIIa inhibitor was left to the physician’s discretion. TIMI flow grades were rated as grades 0 to 3 based on pre- and post-PCI cine images. The IMR, fractional flow reserve, and coronary flow reserve were assessed shortly after primary PCI using a thermodilution-derived method with a coronary pressure guidewire (Radi Pressure Wire 5; Radi Medical Systems, Uppsala, Sweden). A baseline transthoracic echocardiogram was performed within 24 hours of primary PCI.
Continuous variables are presented as the mean ± SD and one-way analysis of variance was used for analysis. Categorical variables are presented as the number of patients (percentages) and Pearson’s chi-square or Fisher’s exact tests were used for analysis. Linear regression analysis was performed to investigate the association between NLR and variables using clinical, laboratory, echocardiographic, and angiographic data. A p value <0.05 was considered statistically significant. All statistical analyses were performed using SPSS, version 19.0 (SPSS Inc., Chicago, Illinois).
Results
Baseline characteristics according to NLR tertiles are presented in Table 1 . WBC counts were significantly higher in the high NLR group than those in the low and intermediate NLR groups. Cardiac biomarker levels were also higher in the high NLR group than those in the low and intermediate NLR groups. Angiographic and coronary physiological data based on all 3 NLR groups are presented in Table 2 . Pre-PCI TIMI flow grade 0 showed a gradually higher frequency according to NLR tertiles ( Figure 2 ). In addition, post-PCI TIMI flow grade 3 showed a gradually lower frequency by NLR group ( Figure 2 ). Door-to-balloon time was found to be similar in all NLR groups ( Table 2 ). However, symptom onset-to-balloon time (STB) was significantly longer in the high NLR group than that in the low and intermediate NLR groups ( Figure 3 ). The hyperemic mean transit time revealed significantly increased prolongation in the high NLR group compared with the low and intermediate NLR groups ( Table 2 ). Although the fractional flow reserve and coronary flow reserve values did not differ among the 3 groups, IMR was significantly elevated in the high NLR group compared with the low and intermediate NLR groups ( Figure 3 ). The relations between NLR and parameters are presented in Table 3 . Simple linear regression analyses revealed that NLR showed good linear positive correlation with STB and IMR ( Figures 4 ). Moreover, multiple linear regression stepwise analysis showed that NLR was independently correlated with WBC count, STB, post-PCI TIMI flow grade 3, and IMR (r = 0.647, p <0.001; Table 3 ).
| Variables | Neutrophil-to-Lymphocyte Ratio | p-value | ||
|---|---|---|---|---|
| < 1.78 (n=41) | 1.78 – 3.90 (n=41) | > 3.90 (n=41) | ||
| Age (years) | 55 ± 10 | 55 ± 11 | 58 ± 12 | 0.290 |
| Men | 35 (85%) | 37 (90%) | 38 (93%) | 0.666 |
| Systolic blood pressure (mmHg) | 127 ± 19 | 127 ± 17 | 134 ± 25 | 0.370 |
| Diastolic blood pressure (mm Hg) | 78 ± 15 | 78 ± 12 | 86 ± 15 | 0.105 |
| Heart rate (beats per minute) | 74 ± 12 | 76 ± 19 | 78 ± 15 | 0.597 |
| Hypertension | 16 (39%) | 22 (54%) | 21 (51%) | 0.364 |
| Diabetes mellitus | 10 (24%) | 13 (32%) | 12 (29%) | 0.756 |
| Dyslipidemia | 18 (44%) | 20 (49%) | 16 (39%) | 0.673 |
| Smoke | 32 (78%) | 26 (63%) | 28 (68%) | 0.339 |
| White blood cell (x 10 9 /L) | 10.84 ± 2.52 | 10.90 ± 4.00 | 13.17 ± 4.28 | 0.006 |
| Hemoglobin (g/dL) | 15.1 ± 1.6 | 15.0 ± 1.6 | 15.3 ± 1.5 | 0.809 |
| Platelets (x10 9 /L) | 265.32 ± 66.59 | 253.18 ± 84.34 | 238.10 ± 53.27 | 0.208 |
| Mean platelet volume (fL) | 7.86 ± 0.85 | 7.95 ± 1.06 | 7.87 ± 0.74 | 0.872 |
| Neutrophil (%) | 46.7 ± 7.1 | 64.8 ± 5.2 | 81.4 ± 5.2 | < 0.001 |
| Lymphocyte (%) | 43.1 ± 6.8 | 25.8 ± 4.4 | 12.7 ± 3.8 | < 0.001 |
| NLR | 1.13 ± 0.33 | 2.63 ± 0.67 | 7.43 ± 3.87 | < 0.001 |
| High sensitivity C-reactive protein (mg/dl) | 0.17 ± 0.17 | 0.39 ± 0.92 | 0.38 ± 0.77 | 0.283 |
| Peak creatine kinase (IU/L) | 2493.5 ± 2347.5 | 2745.4 ± 2743.6 | 3789.5 ± 2278.0 | 0.045 |
| Peak creatine kinase-MB (ng/ml) | 219.7 ± 166.1 | 224.7 ± 191.6 | 339.6 ± 248.5 | 0.015 |
| Peak troponin I (ng/ml) | 78.5 ± 87.7 | 97.7 ± 84.0 | 115.2 ± 91.5 | 0.208 |
| Left ventricular ejection fraction (%) | 46.8 ± 6.0 | 46.5 ± 6.1 | 44.1 ± 6.3 | 0.094 |
| Wall motion score index | 1.48 ± 0.30 | 1.47 ± 0.30 | 1.60 ± 0.29 | 0.100 |
| Variables | Neutrophil-to-Lymphocyte Ratio | p-value | ||
|---|---|---|---|---|
| < 1.78 (n=41) | 1.78 – 3.90 (n=41) | > 3.90 (n=41) | ||
| Door to balloon time (minutes) | 82 ± 88 | 83 ± 55 | 84 ± 53 | 0.991 |
| Symptom onset to balloon time (minutes) | 175 ± 157 | 286 ± 305 | 360 ± 269 | 0.005 |
| Culprit coronary artery | 0.020 | |||
| Left anterior descending | 33 (80%) | 21 (51%) | 29 (71%) | |
| Left circumflex | 4 (10%) | 8 (20%) | 1 (2%) | |
| Right | 4 (10%) | 12 (29%) | 11 (27%) | |
| Mutivessel disease | 18 (44%) | 17 (41%) | 15 (37%) | 0.790 |
| Aspiration thrombectomy | 20 (49%) | 22 (54%) | 19 (46%) | 0.796 |
| Use of glycoprotein IIb/IIIa inhibitor | 10 (24%) | 10 (24%) | 7 (17%) | 0.652 |
| Stent diameter (mm) | 3.10 ± 0.27 | 3.17 ± 0.41 | 3.01 ± 0.32 | 0.095 |
| Stent length (mm) | 27.20 ± 11.91 | 26.28 ± 8.69 | 25.32 ± 8.31 | 0.686 |
| Pre-PCI thrombolysis in myocardial infarction flow grade | 0.027 | |||
| 0 | 7 (17%) | 15 (37%) | 20 (49%) | |
| 1 | 16 (39%) | 12 (29%) | 11 (27%) | |
| 2 | 11 (27%) | 13 (32%) | 8 (19%) | |
| 3 | 7 (17%) | 1 (2%) | 2 (5%) | |
| Post-PCI thrombolysis in myocardial infarction flow grade | 0.026 | |||
| 0/1 | 0 | 0 | 0 | |
| 2 | 2 (5%) | 7 (17%) | 11 (27%) | |
| 3 | 39 (95%) | 34 (83%) | 30 (73%) | |
| Hyperemic aortic pressure (mm Hg) | 86.4 ± 16.7 | 83.0 ± 12.9 | 87.8 ± 17.6 | 0.382 |
| Hyperemic distal coronary pressure (mm Hg) | 79.2 ± 15.2 | 77.6 ± 13.6 | 80.7 ± 16.3 | 0.651 |
| Baseline mean transit time (seconds) | 0.52 ± 0.39 | 0.54 ± 0.27 | 0.66 ± 0.36 | 0.116 |
| Hyperemic mean transit time (seconds) | 0.28 ± 0.17 | 0.30 ± 0.16 | 0.43 ± 0.30 | 0.005 |
| Fractional flow reserve | 0.91 ± 0.06 | 0.93 ± 0.07 | 0.91 ± 0.09 | 0.235 |
| Coronary flow reserve | 1.92 ± 1.04 | 1.99 ± 1.01 | 1.85 ± 1.08 | 0.819 |
| Index of microcirculatory resistance (U) | 21.94 ± 12.87 | 23.22 ± 12.73 | 32.95 ± 20.60 | 0.003 |




