Coronary collateral circulation is an alternative source of blood supply to the myocardium in the presence of chronic total coronary occlusion (CTO). C-X-C motif chemokine receptor 4 (CXCR4) signaling usually contributes to neovascularization. Here, we investigate the relation between CXCR4 levels in peripheral blood CD34+ cells and the formation of angiographic coronary collaterals and determine the risk factors that affect CXCR4 expression in patients with CTO. Demographic, biochemical, and angiographic variables were collected from 324 patients with CTO and 90 negative controls. The presence and extent of collaterals were scored according to the Rentrop scoring system (Rentrop’s). CXCR4 levels and plasma biochemical factors were detected. Clinical outcomes were collected during a 12-month follow-up. Results show that low (Rentrop’s 0 or 1) and high (Rentrop’s of 2 or 3) coronary collateralizations were detected in 183 and 141 patients, respectively. The Rentrop scores were positively correlated with CXCR4 levels in patients with CTO. Patients with low CXCR4 expression exhibited worse clinical outcomes compared with those with high CXCR4 expression. Univariate correlation analysis revealed that age of ≥65 years, women, diabetes, increased plasma level of high-sensitivity C-reactive protein (hs-CRP), and N-terminal brain-type natriuretic peptide were associated with low CXCR4 levels. In conclusion, CXCR4 levels were positively correlated with the presence and extent of angiographic coronary collaterals in patients with CTO. Elder age, women, diabetes, increased plasma level of high-sensitivity C-reactive protein, and N-terminal brain-type natriuretic peptide may be risk factors of CXCR4 expression.
In the human heart, well-developed coronary collaterals serve as a conduit, bridging significantly stenotic or occluded coronary vessels, are capable of improving clinical prognosis in patients with chronic total coronary occlusion (CTO). The extent of coronary collateralization differs greatly among patients and is affected by multiple clinical, angiographic, biochemical factors, and inflammatory cytokines. Chemokine stromal-derived factor (SDF)-1 and its unique receptor C-X-C motif chemokine receptor 4 (CXCR4) were reported and play an important role in postnatal vasculogenesis and normal cardiovascular development. Very recent studies show that the CXCR4 receptor is essentially involved in the stem cell function and may modulate the dual stem cell therapy after myocardial infarction (MI). Therefore, in this study, we investigated the relation between CXCR4 levels in peripheral blood CD34+ cells and the formation of angiographic coronary collaterals in patients with CTO, and the risk factors that affected CXCR4 expression were also determined.
Methods
This study was approved by the Ethical Committee of the First Affiliated Hospital of Xi’an Jiaotong University, China. All patients provided written informed consent to participate after a full explanation of the study. From March 2010 to September 2012, 324 consecutive patients with chronic total occlusion (2 to 12 weeks) of at least 1 major epicardial coronary artery with Thrombolysis In Myocardial Infarction grade 0 to 1 blood flow and 90 controls with coronary artery disease (CAD) but without CTO in the corresponding period were recruited at the First Affiliated Hospital of Xi’an Jiaotong University. The duration of CTO was estimated from the date of occurrence of MI in the area of myocardium supplied by the occluded vessel, from an abrupt worsening of existing angina pectoris, or from information obtained from a previous angiogram. CAD was diagnosed according to the criteria recommended by the American College of Cardiology/American Heart Association. Patients with co-morbidities such as cancer or with immunological diseases or a serious liver, renal, hematological, or neurological disorder, or those who had received coronary intervention or coronary artery bypass surgery before were excluded from the study. The participants were all the Chinese Han population in an attempt to provide a genetic and environmental background that was similar to the patient population. Baseline demographic, biochemical, and angiographic features were recorded for each patient.
All subjects underwent blood collection of the cubital vein and laboratory testing. For patients, aspirin (100 mg) and clopidogrel (600 mg) were administered at the time of coronary angiography. Aspirin (300 mg/day) was administered for at least 3 days, followed subsequently by a daily maintenance dose of 100 mg. Clopidogrel (150 mg/day) was administered for at least 12 months after the intervention. Unfractionated heparin (100 IU/kg) was administered during the procedure. All patients were evaluated at 1, 6, and 12 months by phone contact or office visit.
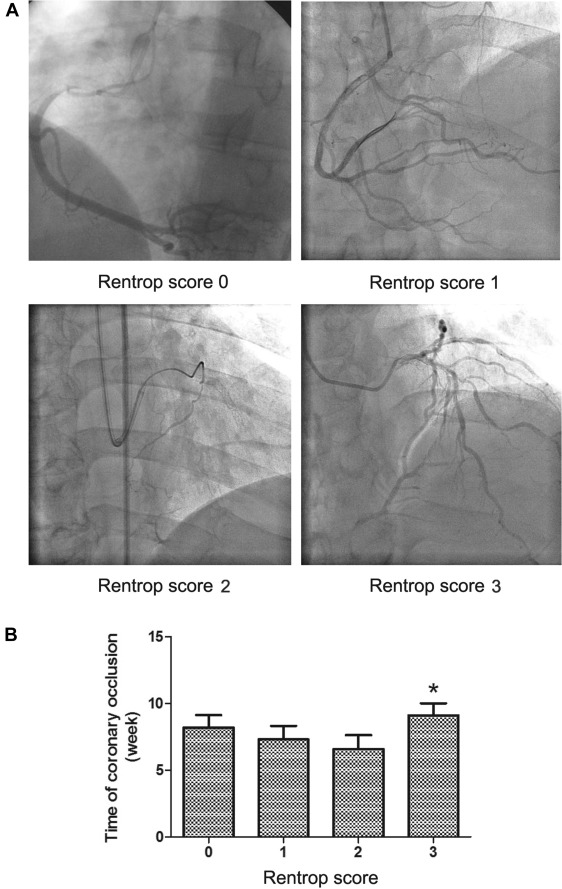
Coronary angiography was performed through the femoral or radial approach by the use of standard techniques. CTO was defined by the presence of a coronary artery stenosis causing complete interruption of anterograde flow in a major epicardial coronary artery or minimal contrast penetration through the lesion without distal vessel opacification (Thrombolysis In Myocardial Infarction 0 to 1 flow). Because patients with acute coronary syndromes within 90 days of enrollment were excluded, the presence of a total occlusion on coronary angiography was assumed to be chronic (at least 3 months). All angiograms were reviewed by 2 experienced interventional cardiologists, according to the lesion classification scheme of the American College of Cardiology/American Heart Association. They were blinded to study protocol and biochemical measurements, and any difference in interpretation was resolved by a third reviewer. The presence and degree of collaterals supplying the distal aspect of a total coronary occlusion from the contralateral vessel were graded on a 4-point scale from 0 to 3 according to the Rentrop scoring system : 0 = no collateral vessels; 1 = thread-like, poorly opacified collaterals with faint visualization of the distal vessel; 2 = moderately opacified collateral channels; 3 = large, brightly filled collateral channels with immediate visualization of the entire distal vessel >10 mm. Low coronary collateralization was defined as Rentrop score 0 or 1, and high coronary collateralization was defined as Rentrop score 2 or 3. For those with more than 1 total coronary occlusion, the vessel with the highest collateral grade was chosen for analysis.
Blood samples were collected at the day of angiography in patients after overnight fasting. Samples were immediately anticoagulated with 2% ethylenediaminetetraacetic acid disodium, then separated by centrifugation and plasma was removed and frozen at −80°C for future analysis while cells were processed for flow cytometry.
Plasma concentrations of vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), transforming growth factor (TGF)-β, high-sensitivity C-reactive protein (hs-CRP), interleukin (IL)-6, tumor necrosis factor (TNF)-α, N-terminal brain-type natriuretic peptide (NT-proBNP), high-density lipoprotein, and low-density lipoprotein were measured using enzyme linked immunosorbent assay (ELISA) kits purchased from Abcam according to the manufacturer’s recommendations. Each sample was placed in double wells.
After red blood cell lysis, cells were labeled with the following antibodies: phycoerythrin conjugated CD34 (No. 12-0349; eBioscience, San Diego, California), fluorescein isothiocyanate–conjugated CD45 (No. 11-9459; eBioscience, San Diego, California), and allophycocyanin-conjugated CD184 (CXCR4, No. 17-9999; eBioscience, San Diego, California) antibodies. Isotype-matched immunoglobulins were used as controls. All antibodies were used at a final concentration of 5 mg/ml. Cells were stained for 20 minutes at room temperature avoiding lights, then washed with phosphate buffer saline and suspended with binding buffer. CXCR4 expression was determined by a FACScan flow cytometer (Becton Dickinson, Rutherford, New Jersey).
Continuous variables are presented as mean and SD, and categorical data are summarized as frequencies or percentages. For categorical clinical variables, differences between groups were evaluated with the chi-square test followed by Bonferroni’s correction to account for multiple comparisons. For continuous variables, differences among groups were analyzed by 1-way analysis of variance or the Kruskal–Wallis analysis followed by post hoc analysis. Correlation between variables was determined by the Spearman’s rho tests as appropriate. For all analyses, a 2-sided p <0.05 was considered statistically significant. All data were processed using SPSS 13.0 (Statistical Package for the Social Sciences, SPSS-PC, Inc., Chicago, Illinois).
Results
Over the study period, a total of 414 patients undergoing coronary angiography agreed to enroll in the research registry. Of these 414 patients, 324 were diagnosed with CTO and formed our patient population. The baseline demographic and clinical characteristics and biochemical measurements for these 414 subjects are listed in Table 1 . The study included patients with CTO (231 men and 93 women, aged 63 ± 11 years) and 90 controls (51 men and 39 women, aged 61 ± 11 years); there was no difference in age between the 2 groups. Among the patients with CTO, low (Rentrop score of 0 or 1) and high (Rentrop score of 2 or 3) coronary collateralization was detected in 183 and 141 patients, respectively ( Figure 1 ). Despite similar number of coronary arteries narrowed and occlusion time, and plasma levels of total cholesterol, high-density lipoprotein, low-density lipoprotein, patients with low collateralization were older, women, had a family history of CTO in a higher proportion and were more hypertensive, had diabetes, and had higher plasma level of triglycerides than those with high collateralization ( Figure 1 , Table 1 ).
| Variable | Control (n=90) | Chronic total coronary occlusion | P | |
|---|---|---|---|---|
| Low coronary collateralization (n=183) | High coronary collateralization (n=141) | |||
| Age (years) | 61±11 | 68±10 | 56±10 ∗ | 0.024 |
| Men | 51 (57%) | 111 (61%) | 120 (85%) ∗ | <0.001 |
| Hypertention | 23 (26%) | 155 (85%) | 107 (76%) ∗ | <0.001 |
| Diabetes mellitus | 11 (12%) | 112 (61%) | 21 (15%) ∗ | <0.001 |
| Family history of chronic total occlusion | 10 (11%) | 87 (48%) | 44 (31%) ∗ | <0.001 |
| Smoke | 27 (30%) | 147 (80%) | 114 (81%) | <0.001 |
| Totalcholesterol (mmol/l) | 4.1±1.1 | 4.9±1.3 | 4.7±0.8 | 0.193 |
| Triglycerides (mmol/l) | 1.2±0.5 | 1.8±1.1 | 1.5±0.8 ∗ | 0.030 |
| High density lipoprotein (mmol/l) | 1.7±0.5 | 1.4±0.2 | 1.6±0.3 | 0.131 |
| Low density lipoprotein (mmol/l) | 2.0±0.9 | 2.1±0.4 | 2.3±0.6 | 0.540 |
| Time of occlusion (week) | – | 7.9±3.1 | 7.8±3.1 | 0.938 |
| Number of coronary arteries narrowed (1/2/3) | – | 14/25/22 | 11/20/16 | 0.937 |
∗ Compare with the low coronary collateralization group p <0.05.
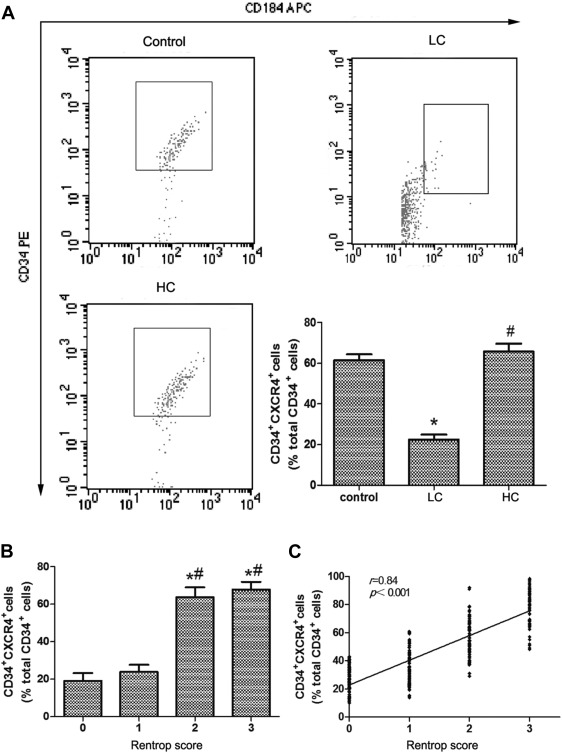
CXCR4 expression in peripheral blood CD34+ cells was greater in patients with CTO with high collateralization than those who had low collateralization (22.5 ± 2.4% vs 65.7 ± 3.9%, p <0.001). However, there was no difference between the patients with high collateralization and controls (65.7 ± 3.9% vs 63.1 ± 3.0%, p >0.05; Figure 2 ). Further statistics showed that subgroups stratified by Rentrop score exhibited significant differences in CXCR4 expression of patients with CTO ( Figure 2 ), and CXCR4 expression was significantly and positively correlated with the degree of collateralization categorized by the Rentrop score ( Figure 2 ). Moreover, multivariate analysis show that after adjusted for other clinical variables, CXCR4 expression still associated with collateral burden, suggesting CXCR4 may be a biomarker of collateralization ( Table 2 ). At 1-year follow-up, patients with CXCR4 expression >40% had statistically significant greater left ventricular systolic function, decreased incidence of sudden cardiac death, restenosis after percutaneous coronary intervention, and heart failure than those with CXCR4 expression <20% (p <0.001). However, there was no significant difference in the incidence of unstable angina pectoris or MI between the 2 groups (p >0.05; Table 3 ).
| Exposure | Model I | Model II | Model III | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| C-X-C motif chemokine receptor 4 | 5.1 | 3.9-6.3 | <0.001 | 5.1 | 3.9-6.4 | <0.001 | 5.6 | 4.1-7.1 | <0.001 |
| Tertile | |||||||||
| Tertile 1 | Reference | Reference | Reference | ||||||
| Tertile 2 | 1.1 | 0.6-1.7 | <0.001 | 1.1 | 0.5-1.7 | <0.001 | 1.1 | 0.5-1.8 | 0.002 |
| Tertile 3 | 1.6 | 1.1-2.0 | <0.001 | 1.6 | 1.2-2.0 | <0.001 | 1.6 | 1.1-2.1 | <0.001 |
| Variable | C-X-C motif chemokine receptor 4 expression of CD34 + cells | p | ||
|---|---|---|---|---|
| <20% (n=84) | 20-40% (n=114) | >40% (n=126) | ||
| Left ventricular ejection fraction (%) | 44±6 | 44±6 | 48±5 | <0.001 |
| Sudden cardiac death (in hospital) | 15 (18%) | 0 (0%) | 0 (0%) | <0.001 |
| Percutaneous coronary intervention (indicates restenosis) | 15 (18%) | 0 (0%) | 0 (0%) | <0.001 |
| Unstable angina pectoris | 12 (14%) | 15 (13%) | 12 (10%) | 0.525 |
| Myocardial infarction | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Heart failure (out hospital) | 39 (46%) | 21 (18%) | 0 (0%) | <0.001 |
CXCR4 expression in peripheral blood CD34+ cells was greater in patients with CTO aged <65 years, men, and patients without diabetes or nonsmokers than those who were aged ≥65 years, women, with diabetes and smoking ( Table 4 ). Analysis of biochemical characteristics showed that the plasma levels of VEGF, bFGF, and TGF-β were significantly higher in patients with 20% to 40% CXCR4 expression, whereas plasma hs-CRP and NT-proBNP levels were downregulated as the CXCR4 expression increased in the patients with CTO ( Table 5 ). Furthermore, to determine risk factors influencing CXCR4 expression, the Spearman’s rho test was performed ( Table 6 ). The correlation between baseline characteristics and CXCR4 expression in patients with CTO showed no significant association between smoking, VEGF, and bFGF, TGF-β, and CXCR4 expression. However, the factors including age, gender, diabetes, hs-CRP, and NT-proBNP were negatively correlated with the peripheral blood CD34+ cells CXCR4 expression. These data indicate that age, gender, diabetes, increased plasma level of hs-CRP, and NT-proBNP can influence the peripheral blood CD34+ cells CXCR4 expression in patients with CTO.



