This study reports the prevalence and prognostic impact of right bundle branch block (RBBB) and left bundle branch block (LBBB) in the admission electrocardiogram (ECG) of comatose survivors of out-of-hospital cardiac arrest (OHCA). The present study is part of the predefined electrocardiographic substudy of the prospective randomized target temperature management trial, which found no benefit of targeting 33°C over 36°C in terms of outcome. Six-hundred eighty-two patients were included in the substudy. An admission ECG, which defined the present study population, was available in 602 patients (88%). These ECGs were stratified by the presence of LBBB, RBBB, or no-BBB (reference) on admission. End points were mortality and neurologic outcome 6 months after OHCA. RBBB was present in 79 patients (13%) and LBBB in 65 patients (11%), and the majority of BBBs (92%) had resolved 4 hours after admission. RBBB was associated with significantly higher 6 months mortality (RBBB: hazard ratio [HR] unadjusted 1.78, 95% confidence interval [CI] 1.30 to 2.43; LBBB: HR unadjusted 1.26, 95% CI 0.87 to 1.81), but this did not reach a level of significance in the adjusted model (HR adjusted 1.33, 95% CI 0.94 to 1.87). Similar findings were seen for neurologic outcome in the unadjusted and adjusted analyses. RBBB was further independently associated with higher odds of unfavorable neurologic outcome (RBBB: adjusted odds ratio 1.97, 95% CI 1.05 to 3.71). In conclusion, BBBs after OHCA were transient in most patients, and RBBB was directly associated with higher mortality and independently associated with higher odds of unfavorable neurologic outcome. RBBB is seemingly an early indicator of an unfavorable prognosis after OHCA.
Outcome prediction in patients with out-of-hospital cardiac arrest (OHCA) is notoriously difficult, and early indicators of prognosis are needed. The first test result available in patients with OHCA is often the electrocardiogram (ECG), which may show a right bundle branch block (RBBB) or left bundle branch block (LBBB). Uncertainty remains regarding the predictive implication of BBB in patients with OHCA, but BBB has been associated with increased mortality in asymptomatic subjects and in those admitted with acute myocardial infarction (AMI), which is a frequent cause of OHCA. A small observational study has suggested that patients with RBBB on the admission ECG after OHCA had a higher mortality than patients without RBBB. Furthermore, in this study, a large proportion of the initial RBBBs resolved during targeted temperature management (TTM). The transient nature of RBBBs could be because of electrophysiological impacts of the cardiac arrest itself or effects of TTM as TTM in the range of 32°C to 34°C is known to trigger structural changes in the ECG. The development over time, relation to cardiac arrest characteristics, and ability to predict outcome of BBBs in patients with OHCA require clarification. Potentially, the presence of BBB could provide important prognostic information before other tests are available and guide the triage in the early post-OHCA phase. This study aimed to report the prevalence and prognostic impact of BBBs on arrival to hospital in comatose survivors of OHCA.
Methods
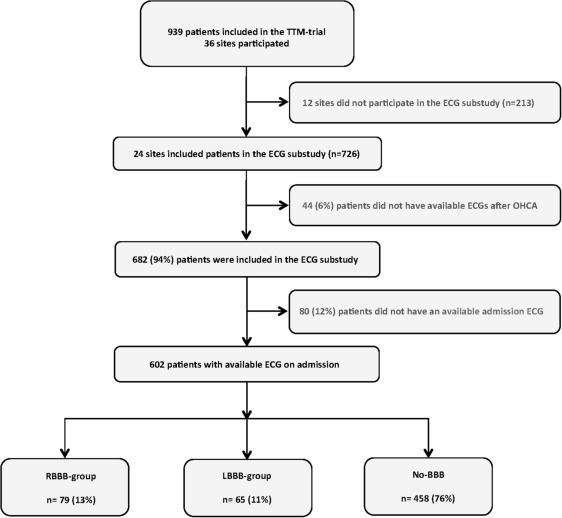
The present study is part of the predefined electrocardiographic substudy of the TTM trial. Adult comatose patients with OHCA (n = 939) with return of spontaneous circulation (ROSC) for a minimum of 20 minutes irrespective of initial rhythm were enrolled and randomized from November 2010 to January 2013 in a 1:1 fashion to TTM at either 33°C or 36°C. A full list of inclusion and exclusion criteria has previously been published. Twenty-four of 36 TTM sites participated in the electrocardiographic substudy, which constituted a total of 682 patients with available ECGs in the full electrocardiographic substudy population. A 12-lead ECG on admission, defining the population of the present substudy, was available in 602 patients (88%; Figure 1 ). Patients with and without admission ECGs had similar baseline characteristics (data not shown), with the exceptions that patients without an admission ECG had shorter time to ROSC (median: 23 [16 to 30] vs 25 [16 to 40], p = 0.05) and lower lactate levels on admission (mean: 5.8 vs 7.1 mmol/L, p = 0.03).
An induction phase of maximum 4 hours to reach the allocated target temperature was protocolled in both arms. After 28 hours, gradual rewarming to 37°C with an increase in core temperature with a maximum of 0.5°C per hour was commenced. Sedation, intubation, and mechanical ventilation were mandatory until the end of the 36-hour intervention period. The main TTM trial showed no benefit of targeting 33°C over 36°C in terms of improving survival or neurologic outcome in comatose survivors of OHCA. The TTM trial complies with the Declaration of Helsinki and is registered and accessible through ClinicalTrials.gov (identifier: NCT01020916 ).
Serial ECGs after OHCA were obtained as part of protocolled management of the patients at the following time points: at hospital admission (ECG1), at allocated target temperature of TTM (ECG2), 28 hours after induction (ECG3), at rewarming 36 hours after induction (ECG4), and 72 hours after induction (ECG5). All ECGs were manually analyzed by assessors blinded to treatment allocation, survival status, and neurologic outcome. The blinding was maintained until data collection and analysis had ended. Demographic and pre-hospital data regarding the circumstances of the OHCA were collected according to the Utstein guidelines. Left ventricular ejection fraction was evaluated within 4 days of the OHCA.
The admission ECGs were stratified according to the presence of LBBB, RBBB, or no-BBB (reference). An ECG was categorized with RBBB based by the following findings: (1) QRS duration >0.12 seconds, (2) a secondary R wave (R′) in V1 or V2, and (3) wide slurred S wave in leads I, V5, and V6. LBBB was defined as (1) QRS duration >0.12 seconds, (2) broad monophasic R wave in leads I, V5, and V6, and (3) absence of Q waves in leads V5 and V6.
Baseline characteristics were presented and stratified by the presence and type of BBB on admission, including groups of LBBB, RBBB, and no-BBB. Normally distributed continuous variables were presented as means ± SD and non-normally distributed variables with median and interquartile range. Differences between groups were analyzed with the chi-square test for categorical variables and continuous variables using the analysis of variance test. Kaplan-Meier survival curves and log-rank tests were used to illustrate and assess differences in 6-month survival between the groups. Univariable and multivariable proportional hazard Cox regressions were used to assess the unadjusted and adjusted associations among LBBB, RBBB, and no-BBB and 6 months mortality. Univariable and multivariable logistic regressions were used in similar fashion to assess the association among LBBB, RBBB, and no-BBB and neurologic outcome 6 months after the OHCA. Neurologic outcome was dichotomized into favorable versus unfavorable outcome, based on the Cerebral Performance Category Scale (CPC) score. Favorable neurologic outcome was defined as a CPC score of 1 or 2, including patients with the ability to carry out independent activities of daily life. Unfavorable outcome was defined as a CPC score of 3 to 5, including severe cerebral disability, with patients depending on daily support, comatose, and expired patients. The multivariable models were adjusted for cardiac arrest characteristics and factors known to influence mortality after OHCA (age, gender, time to ROSC, witnessed arrest, bystander cardiopulmonary resuscitation, bystander defibrillation, primary rhythm, lactate level at admission, ST-elevation myocardial infarction, and known co-morbidity [cumulated number of co-morbidities]). Results were presented as hazard ratios for 6 months mortality and odds ratios for unfavorable neurologic outcome with corresponding 95% confidence intervals. All tests were 2 sided, and statistical significance was defined as a p value <0.05. All statistical analyses were performed using the SAS Statistical Software, version 9.4 (SAS Institute, Cary, North Carolina).
Results
Seventy-nine patients (13%) presented with an RBBB and 65 (11%) with LBBB after OHCA. The majority of the BBBs resolved during TTM. Only 6 patients (8%) had persistent RBBB and only 5 (7%) had persistent LBBB after reaching the target temperature 4 hours after admission. No significant differences in prevalence of LBBB and RBBB were found between patients treated with TTM at 33°C versus 36°C on admission ( Table 1 ) and after reaching the target temperature (p = 0.51).
| Variable | Right bundle branch block n=79 (13%) | Left bundle branch block n=65 (11%) | No bundle branch block n=458 (76%) | p-value |
|---|---|---|---|---|
| Demography: | ||||
| Age – (year) (±SD) | 67 (±11) | 66 (±12) | 63 (±12) | <0.01 |
| Men | 66 (84%) | 54 (83%) | 377 (82%) | 0.96 |
| Randomization allocation | ||||
| TTM at 36° C | 41 (52%) | 40 (62%) | 215 (47%) | 0.08 |
| Cardiac arrest characteristics: | ||||
| Witnessed arrest | 75 (95%) | 61 (94%) | 420 (92%) | 0.54 |
| Bystander Cardiopulmonary Resuscitation | 53 (67%) | 45 (69%) | 332 (72%) | 0.57 |
| Bystander defibrillation | 8 (10%) | 6 (9%) | 45 (10%) | 0.98 |
| Shockable initial rhythm | 61 (80%) | 52 (81%) | 362 (81%) | 0.99 |
| Time to return of spontaneous circulation – min. (IQR) | 33 (22-52) | 29 (17-41) | 25 (16-37) | <0.001 |
| Lactate at admission – (mmol/L) (±SD) | 8.2 (±4.8) | 7.2 (±4.5) | 6.9 (±4.5) | 0.06 |
| Acute coronary angiography | 45 (57%) | 34 (52%) | 294 (64%) | 0.11 |
| Percutaneous coronary intervention | 33 (42%) | 14 (22%) | 203 (44%) | <0.01 |
| Coronary artery bypass graft | 0 (0%) | 1 (2%) | 11 (2%) | 0.46 |
| Left ventricular ejection fraction: | ||||
| Normal or preserved (>50%) | 18 (23%) | 9 (14%) | 96 (21%) | |
| Moderately impaired (30-50%) | 32 (41%) | 24 (37%) | 170 (37%) | 0.15 |
| Severely impaired (<30%) | 14 (18%) | 20 (31%) | 78 (17%) | |
| Not performed | 15 (19%) | 12 (18%) | 114 (25%) | |
| Pre-arrest comorbidities: | ||||
| Coronary disease | 27 (35%) | 23 (35%) | 121 (26%) | 0.15 |
| Previous acute myocardial infarction | 16 (20%) | 21 (32%) | 92 (20%) | 0.08 |
| Previous coronary artery bypass graft | 9 (11%) | 8 (13%) | 37 (8%) | 0.37 |
| Previous cardiac arrest | 1 (1%) | 3 (5%) | 8 (2 %) | 0.27 |
| Congestive heart failure | 7 (9%) | 7 (11%) | 23 (5%) | 0.11 |
| Hypertension | 33 (42%) | 26 (40%) | 162 (35%) | 0.47 |
| Previous transitory cerebral ischemia /stroke | 7 (9%) | 7 (11%) | 33 (7%) | 0.57 |
| Diabetes | 13 (17%) | 12 (18%) | 72 (16%) | 0.86 |
| Asthma/ chronic obstructive pulmonary disease | 9 (11%) | 9 (14%) | 44 (10%) | 0.54 |
| Alcoholism | 4 (5%) | 2 (3%) | 18 (4%) | 0.83 |
| Comorbidity – median (IQR) | 2 (0-3) | 2 (1-4) | 1 (0-3) | <0.03 |
Patients with BBBs were significantly older than the no-BBB group. Time from cardiac arrest to ROSC was significantly longer in the RBBB and LBBB group, and a trend toward higher lactate levels on admission was found in RBBB patients. Acute coronary angiographies (CAGs) were performed with similar frequencies between the groups, but primary percutaneous coronary intervention (PCI) was performed less often in patients with LBBB ( Table 1 ).
Factors independently associated with RBBB after OHCA were increasing age and longer time to ROSC. A higher cumulated number of co-morbidities were associated with LBBB after OHCA in univariable analysis, but no factor in our multivariable model was, however, independently associated with LBBB ( Table 2 ).
| Odds ratios for right bundle branch block at admission after out-of-hospital cardiac arrest | Odds ratios for left bundle branch block at admission after out-of- hospital cardiac arrest | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | |||||
| Odds ratio (95%CI) | p-value | Odds ratio (95%CI) | p-value | Odds ratio (95%CI) | p-value | Odds ratio (95%CI) | p-value | |
| Age at arrest, per 5 year | 1.14 (1.03-1.26) | <0.02 | 1.13 (1.01-1.27) | 0.04 | 1.11 (0.99-1.23) | 0.07 | 1.08 (0.96-1.23) | 0.21 |
| Sex, male | 1.08 (0.57-2.05) | 0.80 | 1.11 (0.55-2.23) | 0.77 | 1.04 (0.53-2.07) | 0.91 | 1.01 (0.49-2.11) | 0.97 |
| Time to return of spontaneous circulation /5 minute | 1.09 (1.04-1.13) | <0.001 | 1.09 (1.04-1.14) | <0.001 | 1.02 (0.97-1.07) | 0.42 | 1.02 (0.96-1.08) | 0.49 |
| Lactate level at admission per mmol/L | 1.06 (1.01-1.12) | 0.02 | 1.04 (0.98-1.09) | 0.19 | 1.00 (0.95-1.07) | 0.88 | 1.00 (0.94-1.07) | 0.97 |
| Witnessed arrest | 1.64 (0.57-4.69) | 0.36 | 1.69 (0.56-5.16) | 0.35 | 1.29 (0.45-3.73) | 0.63 | 1.53 (0.45-5.21) | 0.49 |
| Bystander cardiopulmonary rescue | 0.79 (0.48-1.31) | 0.36 | 0.76 (0.42-1.35) | 0.34 | 0.89 (0.51-1.55) | 0.68 | 0.93 (0.49-1.73) | 0.81 |
| Bystander defibrillation | 1.04 (0.48-2.29) | 0.92 | 1.39 (0.59-3.29) | 0.44 | 0.93 (0.38-2.25) | 0.87 | 0.86 (0.32-2.36) | 0.77 |
| Shockable primary rhythm | 0.95 (0.52-1.75) | 0.88 | 1.31 (0.68-2.54) | 0.42 | 1.02 (0.53-1.99) | 0.94 | 1.11 (0.55-2.27) | 0.77 |
| Comorbidity | 1.08 (0.96-1.20) | 0.19 | 1.03 (0.90-1.17) | 0.69 | 1.13 (1.01-1.27) | <0.04 | 1.11 (0.97-1.27) | 0.13 |
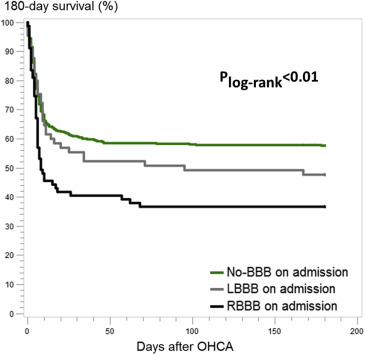
When assessing 6 months mortality between the groups, patients without BBB had the highest survival rates and RBBB the lowest ( Figure 2 ). RBBB was associated with higher mortality in the univariable analyses compared with the no-BBB group. However, when adjusting for cardiac arrest characteristics and factors known to influence mortality, this result did not reach level of statistical significance ( Table 3 ). RBBB were, however, associated with higher odds of unfavorable neurologic outcome compared with no-BBB, which remained an independent association after adjusting for potential confounders ( Table 3 ). LBBB was not significantly associated with mortality or neurologic outcome in either the univariable or the multivariable models.
| Hazard ratio for 180-day mortality | Odds ratios for unfavorable neurological outcome 180 days after out-of-hospital cardiac arrest | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | |||||
| Hazard ratio (95% confidence interval) | p-value | Hazard ratio (95% confidence interval) | p-value | Odds ratio (95% confidence interval) | p-value | Odds ratio (95% confidence interval) | p-value | |
| Right bundle branch block | 1.78 (1.30-2.43) | 0.001 | 1.33 (0.94-1.87) | 0.11 | 2.61 (1.56-4.36) | <0.001 | 1.97 (1.05-3.71) | <0.05 |
| Left bundle branch block | 1.26 (0.87-1.81) | 0.22 | 1.13 (0.77-1.65) | 0.54 | 1.51 (0.89-2.55) | 0.13 | 1.33 (0.69-2.58) | 0.39 |
| No bundle branch block (reference) | 1 | 1 | 1 | 1 | ||||
| Age at arrest/5 year | 1.26 (1.19-1.32) | <0.0001 | 1.25 (1.17-1.33) | <0.0001 | 1.37 (1.27-1.48) | <0.0001 | 1.38 (1.24-1.52) | <0.0001 |
| Sex, male | 0.88 (0.65-1.19) | 0.40 | 1.15 (0.83-1.61) | 0.40 | 0.85 (0.55-1.30) | 0.44 | 1.15 (0.65-2.03) | 0.63 |
| Time to return of spontaneous circulation /5 minute | 1.09 (1.07-1.10) | <0.0001 | 1.07 (1.05-1.09) | <0.0001 | 1.17 (1.11-1.22) | <0.0001 | 1.15 (1.09-1.22) | <0.0001 |
| Witnessed arrest | 0.61 (0.41-0.90) | 0.012 | 0.56 (0.36-0.88) | <0.02 | 0.58 (0.31-1.08) | 0.09 | 0.57 (0.25-1.27) | 0.17 |
| Bystander cardiopulmonary resuscitation | 0.57 (0.45-0.73) | <0.0001 | 0.91 (0.69-1.20) | 0.49 | 0.49 (0.34-0.70) | 0.0001 | 0.76 (0.47-1.24) | 0.27 |
| Bystander defibrillation | 0.51 (0.31-0.84) | 0.008 | 0.74 (0.43-1.27) | 0.27 | 0.54 (0.31-0.94) | 0.03 | 0.59 (0.29-1.19) | 0.14 |
| Shockable primary rhythm | 0.26 (0.20-0.33) | <0.0001 | 0.31 (0.23-0.41) | <0.0001 | 0.12 (0.07-0.21) | <0.0001 | 0.16 (0.09-0.31) | <0.0001 |
| Lactate level at admission per mmol/L | 1.09 (1.07-1.12) | <0.0001 | 1.07 (1.04-1.09) | <0.0001 | 1.11 (1.07-1.15) | <0.0001 | 1.06 (1.01-1.11) | 0.01 |
| ST-elevation myocardial infarction | 0.76 (0.59-0.97) | 0.027 | 0.99 (0.76-1.30) | 0.95 | 0.67 (0.48-0.93) | <0.02 | 0.96 (0.62-1.48) | 0.85 |
| Comorbidity | 1.14 (1.09-1.20) | <0.0001 | 1.03 (0.97-1.10) | 0.30 | 1.27 (1.16-1.38) | <0.0001 | 1.06 (0.95-1.18) | 0.32 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


