Radionuclide Studies of the Mediastinum
William G. Spies
Until recently, the role of radionuclide imaging in the chest was primarily related to evaluation of disorders of the heart and lungs, particularly the evaluation of myocardial perfusion and ventricular function, the use of ventilation/perfusion scintigraphy in the detection of pulmonary embolism, and the diagnosis of inflammatory and neoplastic disorders of the lungs and bony thorax using traditional single-photon radionuclides. In the course of pulmonary scintigraphy, findings may indirectly identify the presence of pathology in the mediastinum, such as obstructive airways disease on ventilation studies or the presence of mediastinal lesions producing secondary effects on pulmonary ventilation, perfusion, or both, including mass lesions and fibrosing mediastinitis.
Gallium imaging of the chest has been used in the detection of inflammatory lesions in the lungs and mediastinum and in the detection and staging of certain intrathoracic neoplasms, notably bronchial carcinoma and lymphoma. Focal mediastinal adenopathy is also an important finding in patients with acquired immunodeficiency syndrome (AIDS) presenting with fever, respiratory symptoms, or both. Indium-111(111In)–labeled leukocytes are useful also in the detection of inflammatory processes, including mediastinitis.
With the advent of regulatory agency approval and established literature supporting it, the past several years have seen a dramatic growth in the clinical use of positron emission tomographic (PET) imaging using the radiopharmaceutical fluorine-18 (18Fl) 2-fluoro-2-deoxy-D-glucose (FDG) for the detection and staging of a number of common malignancies. Tumors for which this modality has proven to be efficacious comprise some of the most important malignancies of the chest and mediastinum, including non-small-cell lung carcinoma (NSCLC), lymphoma, esophageal carcinoma, carcinoma of the head and neck, and, more recently, breast carcinoma and well-differentiated thyroid carcinoma. PET imaging has been shown to be superior to gallium scintigraphy in the diagnosis, staging, and restaging of NSCLC and lymphoma and has largely replaced it for these purposes in many centers. Furthermore, PET imaging has also been shown to be superior even to computed tomography (CT) scanning for the staging, assessment of the response to therapy, and detection of recurrences in patients with these tumors. This imaging modality, which was once limited to a few highly specialized research centers, is becoming widely clinically available at much lower expense. In addition, some manufacturers have developed “hybrid” imaging units capable of performing both PET and CT studies sequentially during a single imaging session.
Radionuclide lymphoscintigraphy was used for a number of years to evaluate for the presence of tumor involvement in the otherwise inaccessible internal mammary lymph nodes, which are a frequent site of metastatic disease in breast carcinoma. More recently, lymphoscintigraphy has been used preoperatively and intraoperatively using specialized probe detectors to localize the sentinel lymph node(s) in patients with breast carcinoma or medium-thickness malignant melanomas. At present, preoperative lymphoscintigraphy with sentinel lymph node mapping—coupled with intraoperative probe localization, biopsy, and immunohistochemical analysis—has rapidly become the standard of care for patients with operable breast carcinoma.
Peptide radionuclide imaging agents have been developed and evaluated for the detection of specific tumors. The most widely studied agent of this type, a somatostatin analog of octreotide, is currently routinely used clinically for the detection and follow-up of carcinoid tumor, islet cell carcinoma of the pancreas, medullary carcinoma of the thyroid, and other related neuroendocrine tumors. Some of these agents can also be modified or used directly for radionuclide therapy of these tumors.
The compound metaiodobenzylguanidine (MIBG) labeled with iodine-131(131I) or iodine-123 (123I) is a norepinephrine analog that has specific affinity for adrenal medullary tumors such as pheochromocytomas, paraganglionomas, and neuro- blastomas. This agent can be used in conjunction with laboratory data and CT scanning or magnetic resonance imaging (MRI) to detect and localize these tumors, especially extra-adrenal pheochromocytomas, which may be located in the mediastinum, retroperitoneum, or pelvis.
A number of murine, chimeric, and even human monoclonal antibodies directed against human neoplasms—including bronchial carcinoma, lymphoma, colorectal carcinoma, ovarian carcinoma, and prostate carcinoma—have been evaluated in the detection and staging of these lesions. Some of these agents have also been radiolabeled with high-energy beta-emitting radionuclides and evaluated for use as immunoradiotherapeutic agents as well. At present, only one monoclonal antibody has been
approved by the U.S. Food and Drug Administration (FDA) for routine clinical use in the treatment of refractory non-Hodgkin’s lymphoma, and another related agent is currently undergoing the approval process.
approved by the U.S. Food and Drug Administration (FDA) for routine clinical use in the treatment of refractory non-Hodgkin’s lymphoma, and another related agent is currently undergoing the approval process.
Thyroid scintigraphy is a sensitive and specific technique for establishing the presence of functioning thyroid tissue within mediastinal masses. This approach is valuable in the differential diagnosis of superior mediastinal masses suspected to represent substernal goiters and in the detection of functioning metastases in patients with well-differentiated thyroid carcinoma. In addition, the iodine radioisotope (131I) is used therapeutically to ablate residual normal thyroid tissue and metastatic disease in thyroid carcinoma once the presence of functioning thyroid tissue is established by 131I whole-body imaging. FDG PET imaging may be useful in the detection of occult mediastinal metastases in patients with elevated serum thyroglobulin levels but negative 131I whole-body scans, and it has recently received government approval for this indication. Parathyroid scintigraphy using technetium-99m (99mTc) sestamibi is a sensitive method for the detection of parathyroid adenomas in the neck and superior mediastinum.
Functional imaging of the esophagus using orally administered radiopharmaceuticals can be used to detect and quantify the presence of gastroesophageal reflux and to quantitatively evaluate esophageal motility, as discussed in detail in Chapter 125.
Radionuclide angiography of the chest is most often used in first-pass cardiac studies and to evaluate right and left ventricular function; it can also help establish the presence of vascular lesions of the great vessels or mediastinum or the presence of superior vena caval obstruction or other vascular abnormalities.
Apart from the direct evaluation of mediastinal lesions, nuclear medicine procedures are also useful in the diagnosis of metastatic lesions from primary mediastinal tumors. In this regard, PET imaging and bone, gallium, and octreotide scintigraphy are currently the most important modalities, with monoclonal antibodies also being used in special circumstances.
Ventilation/Perfusion Scintigraphy
Radionuclide imaging of the lungs remains one of the most commonly performed nuclear medicine procedures of the chest. Although spiral CT imaging of the chest has emerged as a viable alternative modality for the evaluation of patients with suspected pulmonary thromboembolism, ventilation/perfusion (V/Q) lung scintigraphy remains an important screening modality in the evaluation of these patients, and this application is by far the most important indication for this procedure. This subject is discussed in greater detail in Chapter 13. However, V/Q imaging can also provide useful information regarding certain types of mediastinal pathology. Ventilation imaging is performed using either radioactive gases, such as xenon-133 (133Xe) or krypton 81m (81mKr) or using fine, uniform aerosols labeled with 99mTc, which are inhaled by the patient. Alderson and colleagues4,5,6 have shown that these studies are extremely sensitive for the detection of obstructive airways disease, nearly twice as sensitive as routine chest radiographs. The 133Xe study is performed by having the patient slowly inhale as a 10- to 20-mCi (370- to 740-mBq) dose of the radioactive gas is injected into a breathing apparatus, similar to a standard spirometer. The patient holds his or her breath as long as possible while a posterior “single-breath” image is acquired, which reflects regional ventilation. The patient then breathes a 133Xe/air mixture in a closed system for 3 to 5 minutes to allow equilibration of the gas in the airways to occur. During or at the conclusion of this period, an “equilibrium washin” image or images are obtained, which reflect total ventilated lung volume. Finally, the patient exhales the radioactive gas and breathes room air while additional images are obtained every 30 to 60 seconds, constituting the “washout” phase. This latter phase is the most sensitive for detection of obstructive airways disease and cannot be obtained with either 81mKr or 99mTc aerosols. In 133Xe imaging (unlike the other ventilation imaging agents), all images are acquired in the posterior projection with the exception that posterior oblique views are often obtained during the washout phase, if possible, to improve the localization of abnormalities in the anteroposterior plane.
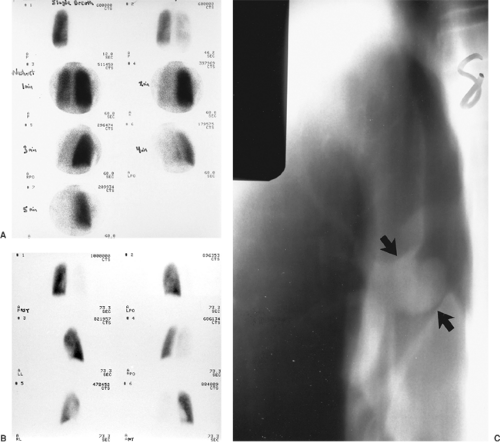
In addition to diffuse involvement in emphysema, asthma, or chronic bronchitis, the presence of endobronchial masses, foreign bodies, or mucous plugging can be detected by these studies, particularly using 133Xe imaging. The most significant finding in such cases is the presence of decreased uptake of the gas on the single-breath study, with prolonged retention of the tracer in the affected lung during the washout phase, when the patient is breathing room air. Whole-lung hypoventilation is particularly suggestive of a central mass, foreign body, or mucous plug causing a ball–valve type of airway obstruction and often results in a secondary global decrease in perfusion to the affected lung via reflex vasoconstriction, as demonstrated in Figure 167-1. With aerosol ventilation agents, areas of obstructive airways disease present as focal defects in ventilation. In severe cases of chronic obstructive airways disease, clumping of the radioaerosol in the central airways may also be observed.
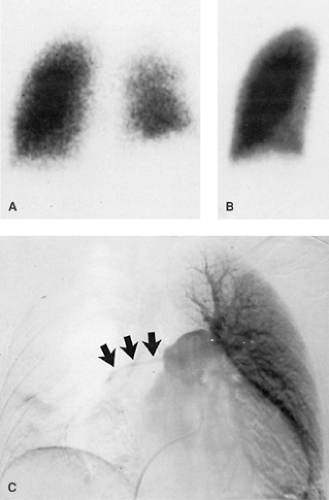
Pulmonary perfusion imaging is performed by intravenous injection of 99mTc-labeled particles, such as macroaggregated albumin (MAA), which are trapped in the pulmonary capillary system in proportion to regional pulmonary blood flow. Although pulmonary embolism is again the most important cause of perfusion defects, perfusion abnormalities are also commonly associated with the presence of mediastinal lesions, which produce hypoperfusion as the result of compression or invasion of pulmonary arterial or venous branches. In combination with the ventilation study, it can be determined whether the perfusion defect is the primary abnormality (producing V/Q mismatch) or whether there is secondary reflex vasoconstriction and shunting of blood flow away from a site of ventilatory deficit (matching abnormalities). Important mediastinal lesions producing such changes in pulmonary blood flow include mediastinal masses due to lung carcinoma or other tumors and fibrosing mediastinitis. The finding of lobar or whole-lung V/Q mismatch is suggestive of these disorders, although these findings may also occur in other situations, as discussed by Datz,29 including massive unilateral pulmonary embolism and other primary vascular lesions, such as arteritis or prior radiation therapy, as shown in Figure 167-2. Thus a mediastinal mass lesion, depending on its location, may produce either V/Q match or mismatch.
The radiopharmaceutical uptake in ventilation/perfusion imaging is easily quantitated using a digital computer interfaced to the nuclear medicine gamma camera used to acquire the study. White and associates105 demonstrated perfusion defects
associated with bronchial carcinoma and determined that the size of the perfusion defect correlated with the extent of the lesion. They found that if the perfusion to the ipsilateral lung was less than 33% of total pulmonary perfusion, the lesion was nearly always unresectable. Quantitation of both perfusion and ventilation allows calculation of regional V/Q ratios. Comparison of these ratios with normal values can also help to predict resectability of tumors, although this analysis is not commonly performed because of relatively low sensitivity and the availability of more accurate staging of lung carcinoma by CT and, more recently, PET imaging. However, quantitative V/Q imaging is now performed to predict pulmonary function following
contemplated pneumonectomy, as described by Kristersson, (1974) Olsen,81 and Boysen19 and their associates. Assessment of postresection pulmonary reserve is an important aspect of the preoperative evaluation of patients considered for lung resection. Significant disability can result from chronic ventilatory insufficiency if the postoperative forced expiratory volume in 1 second (FEV1) is less than 0.8 L, as reported by Olsen and associates81 and by Williams and Brenowitz.106 Quantitative V/Q scintigraphy can accurately predict the postoperative pulmonary function in these patients, as reported by Wernly and coworkers,104 and surgery is usually not performed if the predicted FEV1 is less than 0.8 L, as described by Block and Olsen.16 This technique has also been used to monitor pulmonary function following pulmonary transplantation, as described by the Toronto Lung Transplant Group,99 and to assess patients preoperatively prior to lung reduction surgery, as described by Wang and coworkers.102
associated with bronchial carcinoma and determined that the size of the perfusion defect correlated with the extent of the lesion. They found that if the perfusion to the ipsilateral lung was less than 33% of total pulmonary perfusion, the lesion was nearly always unresectable. Quantitation of both perfusion and ventilation allows calculation of regional V/Q ratios. Comparison of these ratios with normal values can also help to predict resectability of tumors, although this analysis is not commonly performed because of relatively low sensitivity and the availability of more accurate staging of lung carcinoma by CT and, more recently, PET imaging. However, quantitative V/Q imaging is now performed to predict pulmonary function following
contemplated pneumonectomy, as described by Kristersson, (1974) Olsen,81 and Boysen19 and their associates. Assessment of postresection pulmonary reserve is an important aspect of the preoperative evaluation of patients considered for lung resection. Significant disability can result from chronic ventilatory insufficiency if the postoperative forced expiratory volume in 1 second (FEV1) is less than 0.8 L, as reported by Olsen and associates81 and by Williams and Brenowitz.106 Quantitative V/Q scintigraphy can accurately predict the postoperative pulmonary function in these patients, as reported by Wernly and coworkers,104 and surgery is usually not performed if the predicted FEV1 is less than 0.8 L, as described by Block and Olsen.16 This technique has also been used to monitor pulmonary function following pulmonary transplantation, as described by the Toronto Lung Transplant Group,99 and to assess patients preoperatively prior to lung reduction surgery, as described by Wang and coworkers.102
Gallium and Indium Leukocyte Scintigraphy
Gallium-67 (67Ga) citrate is an iron analogue used for evaluation of both inflammatory and neoplastic lesions. 67Ga is a cyclotron-produced radionuclide with a physical half-life of 78 hours and several gamma photopeaks for imaging. Intravenously injected gallium is largely bound to serum transferrin in the blood and taken up by the liver, bone, kidneys, colon, spleen, salivary glands, and lacrimal glands. Approximately 10% to 25% of the injected dose is excreted by the kidneys during the first 24 hours and subsequently by the colon. In children, there is significant uptake by the normal thymus gland, making evaluation of the mediastinum difficult.
Gallium is actively accumulated in a variety of infectious and noninfectious inflammatory lesions and in certain tumors. The mechanisms of gallium uptake have been widely discussed and debated, as reviewed by Hoffer51 and Palestro.83 Gallium scintigraphy for the detection of inflammatory processes usually includes imaging at 24 hours or even earlier in order to diagnose acute infections rapidly. Further delayed images are also commonly obtained to confirm the findings on the early images. Tumor imaging is more often performed at 48 to 72 hours or even later, when target/background ratios in lesions typically become higher. While doses as low as 3 to 5 mCi (111–185 mBq) of 67Ga citrate have been used, it is common to administer higher doses, in the range of 8 to 10 mCi (296–370 mBq).
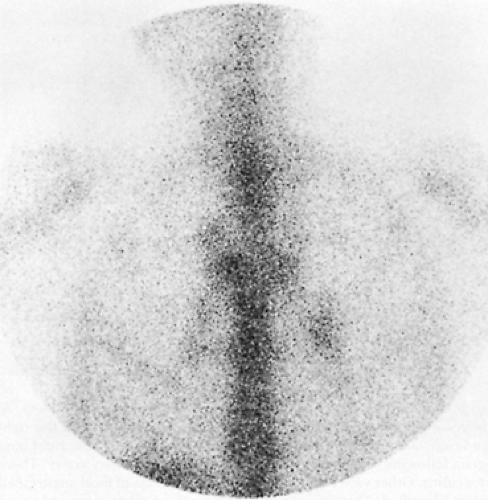
Gallium scintigraphy is a sensitive method for the detection of mediastinal pathology, especially the presence of mediastinitis or lymphadenopathy. This evaluation is particularly useful in patients with AIDS presenting with fever or respiratory symptoms, as reported by Kramer,63 Bitran,15 and Mehta75 and their associates. In these patients, mediastinal or hilar adenopathy is often due to mycobacterial infection, commonly by atypical mycobacteria such as Mycobacterium avium–intracellulare (MAI) (Fig. 167-3). Other nonneoplastic causes of mediastinal adenopathy include viral or bacterial infections and other types of granulomatous disease, such as sarcoidosis.
Neoplasms of the mediastinum with high avidity for gallium include bronchial carcinoma, lymphoma, and metastases from mesothelioma, testicular tumors, and melanoma. Gallium imaging has proven particularly useful in the follow-up of these patients, since the gallium activity will resolve as the lesion is effectively treated, even though CT scans may still demonstrate residual soft tissue densities due to fibrosis at sites of prior adenopathy (Fig. 167-4). Furthermore, serial gallium imaging may provide useful prognostic data in patients undergoing chemotherapy or radiation therapy. Janicek and associates57 found that early restaging gallium scans during high-dose cyclophosphamide, doxorubicin, vincristine, and prednisone
(CHOP) chemotherapy permitted the differentiation between patients with aggressive non-Hodgkin’s lymphoma likely to have prolonged disease-free intervals from those who would likely fail to respond and thus be candidates for alternative treatment. Front and coworkers43 recently found similar results using gallium scintigraphy in patients with Hodgkin’s disease (Hodgkin’s lymphoma) undergoing chemotherapy. There was a statistically significant difference in failure-free survival between patients with positive versus negative gallium scan results after one cycle of chemotherapy (p <0.002), whereas no significant difference was noted between patients with positive versus negative CT scan results at midtreatment. Furthermore, 92% of patients with negative gallium scan results after one cycle and 82% with negative scan results at midtreatment remained in complete response. Front and associates42 also indicated that more than 50% of patients with lymphoma who achieve complete responses to therapy have residual soft tissue masses on palpation, radiographs, or CT. Furthermore, gallium imaging is a sensitive means of detecting recurrences early. In AIDS, if no infectious process is present, mediastinal or hilar adenopathy on gallium images is usually due to lymphoma. Kaposi’s sarcoma is not a gallium-avid tumor and therefore should be suspected in AIDS patients with soft tissue chest masses on the chest radiograph that do not show increased gallium uptake. With respect to bronchial carcinoma, Hoffer52 reviewed data from several other studies, indicating a sensitivity of 80% to 90% for all cell types, although some have reported a somewhat lower sensitivity in adenocarcinoma. Uptake by mediastinal adenopathy may not be of the same magnitude as uptake by a primary parenchymal lesion, which could have adverse implications with regard to staging of NSCLC with gallium imaging. In addition, there is a potential for false-positive findings in patients with inflammatory lesions. At present, PET imaging has proven to be superior to both gallium scintigraphy and CT in the staging and follow-up of NSCLC, lymphoma, and other tumors, as discussed below, and is rapidly replacing gallium scintigraphy in these clinical settings where available.
(CHOP) chemotherapy permitted the differentiation between patients with aggressive non-Hodgkin’s lymphoma likely to have prolonged disease-free intervals from those who would likely fail to respond and thus be candidates for alternative treatment. Front and coworkers43 recently found similar results using gallium scintigraphy in patients with Hodgkin’s disease (Hodgkin’s lymphoma) undergoing chemotherapy. There was a statistically significant difference in failure-free survival between patients with positive versus negative gallium scan results after one cycle of chemotherapy (p <0.002), whereas no significant difference was noted between patients with positive versus negative CT scan results at midtreatment. Furthermore, 92% of patients with negative gallium scan results after one cycle and 82% with negative scan results at midtreatment remained in complete response. Front and associates42 also indicated that more than 50% of patients with lymphoma who achieve complete responses to therapy have residual soft tissue masses on palpation, radiographs, or CT. Furthermore, gallium imaging is a sensitive means of detecting recurrences early. In AIDS, if no infectious process is present, mediastinal or hilar adenopathy on gallium images is usually due to lymphoma. Kaposi’s sarcoma is not a gallium-avid tumor and therefore should be suspected in AIDS patients with soft tissue chest masses on the chest radiograph that do not show increased gallium uptake. With respect to bronchial carcinoma, Hoffer52 reviewed data from several other studies, indicating a sensitivity of 80% to 90% for all cell types, although some have reported a somewhat lower sensitivity in adenocarcinoma. Uptake by mediastinal adenopathy may not be of the same magnitude as uptake by a primary parenchymal lesion, which could have adverse implications with regard to staging of NSCLC with gallium imaging. In addition, there is a potential for false-positive findings in patients with inflammatory lesions. At present, PET imaging has proven to be superior to both gallium scintigraphy and CT in the staging and follow-up of NSCLC, lymphoma, and other tumors, as discussed below, and is rapidly replacing gallium scintigraphy in these clinical settings where available.
The use of single photon emission computed tomography (SPECT) imaging can significantly enhance the detection of
mediastinal and hilar adenopathy in gallium imaging. This modification of the study is performed using a gamma camera fitted with a specialized gantry or counterbalance mechanism that permits the camera to rotate a full 360 degrees around the patient. The acquisition of data at multiple angles during rotation allows the computer to reconstruct tomographic images in a fashion completely analogous to conventional x-ray CT; in addition, transaxial, sagittal, and coronal images can all be obtained with a single rotation, and reorientation of the images in different planes is also readily achieved. Tomographic images “blur” data from planes above and below the plane of interest, resulting in improved image contrast and thus improved detection of focal pathology. Although more commonly used in cardiac, brain, and bone imaging, SPECT can be undertaken in conjunction with any nuclear medicine procedure performed with a rotating gamma camera and is often used as an adjunct to conventional planar gallium imaging. Tumeh and associates100 demonstrated significant gains in both sensitivity and specificity in using SPECT imaging compared with planar gallium imaging in patients with lymphoma. The SPECT studies were able to identify additional sites of involvement in the chest and abdomen and to exclude abnormalities in sites that were equivocally abnormal on the planar images. In a study of gallium scintigraphy in the restaging of patients with aggressive non-Hodgkin’s lymphoma undergoing high-dose CHOP chemotherapy, Janicek and associates57 found that SPECT imaging provided similar information at the time of diagnosis as planar imaging in patients with bulky, gallium-positive tumors, but it also provided confirmatory information in treated lesions that were of lower intensity or located in proximity to normal anatomic structures.
mediastinal and hilar adenopathy in gallium imaging. This modification of the study is performed using a gamma camera fitted with a specialized gantry or counterbalance mechanism that permits the camera to rotate a full 360 degrees around the patient. The acquisition of data at multiple angles during rotation allows the computer to reconstruct tomographic images in a fashion completely analogous to conventional x-ray CT; in addition, transaxial, sagittal, and coronal images can all be obtained with a single rotation, and reorientation of the images in different planes is also readily achieved. Tomographic images “blur” data from planes above and below the plane of interest, resulting in improved image contrast and thus improved detection of focal pathology. Although more commonly used in cardiac, brain, and bone imaging, SPECT can be undertaken in conjunction with any nuclear medicine procedure performed with a rotating gamma camera and is often used as an adjunct to conventional planar gallium imaging. Tumeh and associates100 demonstrated significant gains in both sensitivity and specificity in using SPECT imaging compared with planar gallium imaging in patients with lymphoma. The SPECT studies were able to identify additional sites of involvement in the chest and abdomen and to exclude abnormalities in sites that were equivocally abnormal on the planar images. In a study of gallium scintigraphy in the restaging of patients with aggressive non-Hodgkin’s lymphoma undergoing high-dose CHOP chemotherapy, Janicek and associates57 found that SPECT imaging provided similar information at the time of diagnosis as planar imaging in patients with bulky, gallium-positive tumors, but it also provided confirmatory information in treated lesions that were of lower intensity or located in proximity to normal anatomic structures.
In addition to gallium imaging, autologous leukocytes can be labeled with 111In oxine and reinjected for imaging, as reviewed by Coleman,21 Marcus,72 and Datz.30 This radiopharmaceutical is more specific for infection than gallium, although it is rarely taken up by neoplasms. Normal uptake is seen in the spleen, bone marrow, and liver. 111In white blood cell (WBC) imaging may be preferred over gallium in certain clinical settings, but both are useful in evaluating suspected mediastinal infections. It should be noted that uptake in the lungs is normal early after injection of approximately 500 μ Ci (18.5 MBq) 111In WBCs; imaging is therefore usually performed at 18 to 24 hours. Partly for this reason, Fineman and coworkers38 and most other investigators favor the use of gallium over indium leukocytes when pulmonary parenchymal infections are suspected, as in AIDS patients. In indium leukocyte scintigraphy, unlike gallium, delayed imaging beyond 24 hours is rarely necessary. Gallium is probably also more useful in suspected chronic infections, since the majority of labeled leukocytes in 111In WBC imaging are neutrophils; thus the sensitivity for chronic infection may be less. Other radiopharmaceuticals have also been developed for the detection of sites of infection—including 99mTc hexamethylpropylene amine oxime (HMPAO)–labeled leukocytes, monoclonal antigranulocyte and polyclonal immunoglobulin G nonspecific antibodies, chemotactic peptide agents, liposomes, nanocolloids, and others—as reviewed by Peters84 and by Becker,12 Corstens,23 and Fischman39 and their coworkers. Of these, only the 99mTc-labeled leukocytes have achieved widespread clinical use to date. As further discussed, FDG PET imaging has emerged as a powerful tool in oncologic imaging. Some of the most common false-positive findings on PET imaging are related to infectious and noninfectious inflammatory processes associated with increased glucose metabolism, including sarcoidosis, tuberculosis, abscesses, and other infections. As a result, FDG PET imaging may also play a potential role in the evaluation of suspected inflammatory processes, such as enterocolitis, musculoskeletal infections, cerebral infections and others, as described by Kresnik,65 Temmerman,97 DeWinter,33 Stumpe,95 Sugawara,96 and Meyer77 and their coworkers. This topic has also recently been reviewed by Alavi and associates2 and by Zhuang and Alavi.116 However, this application of PET imaging remains primarily investigational at present.
Positron Emission Tomography
The development of a growing body of literature supporting the use of PET, coupled with recent regulatory and reimbursement approval breakthroughs, has led to its rapid advance as a widely used diagnostic modality for the evaluation of patients with a variety of neoplasms. PET has long been available as a research tool in the evaluation of brain and cardiac metabolism, often using ultra–short-lived positron-emitting radionuclides such as carbon-11, nitrogen-13, and oxygen-15. Although these agents permit the labeling of biologically important molecules that serve as excellent tracers of normal and abnormal metabolic functions, their physical nature (half-lives in the range of 2–20 minutes) demands that they be prepared locally for immediate use. This preparation requires the availability of an on-site medical cyclotron and the equipment needed to radiolabel the necessary compounds with these isotopes, which involves complex and expensive instrumentation. In addition, several dedicated personnel are required to operate and maintain this equipment, further adding to the cost. These considerations have long relegated PET imaging to the realm of the research laboratory and kept it beyond the reach of all but the most specialized medical centers. However, a growing body of research over the past several years has been based on the use of another radiopharmaceutical for PET: fluorodeoxyglucose (FDG). FDG is also a positron-emitting radiopharmaceutical, but it has the distinct advantage of a longer half-life of 1.83 hours (∼110 minutes), permitting it to be transported over short distances within a metropolitan area. Thus a private or commercial radiopharmaceutical vendor can operate a cyclotron and distribute the FDG regionally for use at many institutions at a more reasonable cost, obviating the need for a cyclotron at each individual site. FDG has proven to be of even greater value as a tumor-imaging agent than as a cardiac- or brain-imaging agent because it has been found that many malignant neoplasms exhibit increased glucose metabolism and expression of glucose transport proteins relative to normal tissue and thus exhibit increased uptake of FDG on PET scans, as reviewed by Hoh and colleagues.55 Furthermore, FDG PET imaging has been shown to be significantly more sensitive and specific than traditional cross-sectional imaging modalities, such as CT and MRI, for the staging and restaging of many tumors. At present, PET imaging using FDG is a major diagnostic modality used in the diagnosis, initial staging, restaging, and detection of recurrences in a variety of neoplastic disorders, including but not limited to bronchial carcinoma, lymphoma, colorectal carcinoma, malignant melanoma, esophageal carcinoma, and head and neck carcinoma. It is also approved for use in detecting metastatic disease and the recurrence or
treatment monitoring in breast carcinoma (but not for the initial diagnosis or staging of breast carcinoma) and for the detection of occult recurrent, well-differentiated thyroid carcinoma in patients with negative whole-body 131I scans but elevated serum thyroglobulin levels. PET imaging has intrinsically superior spatial resolution and sensitivity than conventional single-photon (i.e., gamma ray) radionuclide imaging. Recent developments in PET scanner technology have resulted in reduced cost and improved imaging capability, including the capability of obtaining whole-body images. PET images are typically evaluated on a computer workstation, which permits interactive evaluation of tomographic images in the coronal, transaxial, and sagittal planes as well as evaluation of rotating cine images of the entire data set using three-dimensional maximum-intensity projection images (MIPs).
treatment monitoring in breast carcinoma (but not for the initial diagnosis or staging of breast carcinoma) and for the detection of occult recurrent, well-differentiated thyroid carcinoma in patients with negative whole-body 131I scans but elevated serum thyroglobulin levels. PET imaging has intrinsically superior spatial resolution and sensitivity than conventional single-photon (i.e., gamma ray) radionuclide imaging. Recent developments in PET scanner technology have resulted in reduced cost and improved imaging capability, including the capability of obtaining whole-body images. PET images are typically evaluated on a computer workstation, which permits interactive evaluation of tomographic images in the coronal, transaxial, and sagittal planes as well as evaluation of rotating cine images of the entire data set using three-dimensional maximum-intensity projection images (MIPs).
During the late 1980s, PET imaging was the subject of a series of reports from the Positron Emission Tomography Panel of the Council on Scientific Affairs of the American Medical Association.24,25,26,27,28 One of these reports26 described the potential impact of PET in the area of oncology, including evaluation of the metabolism and physiology of neoplasms, their effects on adjacent tissues, and development of target sites on tumors, such as monoclonal antibodies and specific growth factors. The unique ability of PET to quantitate these processes will be invaluable in future tumor biology research and in the evaluation of the responses of tumors to therapy.
Subsequent to these early reports, a large body of literature has developed that points to the superiority of FDG PET imaging in the staging and restaging of several neoplasms, as previously noted, as well as its cost effectiveness in this role. PET has been shown to be substantially more accurate in staging many tumors than CT or MRI. In the chest, the major lesions for which PET is routinely used and is Center for Medicare and Medicaid Services–approved include evaluation of solitary pulmonary nodules and in the diagnosis, staging, and restaging of NSCLC, lymphoma, and esophageal carcinoma. Metastatic disease from other FDG-avid tumors—such as malignant melanoma, colorectal carcinoma, and breast carcinoma—are also readily detected. For example, in a multicenter trial of 89 patients, Lowe and coworkers69 found FDG PET imaging to be a highly sensitive technique for the characterization of indeterminate pulmonary nodules identified on CT, with an overall sensitivity and specificity of approximately 90%, using semiquantitation by means of calculating standardized uptake values to compare lesion uptake with surrounding normal tissues. Visual analysis was slightly more sensitive but less specific. False-positive findings may occur in granulomas or in noninfectious inflammatory processes, such as sarcoidosis. False-negative imaging results may occur with cell types that may be associated with lower levels of metabolic activity, such as bronchoalveolar carcinoma and carcinoid tumors, as reported by Higashi and coworkers50 and by Rege and associates,87 respectively. False-negative imaging results or underestimation of the metabolic activity of lesions may also occur in the case of very small pulmonary nodules <7 mm in diameter.
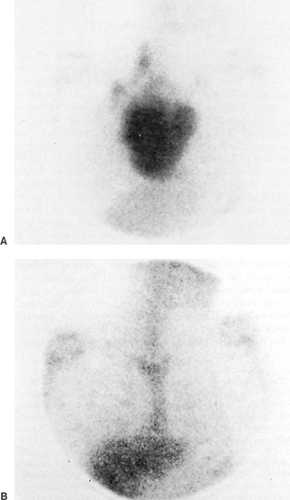
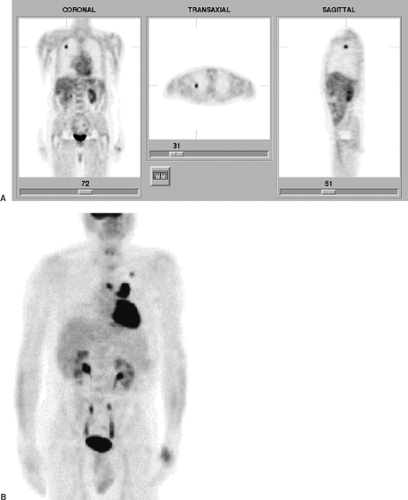
With respect to the mediastinum, the lesions most commonly evaluated by PET include NSCLC, lymphoma, and esophageal carcinoma. In the preoperative staging of NSCLC, one of the key factors is determining the presence or absence of mediastinal or hilar tumor involvement. This information affects not only assessment of operability but also strategies for subsequent treatment and management of the patient. PET has been shown to be superior to CT imaging in this regard, with overall significantly greater sensitivity, specificity, and accuracy, as reviewed by Al-Sugair and Coleman8 and by Bar-Shalom and colleagues.9 CT identifies adenopathy on the basis of size criteria, whereas PET relies on the finding of increased tracer uptake, indicative of increased glucose metabolism within the lesion. Major advantages of PET over CT include the ability to detect tumor involvement in lymph nodes that do not meet CT criteria for pathologic enlargement and the ability to correctly exclude the presence of tumor involvement in enlarged, nonneoplastic nodes identified on CT. Webb and coworkers103 reported the overall sensitivity and specificity of CT in the staging of NSCLC to be only 52% and 69%, respectively. By contrast, as reviewed by Al-Sugair and Coleman,8 numerous studies have shown PET to have sensitivities and specificities for mediastinal lymph node staging in the range of 70% to 90% and 75% to 100%, respectively. Pieterman and associates85 reported a sensitivity and specificity of PET in NSCLC staging of mediastinal involvement of 91% and 86%, respectively, compared with values of 75% and 66% for CT, respectively. Overall, PET was 95% sensitive and 83% specific for the detection of mediastinal involvement and distant metastatic disease. They also found PET to be the only procedure that positively correlated with histopathologic findings in mediastinal lymph nodes and found that the results of the PET study resulted in changes in staging in 62 of 102 patients, raising the stage in 42 and lowering it in 20. Because of the potential for false-positive results secondary to infectious or noninfectious inflammatory processes, such as fungal infection, tuberculosis or sarcoidosis, it is recommended that patients with positive findings in the mediastinum have histologic verification by mediastinoscopy or other methods before surgical management is ruled out. On the other hand, the very high negative predictive value of PET obviates the need for preoperative invasive procedures. Finally, the intrinsic “whole-body” nature of PET imaging also permits the detection of occult distant metastases, such as involvement of the adrenal glands, liver, or skeleton. PET imaging is also extremely valuable in the follow-up assessment of the response to therapy, again outperforming CT in detecting recurrences and differentiating between posttreatment fibrosis versus residual or recurrent tumor involvement. Examples of FDG PET studies in patients with NSCLC are shown in Figure 167-5. FDG PET is also sensitive for the detection of small-cell lung carcinoma; but because of the typically extensive involvement encountered in small-cell carcinoma at initial presentation and its usually poor prognosis, management is often similar for many patients. Therefore it has been more difficult thus far to establish a cost-effective role for PET imaging in this disorder. A more limited role for PET in small-cell lung carcinoma may emerge in the future.
Another common neoplasm involving the mediastinum in which FDG PET imaging plays an important role is lymphoma, including both Hodgkin’s and non-Hodgkin’s lymphoma. Whole-body FDG PET imaging has been shown to be an accurate and cost-effective method of staging or restaging lymphoma relative to CT, MRI, and other conventional staging modalities, as reported by Hoh and associates.56 Kostakoglu and Goldsmith62 found that PET imaging was equivalent or superior to CT for the initial staging of lymphoma. More importantly, as in the case of NSCLC, PET has proven to be superior to CT in the evaluation of patients with lymphoma for the assessment of response to therapy and detection of recurrences. Jerusalem
and associates58 reported that PET found 100% of recurrences in patients with residual soft tissue masses on CT posttreatment, whereas only 26% of PET-negative cases presented with recurrence subsequently. The positive predictive value for recurrence was 100% for PET, as compared with only 42% for CT. PET can also be used for treatment monitoring, since a positive response to therapy may be detected by a decrease in FDG uptake in lesions after as few as one or two cycles of chemotherapy, as reported by Jerusalem and associates.59 An example of the role of PET in the restaging of lymphoma is shown in Figure 167-6. PET has also been shown to be at least as accurate and more likely superior to gallium scintigraphy in this entity, as reported by Willkomm and colleagues107 and later by Mahajan and associates.71 More recently, Bar-Shalom and coworkers10 reported similar findings in comparing gallium scintigraphy to the less sensitive coincidence gamma camera positron imaging technique, in which a standard nuclear medicine gamma camera is modified to detect positron decay using coincidence detection circuitry. As in the case of lung carcinoma, false-negative imaging results may occur with small lesions and in certain cell types, for example, the mucosa-associated lymphoid tumor (MALT) variety, as reported by Hoffmann and associates.53
and associates58 reported that PET found 100% of recurrences in patients with residual soft tissue masses on CT posttreatment, whereas only 26% of PET-negative cases presented with recurrence subsequently. The positive predictive value for recurrence was 100% for PET, as compared with only 42% for CT. PET can also be used for treatment monitoring, since a positive response to therapy may be detected by a decrease in FDG uptake in lesions after as few as one or two cycles of chemotherapy, as reported by Jerusalem and associates.59 An example of the role of PET in the restaging of lymphoma is shown in Figure 167-6. PET has also been shown to be at least as accurate and more likely superior to gallium scintigraphy in this entity, as reported by Willkomm and colleagues107 and later by Mahajan and associates.71 More recently, Bar-Shalom and coworkers10 reported similar findings in comparing gallium scintigraphy to the less sensitive coincidence gamma camera positron imaging technique, in which a standard nuclear medicine gamma camera is modified to detect positron decay using coincidence detection circuitry. As in the case of lung carcinoma, false-negative imaging results may occur with small lesions and in certain cell types, for example, the mucosa-associated lymphoid tumor (MALT) variety, as reported by Hoffmann and associates.53
Finally, PET imaging has developed an increasing role in the initial staging and follow-up of patients with esophageal carcinoma. In normal studies, faint uptake may be seen in the distal esophagus, which may represent a normal variant, or in some
cases may reflect mild inflammatory changes secondary to gastroesophageal reflux. As recently reviewed by Kostakoglu and associates,62 FDG PET is sensitive for the detection of both squamous cell and adenocarcinoma of the esophagus, except for small (<5 mm) T1 tumors, PET was 30% sensitive and 90% specific for the detection of weighted lesions. PET is approximately 80% sensitive and 95% specific overall in esophageal carcinoma, and detects occult distant metastases missed by CT in approximately 20% of cases, as reported by Block and associates17 and by Yeung and coworkers.113 Neither PET nor CT is sensitive for the staging of mediastinal nodal involvement, although PET is more accurate than CT in this regard. Yoon and associates114 recently reported a series of 81 patients who underwent preoperative PET and CT imaging. For the detection of the primary
lesions, PET correctly identified the primary lesion in 91% of patients, compared with 80% for CT. For staging of lymph node involvement, PET was 30% sensitive and 90% specific for detection of nodal involvement at the time of preoperative evaluation, compared with only 11% sensitivity for CT. CT was slightly more specific than PET, with 95% specificity, but overall accuracy was nearly equal. With respect to thoracic nodal involvement, PET detected 31% of the positive nodes found at surgery, compared with only 3% for CT. Again, PET is also superior to CT for detection of recurrent disease and in predicting the response to neoadjuvant therapy, as reported by Kelly and colleagues.61 The response to preoperative chemotherapy and radiation therapy, as judged by PET imaging, may prove to be a useful indicator for the stratification of patients for subsequent medical versus surgical management. Examples of primary and metastatic esophageal carcinoma are shown in Fig. 167-7.
cases may reflect mild inflammatory changes secondary to gastroesophageal reflux. As recently reviewed by Kostakoglu and associates,62 FDG PET is sensitive for the detection of both squamous cell and adenocarcinoma of the esophagus, except for small (<5 mm) T1 tumors, PET was 30% sensitive and 90% specific for the detection of weighted lesions. PET is approximately 80% sensitive and 95% specific overall in esophageal carcinoma, and detects occult distant metastases missed by CT in approximately 20% of cases, as reported by Block and associates17 and by Yeung and coworkers.113 Neither PET nor CT is sensitive for the staging of mediastinal nodal involvement, although PET is more accurate than CT in this regard. Yoon and associates114 recently reported a series of 81 patients who underwent preoperative PET and CT imaging. For the detection of the primary
lesions, PET correctly identified the primary lesion in 91% of patients, compared with 80% for CT. For staging of lymph node involvement, PET was 30% sensitive and 90% specific for detection of nodal involvement at the time of preoperative evaluation, compared with only 11% sensitivity for CT. CT was slightly more specific than PET, with 95% specificity, but overall accuracy was nearly equal. With respect to thoracic nodal involvement, PET detected 31% of the positive nodes found at surgery, compared with only 3% for CT. Again, PET is also superior to CT for detection of recurrent disease and in predicting the response to neoadjuvant therapy, as reported by Kelly and colleagues.61 The response to preoperative chemotherapy and radiation therapy, as judged by PET imaging, may prove to be a useful indicator for the stratification of patients for subsequent medical versus surgical management. Examples of primary and metastatic esophageal carcinoma are shown in Fig. 167-7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree