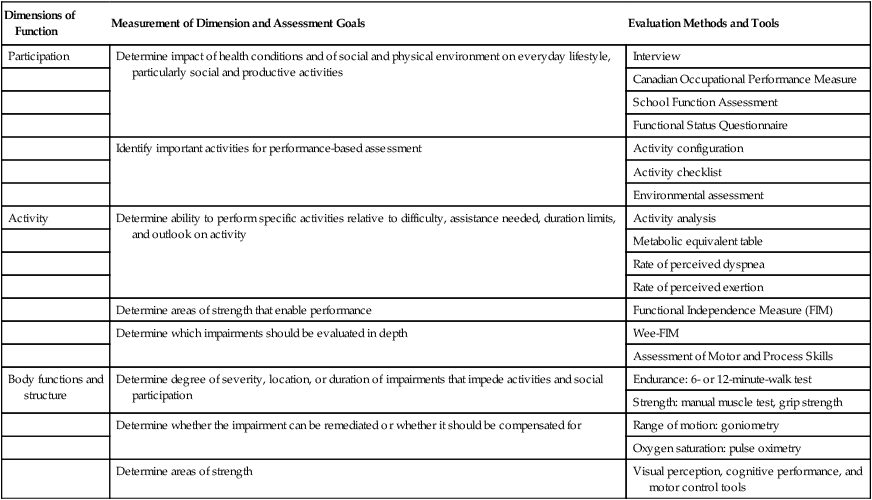
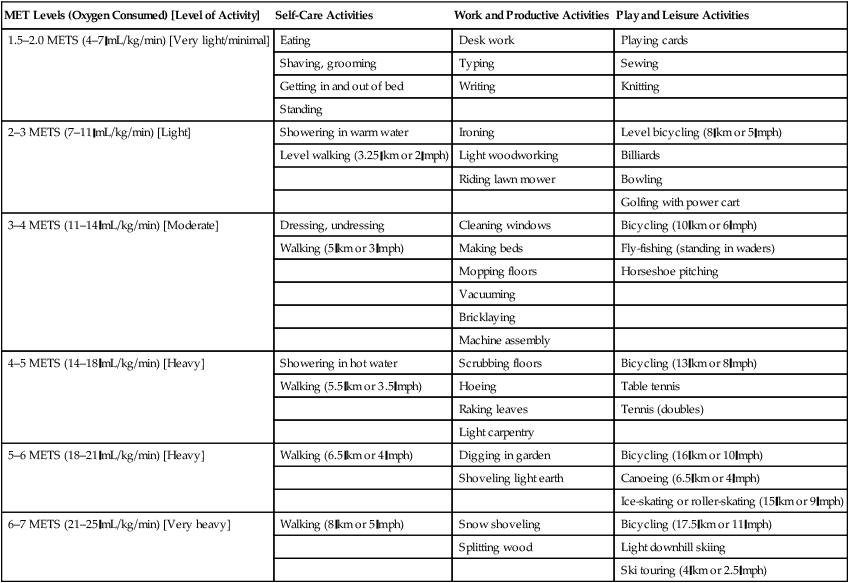
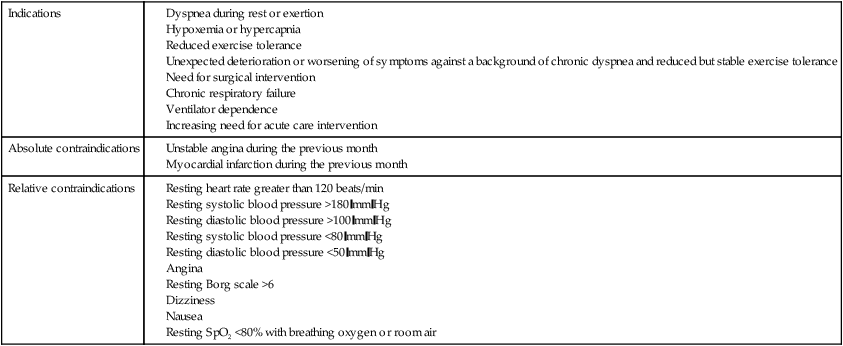
Chapter 27 1. Identify pertinent interview information that would guide the initial exercise program and the progression of exercise. 2. Perform a 6-minute-walk test (6MWT). 3. Calculate a patient’s target heart rate (THR). 4. Explain and use the dyspnea scale. 5. Explain and use the Borg scale. 6. Instruct a patient on the proper method for pursed-lip breathing (PLB). 7. Instruct a patient on the proper method for diaphragmatic breathing (DB). 8. Instruct a patient on the proper method for active cycle of breathing technique (ACBT). 9. Instruct a patient on the proper method for autogenic drainage (AD). 10. Instruct a patient with a weak diaphragm on the proper method for the use of an inspiratory muscle trainer (IMT). Pulmonary rehabilitation is an integral part of keeping a patient healthy at his or her home. The respiratory therapist (RT), who strives to keep a discharged patient strong and focuses on helping him or her function at home, must understand the importance of patient education regarding pulmonary rehabilitation. When patients understand the importance of the techniques and activities that will help them get and stay fit, they will successfully return to a functional strength and to a status where activities of daily living (ADLs) are attainable. Patient goals are developed with the help of the RT. They must be realistic and agreeable to the patient. Some common educational topics discussed in pulmonary rehabilitation are listed in Box 27-1. A clear understanding of these goals and a discussion of progress toward them should involve the patient’s family as well. Examples of goals may be resuming a leisure activity that the patient once enjoyed, returning to work, or participating more in family responsibilities. Teaching patients to recognize how they feel, preparing them to use the tools that help cope with shortness of breath (SOB), and facilitating in rebuilding their strength and endurance are ways that pulmonary rehabilitation can decrease hospitalizations and prevent readmissions. The most common cause of intensive care unit (ICU) readmission is a pulmonary problem. Boxes 27-2 and 27-3 list patient characteristics and risk factors associated with ICU readmissions. This is important not only for the individual but also for the hospital financially, since Medicare now has a 30-day readmission criterion for reimbursement. Common goals for a pulmonary rehabilitation program are listed in Box 27-4. The patient’s medication regimen, oxygen saturation at rest, nutrition, and fluid status must also be evaluated before starting any exercise. Functional status is often assessed using activities of daily living (ADLs). See Tables 27-1 and 27-2 for examples of this assessment. Vaccines are important to protect patients from common infections. If patients are vaccinated, they are less likely to be readmitted with an exacerbation of their underlying pulmonary condition. If their vaccination status is not up to date, provide instructions on how and where to get vaccinated. TABLE 27-1 Occupational Therapy Multidimensional Functional Assessment* *Organized according to International Classification of Functioning and Disability (ICF) Dimensions of Function: Participation, Activity, and Body Functions and Structure Data from International Classification of Functioning, Disability and Health (ICF): http://www.who.int/classifications/icf/en/. Accessed January 2008. (In Hodgkin JE, Celli BR, Connors GL, editors: Pulmonary rehabilitation: guidelines for success, ed 4, St. Louis, MO, 2009, Mosby.) TABLE 27-2 Metabolic Equivalent Values for Some Occupational Performance Areas Schell BA, Scaffa M, Gillen G and Cohn ES: Willard & Spackman’s Occupational therapy, ed 12, Philadelphia, 2013, Lippincott, Williams and Wilkins, Inc. As an RT, you will interview patients entering pulmonary rehabilitation. Information you gather will allow you to structure a program to meet your patient’s specific needs. Performance of the 6MWT may provide a baseline for exercise prescription. Initially, pulmonary rehabilitation may be done in the hospital setting. However, it is typically done on an out-patient basis. Indications and contraindications for the 6MWT are given in Table 27-3. The Borg scale is commonly used to assess dyspnea, perceived level of exertion, and pain. An adaptation of this scale is given in Table 27-4. TABLE 27-3 Indications and Contraindications for a 6MWT
Pulmonary Rehabilitation
Equipment
 A chair that can be easily moved along the walking course
A chair that can be easily moved along the walking course
 Automated electronic defibrillator
Automated electronic defibrillator
 Borg scales (level of perceived exertion, modified dyspnea)
Borg scales (level of perceived exertion, modified dyspnea)
 Countdown timer (or stopwatch)
Countdown timer (or stopwatch)
 Two small cones to mark the turnaround points
Two small cones to mark the turnaround points
Patient Interviewing: Review
Dimensions of Function
Measurement of Dimension and Assessment Goals
Evaluation Methods and Tools
Participation
Determine impact of health conditions and of social and physical environment on everyday lifestyle, particularly social and productive activities
Interview
Canadian Occupational Performance Measure
School Function Assessment
Functional Status Questionnaire
Identify important activities for performance-based assessment
Activity configuration
Activity checklist
Environmental assessment
Activity
Determine ability to perform specific activities relative to difficulty, assistance needed, duration limits, and outlook on activity
Activity analysis
Metabolic equivalent table
Rate of perceived dyspnea
Rate of perceived exertion
Determine areas of strength that enable performance
Functional Independence Measure (FIM)
Determine which impairments should be evaluated in depth
Wee-FIM
Assessment of Motor and Process Skills
Body functions and structure
Determine degree of severity, location, or duration of impairments that impede activities and social participation
Endurance: 6- or 12-minute-walk test
Strength: manual muscle test, grip strength
Determine whether the impairment can be remediated or whether it should be compensated for
Range of motion: goniometry
Oxygen saturation: pulse oximetry
Determine areas of strength
Visual perception, cognitive performance, and motor control tools
MET Levels (Oxygen Consumed) [Level of Activity]
Self-Care Activities
Work and Productive Activities
Play and Leisure Activities
1.5–2.0 METS (4–7 mL/kg/min) [Very light/minimal]
Eating
Desk work
Playing cards
Shaving, grooming
Typing
Sewing
Getting in and out of bed
Writing
Knitting
Standing
2–3 METS (7–11 mL/kg/min) [Light]
Showering in warm water
Ironing
Level bicycling (8 km or 5 mph)
Level walking (3.25 km or 2 mph)
Light woodworking
Billiards
Riding lawn mower
Bowling
Golfing with power cart
3–4 METS (11–14 mL/kg/min) [Moderate]
Dressing, undressing
Cleaning windows
Bicycling (10 km or 6 mph)
Walking (5 km or 3 mph)
Making beds
Fly-fishing (standing in waders)
Mopping floors
Horseshoe pitching
Vacuuming
Bricklaying
Machine assembly
4–5 METS (14–18 mL/kg/min) [Heavy]
Showering in hot water
Scrubbing floors
Bicycling (13 km or 8 mph)
Walking (5.5 km or 3.5 mph)
Hoeing
Table tennis
Raking leaves
Tennis (doubles)
Light carpentry
5–6 METS (18–21 mL/kg/min) [Heavy]
Walking (6.5 km or 4 mph)
Digging in garden
Bicycling (16 km or 10 mph)
Shoveling light earth
Canoeing (6.5 km or 4 mph)
Ice-skating or roller-skating (15 km or 9 mph)
6–7 METS (21–25 mL/kg/min) [Very heavy]
Walking (8 km or 5 mph)
Snow shoveling
Bicycling (17.5 km or 11 mph)
Splitting wood
Light downhill skiing
Ski touring (4 km or 2.5 mph)
» Skills Check List
27-1 Performing the 6-Minute-Walk Test
Indications
Absolute contraindications
Relative contraindications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pulmonary Rehabilitation




























