Pulmonary arterial hypertension (PAH).
Pulmonary venous hypertension.
Disorders of the respiratory system or hypoxemia or both.
Chronic thrombotic or embolic disease.
Disorder directly affecting the pulmonary vasculature.
patients with anemia, including thalassemia and sickle cell disease; those with hyperthyroidism; and those who are obese. Each of these conditions is associated with a marked increase in pulmonary blood flow that could be a trigger, but the association is not clear.
TABLE 35.1. Classification, diseases, and triggers associated with pulmonary hypertension as modified from the WHO classification | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 35.2. Common presenting symptoms and signs in pulmonary hypertension, depending on related disease | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Dyspnea and fatigue are correlated with decrease in rest and exercise stroke volume, cardiac output, and oxygen transport.
Angina-like chest pains on exertion are correlated with increased right ventricular (RV) myocardial oxygen demand and pulmonary artery pressures in excess of aortic pressure.
Presyncope and syncope and postural, tussive, and exercise systemic hypotension are correlated with decreased RV filling, decreased left ventricular (LV) filling, and LV compression by the right ventricle.
Abdominal pain, anorexia, edema, and ascites are correlated with gastric distention, increasing venous pressure, tricuspid insufficiency, and RV diastolic dysfunction.
Raynaud phenomenon is characteristically found in patients with scleroderma-related disorders and in 10% of patients with PPH.
TABLE 35.3. World Health Organization pulmonary hypertension functional assessment classification | ||||
|---|---|---|---|---|
|
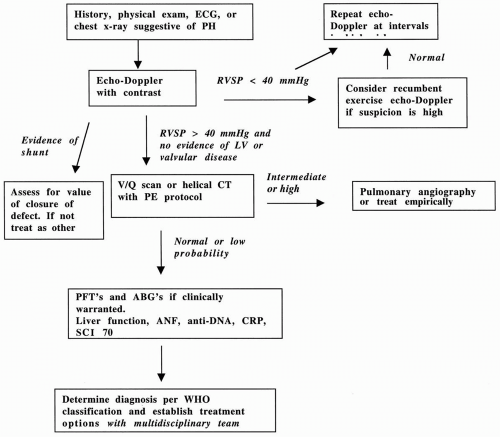
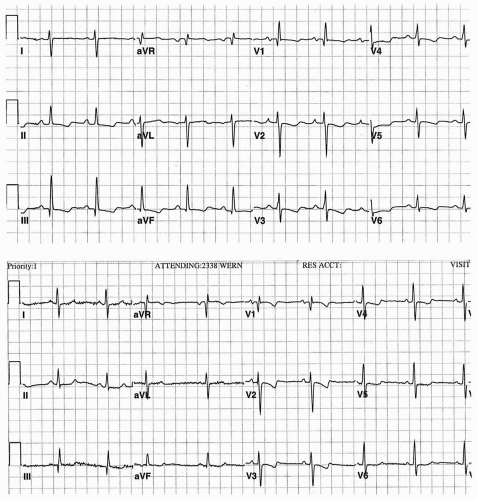
Frequent misdiagnoses include inferior, anterior, and septal infarction; inferior and anterior ischemia; and left posterior fascicular block. The ECG is not an effective screening tool in asymptomatic or mildly symptomatic persons. The most common ECG patterns in PH include a right-axis deviation of the QRS interval of more than 90 degrees, a qR in V1, a right-axis deviation, and increased voltage (more than 2.5 mm) of the p wave in lead II. The increased voltage is associated with a fourfold increase in mortality rate (3). Atrial premature beats occur frequently, but atrial fibrillation, atrial flutter, and serious ventricular arrhythmias are not common. The upper ECG tracing in Figure 35.2 demonstrates the typical ECG findings in PPH. It was obtained in a 37-year-old woman with WHO class IV PPH. Her pretreatment mean pulmonary artery pressure (mPA) was 75 mm Hg, and her pulmonary vascular resistance (PVR) was 24 Wood units. The lower ECG tracing is after 2 years of treatment with intravenous epoprostenol, at which point her disease was WHO class I, her mPA was 30 mm Hg, and her PVR was 6 Wood units. After treatment, less QRS right-axis deviation (120 degrees vs. 90 degrees), lower R-wave voltage in V1 to V3, and persistent but less ST-segment abnormality of RV strain or ischemia are seen.
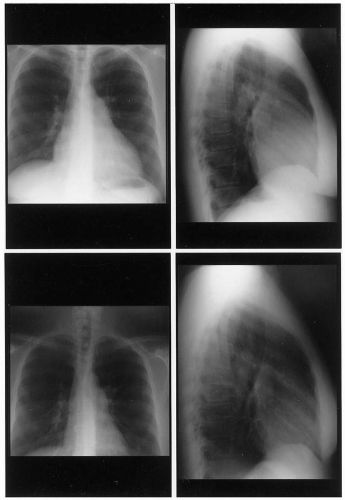
usually detectable on the chest radiograph. Chest radiographic indicators of PH include enlargement of the right ventricle, the right atrium, the superior vena cava, and the main pulmonary artery and its major branches. The criteria for PH are found in 95% of patients with PPH and only 4% of controls matched for age, gender, and bodysurface area. Figure 35.3 demonstrates the baseline and on-treatment chest radiograph in the 37-year-old woman with PPH described previously.
ventricle (4). Pericardial effusions are not common but may be predictive of a poor outcome. Doppler findings include significant tricuspid and pulmonic regurgitation, from which the RVSP and pulmonary artery diastolic pressures can be calculated.
TABLE 35.4. Recommended schedule for Doppler echocardiography for the detection of pulmonary hypertension in persons at high risk | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||
amenable to immunosuppressive therapy. The CT scan can detect PH in parenchymal lung disease. A main pulmonary artery diameter larger than 29 mm has a sensitivity of 87%, a specificity of 89%, and a positive predictive value of 0.97 for identifying patients with an mPA of more than 20 mm Hg (6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree