LEARNING OBJECTIVES
Learning Objectives
The student will be able to list the indications for mechanical ventilation (MV).
The student will be able to describe common modes of MV, frequently used ventilator settings, and waveform monitoring of airway pressures during MV.
The student will be able to describe the process of ventilator weaning and eventual liberation of patients from MV.
The student will be able to distinguish alternative modes of MV and the basic principles of non-invasive ventilation.
The Greek physician and philosopher Claudius Galen (129-199 ce) was the first to artificially reproduce the process of ventilation. He inflated the lungs of a dead animal with bellows during one of his numerous experiments, subsequently described in his iconic text, On the Parts of the Human Body. It was not until more than 1,500 years later that the paradigm of artificial respiration was used for human resuscitation. The first seemingly authentic report was by Tossach in 1744 concerning the resuscitation of a suffocated miner by mouth-to-mouth technique. Again, it was not until the dreaded poliomyelitis epidemics of the 1940s and 1950s in Europe and the United States that mechanical ventilation (MV) was developed as a major therapeutic strategy. Since then, the science of MV has rapidly expanded to encompass a variety of modalities that ensure adequate ventilation and gas exchange by a diverse array of mechanical and physiologic processes. Simultaneously, there has been increasing awareness that unregulated inflation of the lungs may lead to deleterious consequences. Those include excessive stretch and shear forces at the alveolar level that cause physiologically harmful effects on both the respiratory and cardiovascular systems (Chap. 28).
INDICATIONS FOR MECHANICAL VENTILATION
Mechanical ventilation is indicated in any clinical situation where hypoxemia or hypercarbia secondary to underlying abnormal or dysfunctional lung pathophysiology cannot be corrected by spontaneous respiration. Often MV is initiated when lung gas exchange is normal but protection of the anatomical airway by a cuffed endotracheal tube is necessary, to prevent aspiration of oropharyngeal or gastrointestinal contents. This commonly occurs in the setting of a decreased consciousness with depressed protective laryngeal reflexes and incomplete glottic inlet closure (Chap. 11). Finally, MV may be necessary when the work of breathing, while sufficient to eliminate CO2 in cases of severe metabolic acidosis, leads to tachypnea and respiratory muscle fatigue. A prime example of such a scenario is severe sepsis, wherein endotracheal intubation and MV are initiated to avoid impending respiratory failure secondary to excessively high work of breathing. Used in this way, MV decreases both respiratory muscle fatigue and myocardial O2 requirements and thereby promotes clinical recovery. Other indications for initiating MV are to regulate Paco2 in patients with increased intracranial pressure, or to provide an air splint in patients with massive chest injury and flail chest.
REVIEW OF THE MECHANICS OF VENTILATION
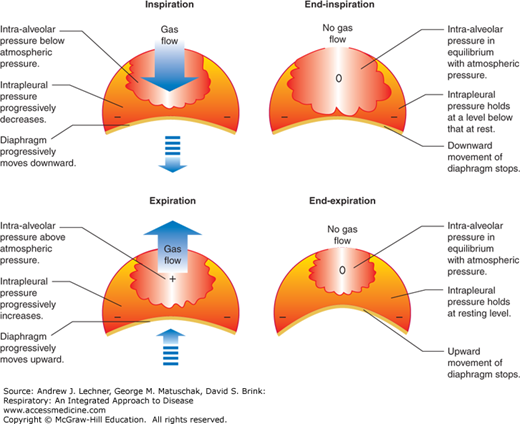
Normal respiration involves the active process of inspiration, created by the generation of negative intrapleural pressure caused by caudal diaphragmatic movement. Expiration is ordinarily a passive process, whereby the diaphragm returns to its baseline position. This differential pressure gradient between the pleural space and the alveolar airspaces causing normal inspiration and expiration is schematically represented in Fig. 30.1.
In general, mechanical ventilation includes two basic designs or subtypes:
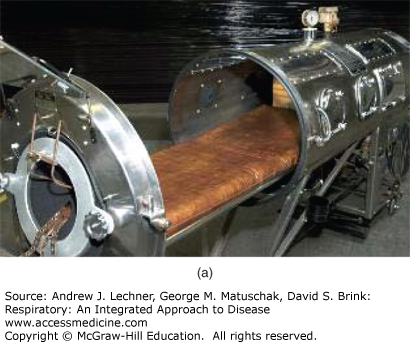
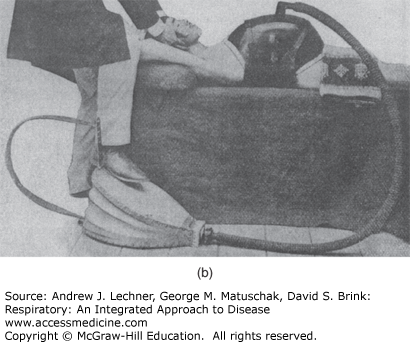
Negative pressure ventilation: Historically the chest or the entire body below the neck was surrounded by a device capable of creating a cyclical partial vacuum that enhanced the normally negative gradient between PIP and PAW. Inspiration was initiated by this partial vacuum, and expiration occurred when the negative pressure was released. Primary examples of negative pressure ventilation included the iron lung and cuirass shell ventilators (Fig. 30.2). Such forms of ventilation are rarely used today.
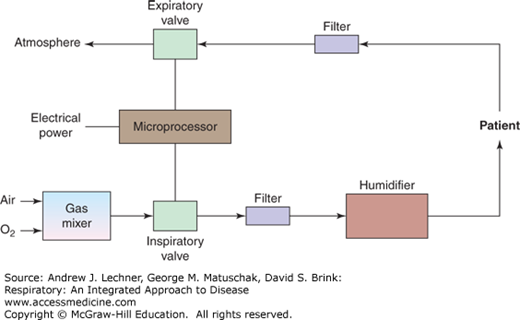
Positive pressure ventilation: A piston-based system of valves controlled by a microprocessor creates positive PAW relative to PB during inspiration, while expiration is a passive process caused by lung and chest wall recoil. This is the current standard of all modern mechanical ventilators, with the exception of some forms of high-frequency ventilation in which expiration is an active process. Components of a simple ventilation system are diagrammed in Fig. 30.3.
FIGURE 30.2
(a) The Emerson iron lung, circa 1950. The patient lies within the chamber with only his/her head outside, which when sealed provides an effectively oscillating atmospheric pressure. (b) The cuirass shell ventilator, circa 1905, which applied negative pressure to the thorax by means of a foot-operated bellows.
MODES OF POSITIVE PRESSURE MECHANICAL VENTILATION
Conventional ventilator modes typically involve limiting either the maximal or peak airway pressure (PPEAK) or the maximal inspired tidal volume (VT) that the patient receives. Newer ventilators have expanded on this traditional approach by creating hybrid modes, wherein both PPEAK and VT can be regulated to some degree. This chapter will focus on the more established modes of each.
Volume-controlled ventilation: Also known as volume-limited ventilation or volume-targeted ventilation, this mode involves setting VT, respiratory f, and the inspiratory flow rate to specific values, while PPEAK is allowed to vary on a breath-to-breath basis. Thus the ventilator delivers a consistent VT, either at the set rate (controlled breath) or when inspiratory effort is initiated by the patient (assisted breath). In the latter, the inspiratory time interval and thereby the inspiratory time/expiratory time ratio (I:E ratio) will vary based upon the patient’s spontaneous f. Although VT had been conventionally set at 10-12 mL/kg of predicted body weight (PBW) for patients without lung injury, recent trials have validated the use of lower VT that are closer to 6 mL/kg of PBW in patients with ALI or ARDS (Chap. 28). When VT, PAW, and flow rates are plotted versus time in this ventilator mode, the waveforms for each resemble those in Fig. 30.4.
Pressure-controlled ventilation: Also referred to as pressure-limited ventilation or pressure-targeted ventilation, this mode involves setting an upper limit on PPEAK during inspiration, while manipulating f and thus the I:E ratio. As a result, VT fluctuates on a breath-to-breath basis, based upon the patient’s dynamic lung and chest wall compliance. The ventilator is limited by the set inspiratory PPEAK, and again will either ventilate the patient at a set rate (controlled breath) or whenever breathing is initiated or attempted by the patient (assisted breath). In the latter variation, the flow rate at which VT is delivered also remains variable, based upon a patient’s effort and demand. Presetting inspiratory time to exceed the expiratory time is termed inverse-ratio pressure control ventilation. It is less commonly used in clinical practice, except in severe ARDS for salvage therapy or to reduce ventilator-induced lung injury (VALI) (Chap. 28). Typical waveforms for PAW, flow rate, and delivered VT during pressure-controlled ventilation are depicted in Fig. 30.5.
Pressure support ventilation (PSV): The PSV mode involves assisting a patient’s spontaneous respiratory effort by the ventilator, up to a preset level of inspiratory pressure. Since the patient must initiate a spontaneous breath before assistance is delivered, setting an inspiratory support pressure is all that is required. Therefore, patient effort decides the respiratory rate, flow rate and VT

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree