INTRODUCTION TO ASTHMA AND ITS EPIDEMIOLOGY
Learning Objectives
The student will be able to describe the epidemiology of asthma in the United States, and list the known or suspected risk factors and triggers for asthma.
The student will be able to explain the immunopathogenesis of asthma.
The student will be able to distinguish the clinical features of asthma from other cardiopulmonary disorders.
The student will be able to develop an evidence-based evaluation and management plan for patients with asthma.
Asthma is a complex disorder characterized by variable and recurring symptoms, airflow obstruction, bronchial hyperresponsiveness, and underlying airway inflammation. Asthma is one of the most common chronic diseases globally and domestically, affecting 23 million individuals and including 7 million in the United States alone. The prevalence of asthma has been increasing since the early 1980s across all age, gender, and racial groups. Asthma is the most common chronic disease in children and affects more children (7%-10%) than adults (3%-5%). Prevalence by gender varies by age, being more common in boys than girls in childhood but more common in women than men in adulthood. The slightly higher prevalence of asthma among African Americans and Puerto Ricans than Caucasians is highly correlated with socioeconomic status (ie, poverty, urban air quality, indoor allergens, lack of patient education, and inadequate medical care).
Asthma is associated with increased morbidity. Approximately 10 million ambulatory care visits, 2 million emergency department visits, and half a million hospitalizations annually are attributed to asthma. In fact, asthma is the third-ranking cause of hospitalization in children. It is also the leading cause of school absenteeism among children, accounting for >14 million total missed days of school. Meanwhile, in terms of risk by ethnicity, African Americans are also three times more likely to be hospitalized from asthma.
Asthma is also a major cause of mortality. It is the primary cause of more than 4,000 United States annual deaths due to asthma and is a contributing factor for nearly 7,000 other deaths annually. Despite improvements in the understanding of the pathophysiology and the expansion of available effective therapies, overall asthma death rates continue to increase by 50% among all genders, age groups, and ethnic groups since the 1980s. In addition, mortality rates for children younger than 19 years old have increased by nearly 80% percent since then. Mortality rates are higher in women, accounting for nearly 65% of all asthma deaths. African Americans are also three times more likely to die from asthma. In fact, mortality rates are highest in African-American women, whose rate is 2.5 times higher than that of Caucasian women. Aside from gender and ethnicity, risk factors for increased asthma mortality include severe airflow obstruction, multiple recent emergency department visits or hospitalizations in the past year, history of intubation or ICU admission in the past five years, nonuse of inhaled corticosteroids, current smoking, psychosocial stress and depression, socioeconomic factors, and attitudes and beliefs regarding medications.
The adverse health outcomes from asthma also impose a major socioeconomic burden. It is estimated that asthma costs the United States $18 billion dollars, $10 billion from direct health care costs and $8 billion from lost productivity due to illness and death. Thus, public health efforts to improve socioeconomic conditions and access to medical care are needed to address this disparity in asthma health outcomes.
There are myriad factors that precipitate and aggravate asthma (Table 21.1). Indoor airborne allergens such as house dust mites, molds, cockroaches, animal/pet dander are well known triggers that may be amenable to environmental modification. Acute viral bronchiolitis due to rhinoviruses not only increase the number of wheezing episodes early in life but also increase the risk of asthma at the age of 6 years. Viral respiratory infections also commonly precipitate exacerbations in asthmatic patients, who may be vulnerable based on epithelial deficiencies in antiviral activity and the integrity of the airway epithelial barrier. Fetal exposure to environmental tobacco smoke (ETS) is an independent risk factor for poor lung function, wheezing, and the development of asthma. Both ETS and personal smoking were significantly related to asthma and wheeze in teenagers. In addition, smoking is associated with decreased asthma control and increased risk of mortality and asthma attacks and exacerbations in adults. Asthmatics should be encouraged to abstain from smoking since cessation is associated with improvements in both asthma and lung function. Heavy exertion (eg, sports activity), particularly in cold, dry weather conditions, can trigger bronchospasm in patients with exercise-induced asthma.
| Airborne Allergens | Occupational Exposures | Diet, Lifestyle |
|---|---|---|
| House dust mite (Dermatophagoides) | Dusts (mineral, plant, etc) | Specific foods |
| Mold (Alternaria, Aspergillus, etc) | Vapors and fumes | Additives, preservatives |
| Cockroach (including feces) | Other irritants | Tobacco smoke |
| Animal dander | Air pollution | Exercise |
| Pollen (seasonal) | ||
| Drugs | Endocrine Factors | Co-morbidities |
| Aspirin, NSAIDs | Menstruation | Rhinosinusitis |
| β-blockers | Pregnancy | Gastroesophageal reflux |
| Psychological Factors | Respiratory Viruses |
Occupational asthma (OA) is defined as new asthma or the recurrence of previously quiescent asthma induced by either sensitization to a specific substance (eg, an inhaled protein) or a chemical at work (sensitizer-induced OA) or by exposure to an inhaled irritant at work (irritant-induced OA). Epidemiological studies reveal an association between the increase in the incidence of allergic respiratory diseases and bronchial asthma in urban populations and the increased presence of outdoor air pollutants resulting from more intense energy consumption and exhaust emissions from cars and other vehicles. Psychogenic stress not only influences the symptoms but also complicates the management of asthma. For example, depressed patients may lack the motivation to adhere to an asthma action plan, while anxious asthmatics who hyperventilate can develop bronchospasm. Five percent of asthmatics are allergic to aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) and when combined with nasal polyposis is a condition known as the Samter triad. Meanwhile, asthma symptoms appear to worsen in 30%-40% of asthmatic women during the perimenstrual period. During pregnancy, a third of asthmatic women develop worse symptoms while another third report an improvement in symptoms. Pregnant women with uncontrolled asthma have been reported to have higher risks of several complications of pregnancy, including preeclampsia, preterm birth, infants with low birth weight or intrauterine growth restriction, infants with congenital malformations, and perinatal death. Dietary intake of certain foods (eg, shellfish), food additives, and preservatives (eg, sulfites) trigger asthma in hypersensitive individuals. Comorbid conditions such as allergic rhinitis and gastroesophageal acid reflux commonly play an aggravating role in asthma symptoms.
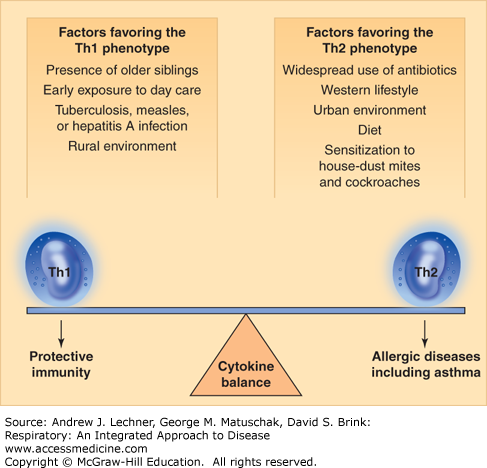
The immunopathogenesis of asthma is thought to be due to the promotion of the allergic asthmatic phenotype resulting from the predominance of Th2 over Th1 cytokine response during early life, also referred to as the Hygiene Hypothesis (Fig. 21.1). This theory stemmed from the observation of increasing prevalence of asthma in industrialized Western societies. Early childhood exposures in these industrialized countries favoring the Th2 response include widespread use of antibiotics, an urban rather than rural environment, and sensitization to cockroaches, which are believed to lead to the development of the allergic asthmatic phenotype. On the other hand, the higher propensity for microbial exposure in developing countries with increased prevalence of infections from Mycobacterium tuberculosis, measles virus, and hepatitis A virus all enhance Th-1 mediated responses which reduce the development of an atopic/allergic immunologic phenotype. Other factors believed to be protective against the asthma phenotype include contact with other siblings and attendance at a day-care facility during the first 6 months of life.
The diagnosis of asthma is based on the presence of episodic symptoms of completely or partially reversible airflow obstruction and/or airway hyperresponsiveness, and only with exclusion of alternative diagnoses. The evaluation includes at least a detailed medical history, physical exam, and spirometry. Additional studies may also be indicated, such as a full pulmonary function test (PFT) combined with a methacholine bronchoprovocation challenge (see below) and chest imaging studies (Chaps. 15 and 16). Symptoms consistent with asthma include: chronic episodic cough that is worse particularly at night; recurrent difficulty in breathing or chest tightness; and recurrent wheezing upon expiration (Chap. 14). However, symptoms may vary depending on the severity of asthma. Severe asthmatics may present having all of the symptoms listed, while patients with mild asthma may complain of just one symptom such as intermittent cough (the so-called cough-variant asthma).
Physical examination findings in patients with uncontrolled asthma or an acute asthma exacerbation include tachypnea, use of the accessory muscles of respiration, audible wheezing, and a prolonged forced expiratory phase. However, given the episodic nature of the airflow limitation in asthma, many patients with intermittent, mild, or even moderate asthma may have a completely normal physical exam. It is also important to emphasize that even in patients with severe disease, lack of wheezing does not exclude asthma, since reduced airflow may attenuate chest physical findings. Physical signs of atopy such as nasal congestion and drainage and/or nasal polyps and eczema may help support a diagnosis of allergic asthma.
Spirometry is the clinical mainstay to objectively confirm the reversibility of airflow obstruction in patients with asthma (Chap. 16). Given the normal decline in spirometric airflow measures with aging, the National Asthma Education and Prevention Program (NAEPP) guidelines recommend using age-adjusted FEV1/FVC thresholds for determining the presence of airflow obstruction (Table 21.2). The FEV1/FVC is calculated by dividing the actual FEV1 in liters (not the percent of predicted) by the actual FVC in liters and multiplying the resulting ratio by 100%. An FEV1/FVC below the lower limits of normal (LLN) for a patient’s age confirms the presence of airflow obstruction, and also indicates asthma that is not well-controlled. To confirm the reversibility of airflow obstruction after baseline spirometry shows airflow obstruction, a short-acting bronchodilator such as albuterol is administered at a dose of up to 500 μg either by metered-dose inhaler or by nebulization. A postbronchodilator increase in the actual FEV1 of ≥12% and ≥200 mL above the pre-bronchodilator baseline indicates at least partial reversibility of airflow obstruction.
Measurement of peak expiratory flow rate (PEFR) using an inexpensive portable device has been employed in the diagnosis and monitoring of asthma. An improvement in PEFR before and after bronchodilator administration of 60 L/min or 20%, a 20% day-to-day PEFR variability, or a >10% intraday PEFR variability when measured twice daily are suggestive evidence of asthma. However, peak flows are highly effort-dependent and variable, making them less reliable than spirometrically derived airflow measurements. Despite its limitations, PEFR measurement may be useful for monitoring airflow limitation in patients with poor perception of their asthma symptoms. The PEFR is also useful in identifying environmental triggers, and in documenting work-related asthma. Additional pulmonary function tests are not routinely necessary unless other pulmonary conditions are suspected, for example, a reduced DLCO in COPD or a limitation of the inspiratory flow-volume loop in vocal chord dysfunction (Chaps. 16 and 33).
In patients with normal baseline spirometry, a bronchoprovocation challenge test can be employed to demonstrate the bronchial hyperresponsiveness or airway hyperreactivity typical of asthma. The degree of bronchial hyperresponsiveness is classified based on the [methacholine] provoking a ≥20% reduction in FEV1 or FVC (PC20). A PC20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree