INTRODUCTION TO LUNG STRUCTURE
Learning Objectives
The student will be able to describe the architectural layers, components, and relationships to adjacent tissue of all major elements of the normal respiratory system, including nasal cavities, sinuses, oropharynx, larynx, bronchi, and lungs.
The student will be able to recognize the histologic appearance of all major elements of the normal respiratory system.
The student will be able to describe the major stages of lung development and the gestational ages when these milestones normally occur.
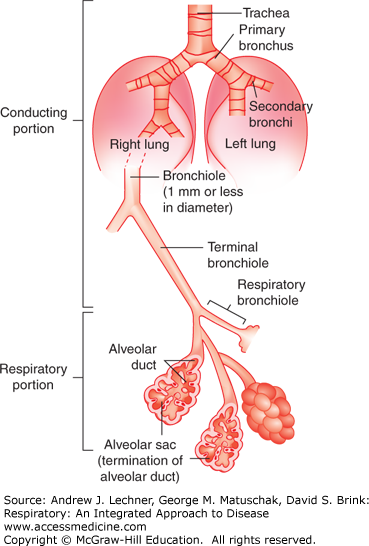
The respiratory system is classically divided into two parts, based on their structures and functions. The first is the conducting zone, being the organized array of progressively smaller airways through which air moves into and out of the lungs during tidal ventilation. The conducting zone starts at the nares (and/or mouth) and includes the nasal cavities, pharynx, larynx, trachea, bronchi, and bronchioles. The second part is the respiratory parenchyma, being the densely packed collection of membrane walls, thin enough to support molecular diffusion between the inspired air and blood coursing through the microvasculature of the lung (Fig. 2.1). Constituents of the respiratory parenchyma begin where the conducting zone ends and include the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. The gross and microscopic appearances of each component are the primary focus of this chapter, with the principal functions for each presented with more detail in subsequent chapters.
The major histologic features of each constituent of the respiratory tract are broadly summarized in Table 2.1. Within the lungs are blood and lymphatic vessels and nerves. The pulmonary arteries and their branches travel beside similarly sized airways, while pulmonary veins and lymphatics travel in the connective tissue septa that form the boundaries of each lung lobule. Bronchial arteries have narrower diameters and thicker walls than the pulmonary arteries, reflecting the smaller quantity of blood they carry (but under higher pressure). They also travel with airways but are inconspicuous due to their small size. Within the connective tissue surrounding larger airways are afferent and efferent nerve fibers. The external surface of the lung is covered by mesothelium, a simple squamous epithelium which normally is in contact with the mesothelial lining of the hemithoraces. The mesothelial layer that covers the entire outer surface of the lungs is called the visceral pleura, while the mesothelium that lines the hemithoraces is called the parietal pleura.
| Nasal cavity | Naso-pharynx | Larynxz | Trachea | Bronchi | Bronchioles | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Large | Small | Regular | Terminal | Respiratory | ||||||
| epithelium | pseudo-stratified ciliated columnara | transition | ||||||||
| pseudo- | simple | simple | ||||||||
| stratified → | ciliated → | ciliated | ||||||||
| ciliated | columnar | cuboidal | ||||||||
| columnar | ||||||||||
| goblet cells | abundant | present | few | scattered | none | |||||
| glands | abundant | present | few | none | ||||||
| cartilage | complex | C-shaped rings | irregular rings | plates & islands | none | |||||
| smooth muscle | none | posterior spanning open ends of C-shaped rings | crisscrossing spiral bundles | |||||||
| elastic fibers | none | present | abundant | |||||||
PRINCIPAL SECTIONS OF THE RESPIRATORY TRACT
The two nasal cavities are separated by a nasal septum composed of cartilage anteriorly and bone posteriorly. Each cavity is subdivided into three segments: the vestibule, the respiratory segment, and the olfactory segment. The vestibule is the short chamber just internal to the naris and is lined by stratified squamous epithelium. Externally, this epithelium is keratinized like skin before gradually transitioning to a nonkeratinizing form as in the oropharynx. Vestibular hairs, called vibrissae, filter large particulate matter. Within the lamina propria of the vestibule, as in the dermis, are hair follicles, eccrine glands, and sebaceous glands (Fig. 2.2).
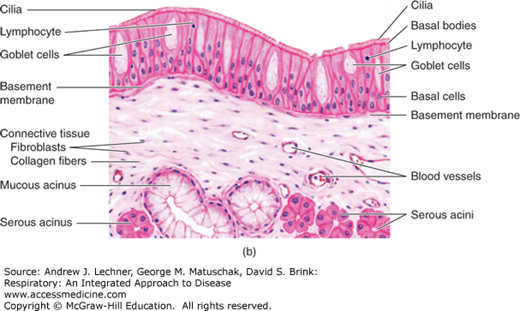
Internal to each vestibule are the respiratory segments of the nasal cavities. Although they are parts of the conducting zone and not the diffusive respiratory parenchyma, their name reflects their lining of respiratory mucosa. Respiratory mucosa is common within the respiratory system and consists of a ciliated pseudo-stratified columnar respiratory epithelium overlying layers of dense irregular connective tissue, the perichondrium of cartilage and the periosteum of bone. Deeper within the respiratory system, this connective tissue layer consists of loose irregular connective tissue characteristic of lamina propria. The staggered vertical distribution of nuclei within the respiratory epithelium suggests that it is stratified into multiple layers. However, all of its cells touch the basement membrane, and thus the epithelium is pseudo-stratified. Within it are three main types of cells: ciliated cells, goblet cells, and basal cells. Ciliated cells exhibit coordinated motility of their apical cilia to propel a sheet of mucus in retrograde direction over the surface of the epithelium, plus any particulate matter embedded within the mucus. Goblet cells are unicellular glands that produce copious quantities of mucus. Basal cells serve as progenitors that repopulate the epithelium as needed through mitosis and subsequent differentiation. Additional cell types that are less commonly noted within respiratory epithelium include brush cells, which are columnar in appearance and have apical microvilli rather than true cilia. There are also small granular neuroendocrine cells that rest upon the basement membrane (Fig. 2.3).
FIGURE 2.3
(a) Schematic of pseudo-stratified respiratory epithelium. Nuclei appear stratified, but all cells rest upon the basement membrane. From Junqueria’s Basic Histology, McGraw-Hill; 2009. (b) Respiratory epithelium as it would appear with H&E staining. From diFiore’s Atlas of Histology with Functional Correlations, 10th ed. Lippincott; 2005.
Extending from the lateral walls of the nasal cavity are three bony projections termed the superior, middle, and inferior conchae. The middle and inferior conchae are part of the vestibule and are lined by respiratory mucosa; the roof and superior concha comprise the olfactory segments of the nasal cavity. An olfactory segment consists of an olfactory epithelium overlying a lamina propria that contains Bowman glands, which are serous. The principal constituents within the olfactory epithelium are olfactory cells (or bipolar neurosensory cells). These are modified neurons with apical nonmotile cilia, which function as chemoreceptors, and basal afferent axons that join to form the olfactory nerves. In addition, the olfactory epithelium contains supporting cells, with apical microvilli that resemble the brush cells of respiratory epithelium, and regenerative basal cells, also similar to those in respiratory epithelium. Histologically, the olfactory epithelium is also termed pseudo-stratified: nuclei situated closest to the lumen belong to supporting cells; nuclei nearest the epithelium’s basement membrane are basal cells; and nuclei located between these two other nuclear layers are those of the chemoreceptive olfactory cells (Fig. 2.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree