Although degenerative aortic valve stenosis (AS) is common with increasing age, limited data exist regarding the prevalence and prognostic impact of its various valve area—gradient patterns in patients ≥80 years. To test this, echocardiograms were obtained in 542 randomly selected subjects aged ≥80 years recruited in the Belgium Cohort Study of the Very Elderly study (BFC80+). Subjects were divided into 3 groups: no or mild AS, moderate AS, and severe AS. Patients with severe AS were further stratified into those with high mean gradients (HG-AS) and those with paradoxically low mean gradients (LG-AS). Prevalence of moderate-to-severe AS was 14.7% and that of severe AS was 5.9%. In patients with severe AS, most (72%) exhibited paradoxical LG-AS. All patients with severe HG-AS were asymptomatic at the time of inclusion, whereas 48% of those with severe paradoxical LG-AS had significant symptoms. During follow-up, there were 2 aortic valve replacements and 230 deaths, of which 100 (43%) were of cardiovascular origin. Five-year overall survival rate was significantly worse in severe HG-AS than in any of the other groups (22 ± 14% vs 62 ± 2% in no or mild AS, 48 ± 7% in moderate AS, and 43 ± 10% in severe paradoxical LG-AS, p <0.01). Survival rate was similar among severe paradoxical LG-AS with and without low flow. In conclusion, in this large population-based sample of subjects ≥80 years, the prevalence of severe AS was 5.9%. Most of these subjects presented with the severe paradoxical LG-AS and a third of them were symptomatic. In this elderly community, severe HG-AS is a major determinant of prognosis, even in the absence of symptoms, whereas severe paradoxical LG-AS seems to behave similarly to moderate AS.
Several recent retrospective studies have indicated that in elderly patients, and particularly in elderly women, severe aortic stenosis (AS) is frequently associated with lower-than-expected mean transvalvular gradients, even in the presence of preserved left ventricular (LV) ejection fraction. The term severe “paradoxical low gradient (LG)”-AS was recently coined to describe this new form of severe AS and to differentiate it from the well-recognized “low flow-low gradient” form seen in patients with LV dysfunction. There is considerable debate as to the prevalence and clinical significance of severe paradoxical LG-AS. Some investigators, indeed, consider this new entity as a more advanced form of AS, with increased interstitial fibrosis, reduced LV longitudinal function, and poor prognosis, whereas others believe it represents a relatively benign form of AS, with an outcome similar to that of moderate AS. The aim of the present study was to investigate the prevalence and prognostic impact of moderate-to-severe AS, including severe paradoxical LG-AS, in the community. For this purpose, we analyzed the data of the Belgium Cohort Study of the Very Elderly study, a community-based prospective study performed in patients aged ≥80 years, at the subject’s home.
Methods
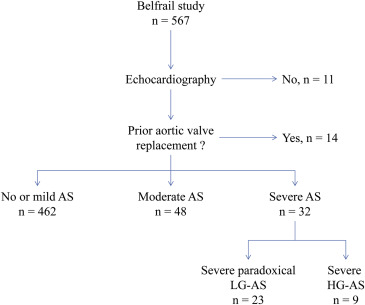
The BFC80+ study is a prospective, observational, population-based cohort study of subjects ≥80 years in 3 well-circumscribed areas of Belgium. The study design and characteristics of the cohort have been described in detail elsewhere. From November 2, 2008, to September 15, 2009, 567 subjects were included in the BFC80 + study. Of these patients, 25 subjects were excluded from the present analysis, 11 because of lack of baseline echocardiographic data and 14 because of previous aortic valve surgery. The flowchart of the study population is shown in Figure 1 . The study protocol was approved by our internal review board, and all participants gave informed consent before participating into the study.
The patients’ functional status was graded according to the New York Heart Association (NYHA) classification. Patients were considered to be in NYHA class I if they were free of any symptoms. Patients were considered to be in NYHA class II if they complained of mild symptoms (i.e., dyspnea, angina or both) during ordinary activity. Patients were considered to be in NYHA class III if they had experienced heart failure or angina during less than ordinary activity. Finally, patients were considered to be in NYHA class IV if they had experienced heart failure or angina while at rest. Patients with exercise-induced syncope were considered to be in NYHA class III. Patients who experienced transient NYHA class III or IV symptoms and did return in lower NYHA classes because of medical treatment were considered to be in either NYHA class III or IV.
Echocardiographic data were obtained at the subject’s home using a commercially available portable system (CX50; Philips, Andover, Massachusetts). All patients underwent a comprehensive examination, including M-mode and 2-dimensional echocardiography, and Doppler examinations. All tests were conducted by a single certified cardiologist with level 3 competence in echocardiography. For assessment of AS, multiple transducer positions were systematically used to record peak aortic jet velocities. Left ventricular outflow tract diameter was obtained from the parasternal long-axis view in mid-systole, parallel to the valve plane and immediately adjacent to the aortic leaflet insertion into the annulus. Left ventricular outflow tract velocity was recorded from the apical window by placing the pulse-wave Doppler sample volume in the outflow tract, proximal to the aortic valve. Proper positioning of the sample volume was ensured by verifying the presence of smooth spectral velocity curves associated with an aortic valve closing click. Care was taken to optimize the ultrasound beam-blood flow alignment and to avoid sampling in the transvalvular jet or the proximal flow convergence region by excluding velocity curves with spectral broadening at peak ejection. The maximal velocity across the aortic valve was measured with continuous-wave Doppler from multiple positions (apical, right parasternal, and subxyphoidal). The highest velocity signal was used to calculate peak and mean gradients. The aortic valve area was calculated using the continuity equation.
Severe AS was defined as an indexed aortic valve area <0.6 cm 2 /m 2 and was further stratified into subgroups with high (HG-AS) and low transvalvular gradients (LG-AS), respectively, in the presence of a mean transvalvular gradient ≥40 and <40 mm Hg. In patients with severe LG-AS, those with an LV ejection fraction >50% were considered as having severe paradoxical LG-AS. Patients with severe paradoxical LG-AS were further stratified into subgroups with low flow and normal flow, respectively, in the presence of an indexed stroke volume ≤35 or >35 ml/m 2 . Moderate AS was defined as an aortic valve area between 0.6 and 0.9 cm 2 /m 2 . Finally, mild AS was considered in the presence of an aortic valve area >0.9 cm 2 /m 2 .
LV volumes and LV ejection fraction were calculated using the biplane Simpson method, whereas LV mass was calculated according to Devereux et al. Left atrial volume was measured using the biplane area-length formula. Systolic pulmonary artery pressure was considered to be equal to the systolic transtricuspid pressure gradient as calculated using the modified Bernoulli equation. No attempt was made to estimate right atrial pressure.
Cardiac events (hospitalization, cardiac surgery, and percutaneous interventions) and causes of death were prospectively collected by the patients’ general practitioners as part of the BFC80+ study protocol. Two separate detailed follow-up questionnaires were received from the participating physicians after 1.4 ± 0.3 and 3.0 ± 0.2 years of follow-up. Mortality and cause of mortality were also recorded by the general practitioners 5.1 ± 0.25 years after inclusion. The causes of death were divided into cardiovascular and noncardiovascular, as reported in the death certificate. Follow-up was 100% complete. In addition to the follow-up questionnaires, 450 patients (81%) also underwent a second complete echocardiographic examination, 2.0 ± 0.2 years after the initial visit.
All analyses were performed using the STATA 11.0 software (StataCorp, College Station, Texas). Continuous variables were expressed as mean ± 1 standard deviation, categorical variables as counts and percentages, and follow-up times as mean and range. Continuous variables among groups were evaluated for normality and homoscedasticity and compared using a 2-way analysis of variance or the Kruskal-Wallis test when appropriate. Comparisons between groups were performed with the Bonferroni test. Categorical variables were compared using exact tests.
The impact of AS severity on survival was analyzed using the Kaplan-Meier method. Primary end point was overall mortality. Secondary end point was cardiovascular mortality. Groups were compared using a log-rank test. For each patient included in the study, the corresponding average age-specific annual mortality rates of the Belgian general population were obtained. To assess the parameters independently influencing survival in this old population, a stepwise Cox’s proportional hazard model was built to which all baseline covariates with a p value <0.05 in the univariate analysis were proposed for inclusion. To avoid collinearity, the correlation coefficients between covariates were calculated. In case of collinearity ( r value >0.90), only 1 of the 2 covariates was considered in the multivariate model. Relative hazard ratio for each specific covariate of the final models was computed as the exponential of the regression coefficient. A p value <0.05 was considered indicative of a statistically significant difference.
Results
The baseline clinical, hemodynamic, and echocardiographic characteristics of the study population are listed in Tables 1 and 2 . Moderate-to-severe AS was found in 80 of 542 patients (14.7%), of whom 32 had severe AS (5.9%) and 48 had moderate AS (9.0%). In patients with severe AS, paradoxical LG-AS was more prevalent than HG-AS (23 of 32 vs 9 of 32). Compared with patients with no or mild AS, those with severe AS were older, more frequently experienced NYHA class III-IV symptoms, more often presented with atrial fibrillation, were more likely to receive digitalis, and more frequently had a history of stroke. Thirty-one patients exhibited LV dysfunction, 30 in the no or mild AS subgroup and 1 in the moderate AS subgroup. No patient with severe LG-AS or HG-AS exhibited LV dysfunction. As listed in Table 2 , patients with severe HG-AS have lower indexed aortic valve areas and tended to have higher stroke volumes than those with severe paradoxical LG-AS.
| Mild or no AS (n=462) | Moderate AS (n=48) | Severe paradoxical LG-AS (n=23) | Severe HG-AS (n=9) | P-value | |
|---|---|---|---|---|---|
| Age (years) | 85 ± 4 | 86 ± 4 | 87 ± 5 ∗ | 87 ± 5 | 0.004 |
| Men | 170 (37%) | 13 (27%) | 14 (61%) † | 1 (11%) ‡ | 0.017 |
| Body surface area (m 2 ) | 1.73 ± 0.19 | 1.69 ± 0.19 | 1.72 ± 0.17 | 1.66 ± 0.14 | 0.82 |
| Chronic obstructive pulmonary disease | 53 (11%) | 3 (6%) | 5 (22%) | 0 (0%) | 0.18 |
| Atrial fibrillation | 52 (11%) | 5 (10%) | 9 (39%) ∗ † | 2 (22%) | 0.001 |
| Previous myocardial infarction | 52 (11%) | 4 (8%) | 3 (13%) | 0 (0%) | 0.66 |
| Previous percutaneous coronary intervention | 39 (8%) | 4 (8%) | 2 (9%) | 0 (0%) | 0.84 |
| Previous coronary bypass graft surgery | 22 (5%) | 4 (8%) | 2 (9%) | 0 (0%) | 0.53 |
| Stroke | 63 (14%) | 10 (21%) | 9 (39%) ∗ | 2 (22%) | 0.006 |
| Peripheral artery disease | 44 (10%) | 5 (10%) | 4 (17%) | 1 (11%) | 0.67 |
| Hypertension | 318 (69%) | 38 (79%) | 17 (74%) | 8 (89%) | 0.27 |
| Dyslipidemia | 205 (44%) | 18 (38%) | 10 (43%) | 2 (22%) | 0.48 |
| Diabetes | 84 (18%) | 11 (23%) | 1 (4%) | 3 (33%) | 0.17 |
| Smoking | 150 (32%) | 12 (25%) | 6 (26%) | 1 (11%) | 0.37 |
| Glomerular filtration rate (mL/min) | 65 ± 22 | 58 ± 25 | 57 ± 24 | 70 ± 19 | 0.11 |
| Brain Natriuretic Peptide (pg/ml) | 138 ± 191 | 232 ± 247 § | 254 ± 204 ∗ | 216 ± 119 | 0.001 |
| Anemia | 80 (18%) | 14 (30%) | 9 (39%) | 3 (33%) | 0.012 |
| New York Heart Association class I-II | 379 (82%) | 37 (77%) | 12 (52%) ∗ | 9 (100%) ‡ | 0.002 |
| New York Heart Association class III-IV | 83 (18%) | 11 (23%) | 11 (48%) ∗ | 0 (0%) ‡ | 0.002 |
| Angina | 67 (15%) | 12 (25%) | 6 (26%) | 1 (11%) | 0.13 |
| Diuretics | 219 (47%) | 22 (46%) | 15 (65%) | 7 (78%) | 0.11 |
| Angiotensin converting enzyme inhibitors | 125 (27%) | 14 (29%) | 4 (17%) | 3 (33%) | 0.71 |
| Beta-blockers | 192 (42%) | 23 (48%) | 11 (48%) | 3 (33%) | 0.73 |
| Aspirin or Coumadin | 241 (52%) | 29 (60%) | 13 (57%) | 4 (44%) | 0.67 |
| Statins | 149 (32%) | 11 (23%) | 9 (39%) | 0 (0%) | 0.09 |
| Digitalis | 13 (3%) | 3 (6%) | 3 (13%) | 1 (11%) | 0.031 |
| Logistic EuroScore I | 17 ± 14 | 19 ± 17 | 33 ± 19 ∗ † | 31 ± 21 ¶ | <0.001 |
∗ Mild or no AS versus severe paradoxical LG-AS.
† Moderate AS versus severe paradoxical LG-AS.
‡ Severe paradoxical LG-AS versus severe HG-AS.
§ Mild or no AS versus moderate AS.
| Mild or no AS (n=462) | Moderate AS (n=48) | Severe paradoxical LG-AS (n=23) | Severe HG-AS (n=9) | P-value | |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 146 ± 23 | 150 ± 21 | 138 ± 20 | 155 ± 20 | 0.17 |
| Diastolic blood pressure (mmHg) | 76 ± 12 | 75 ± 9 | 66 ± 11 ∗ † | 76 ± 9 | 0.002 |
| LV end-diastolic volume index (mL/m 2 ) | 76 ± 21 | 68 ± 14 | 67 ± 14 | 73 ± 10 | 0.06 |
| LV ejection fraction (%) | 55 ± 5 | 55 ± 4 | 56 ± 2 | 55 ± 3 | 0.84 |
| LV ejection fraction <50% | 30 (6.5%) | 1 (2.1%) | 0 (0%) | 0 (0%) | 0.30 |
| LV mass (g/m 2 ) | 91 ± 23 | 97 ± 22 | 96 ± 47 | 101 ± 32 | 0.22 |
| Stroke volume index (mL/m 2 ) | 40 ± 5 | 37 ± 8 | 37 ± 7 | 42 ± 11 | 0.03 |
| Pulmonary hypertension | 34 (7) | 8 (17) | 2 (9) | 3 (33) ‡ | 0.008 |
| Left atrial volume index (mL/m 2 ) | 32 ± 10 | 38 ± 11 § | 39 ± 11 ∗ | 42 ± 8 ‡ | <0.001 |
| Indexed aortic valve area (cm/m 2 ) | – | 0.74 ± 0.09 § | 0.49 ± 0.08 ∗ † | 0.36 ± 0.07 ‡ ‖ | <0.001 |
| Mean gradient (mmHg) | – | 12 ± 4 § | 23 ± 5 ∗ † | 47 ± 6 ‡ ‖ ¶ | <0.001 |
| Peak velocity (m/s) | 1.4 ± 0.3 | 2.4 ± 0.4 § | 3.0 ± 0.4 ∗ † | 4.3 ± 0.3 ‡ ‖ ¶ | <0.001 |
| Mitral regurgitation ≥2+ | 3 (0.6%) | 1 (2.1%) | 0 (0%) | 0 (0%) | 0.69 |
| Aortic regurgitation ≥2+ | 8 (1.7%) | 1 (2.1%) | 0 (0%) | 0 (0%) | 0.90 |
| Severe mitral stenosis | 1 (0.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.98 |
∗ Mild or no AS versus severe paradoxical LG-AS.
† Moderate AS versus severe paradoxical LG-AS.
‡ Mild or no AS versus severe HG-AS.
§ Mild or no AS versus moderate AS.
‖ Severe paradoxical LG-AS versus severe HG-AS.
During a mean follow-up of 5.0 ± 0.2 years, there were 2 aortic valve replacements and 230 deaths, of which 100 (43%) were of cardiovascular origin. Of the 32 patients with severe AS, 20 patients (60%) died, of which 12 (60%) died of cardiovascular causes. As shown in Figure 2 , 5-year overall survival rate was significantly worse in patients with severe HG-AS than in any other groups (22 ± 14% vs 62 ± 2% in patients with no or mild AS, 48 ± 7% in patients with moderate AS, and 43 ± 10% in severe paradoxical LG-AS, p <0.01). In patients with severe paradoxical LG-AS, survival rate was 33 ± 16% in those with and 50 ± 13% in those without low transvalvular flow (p = 0.41). Similar results were found for cardiovascular mortality ( Figure 3 ). Excluding patients with LV dysfunction, more than moderate mitral stenosis, mitral regurgitation, or aortic regurgitation did not change the results.
The results of the Cox’s proportional hazard model are listed in Table 3 . Six variables were found to be independently associated with overall survival rate: the circulating brain natriuretic peptide levels, age, the mean pressure gradient, the glomerular filtration rate, NYHA class I-II, and the presence of chronic obstructive pulmonary disease. A similar analysis was conducted for cardiovascular mortality. As listed in Table 4 , the Cox’s proportional hazard analysis identified the circulating brain natriuretic peptide levels, the mean pressure gradient, NYHA class I-II, and the presence of peripheral artery disease as being independently associated with outcome.



