Contrast-induced nephropathy (CIN) after percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI) is frequent and associated with long-term renal impairment and mortality. Early markers of CIN are needed to improve risk stratification. We aimed to assess whether N-terminal fragment of pro B-type natriuretic peptide (Nt-proBNP) could be associated with CIN. From the French regional RICO survey, all the consecutive patients who underwent primary PCI for STEMI, from January 1, 2001, to December 3, 2013, were included. Nt-proBNP circulating levels were assessed on admission. CIN was defined as an increase in serum creatinine >26.5 μmol/L or >50% within 48 to 72 hours after PCI (KDIGO criteria). Of the 1,243 patients included, CIN occurred in 130 patients (10.4%). Nt-proBNP levels were 5 times greater in patients who developed CIN than without CIN (1,275 [435 to 4,022] vs 247 [79 to 986] pg/mL, p <0.001). Hospital mortality rate was markedly higher in patients with CIN (6.9% vs 1.1%, p <0.001). Nt-proBNP levels were univariate predictors for CIN as were age, hypertension, diabetes, smoking, previous stroke, heart rate, impaired left ventricular ejection fraction C-reactive protein, history of renal failure, anemia, and estimated glomerular filtration rate <30 ml/min/1.73 m 2 at baseline. Nt-proBNP levels remained strongly associated with the occurrence of CIN even after adjustment for risk factors, treatments, clinical and biological variables (odds ratio 1.99, 95% confidence interval 1.49 to 2.66). Net reclassification improvement was achieved by the addition of Nt-proBNP to the risk model (p = 0.003). In conclusion, from this large contemporary prospective study in nonselected population, our work suggests that Nt-proBNP levels at admission could help to identify patients at risk of CIN beyond traditional risk factors.
Acute kidney injury (AKI) induced by iodinated CM or contrast-induced nephropathy (CIN) is a frequent complication in ST-segment elevation myocardial infarction (STEMI) after percutaneous coronary intervention (PCI), ranging from 10% to 20%. AKI has severe consequences including 5-fold higher hospital mortality rate and may predispose to long-term loss of kidney function. CIN is a complex disorder whose underlying mechanisms has not yet been fully elucidated. Contrast media (CM) causes vasoconstriction of renal medulla, which induces hypoxia and acute tubular necrosis, through vasoconstrictors release such as adenosine or endothelin. CM may also have a direct cytotoxic effect on tubular epithelial cells through reactive oxygen species production and decreased nitric oxide bioavailability. Risk factors for CIN include preexisting renal dysfunction, diabetes, heart failure (HF), old age, and hypotension. Volume and osmolality of CM and the emergency nature of the procedure are also risk factors. Prophylactic strategies, notably hydration, or decreasing osmolality and amount of CM have been shown to limit CIN onset. Furthermore, innovative approaches are under current consideration for preventive therapy. Therefore, efforts to risk stratify patients for CIN should be performed. Natriuretic peptides, including B-type natriuretic peptide (BNP) and the N-terminal fragment of the propeptide (Nt-proBNP), are powerful diagnostic and prognostic markers in patients with HF. In STEMI, circulating levels of Nt-proBNP are predictors for future cardiac events in the short and long term. Recent data suggest that levels of BNP could be useful to predict renal function impairment. However, only few studies have investigated this association in a large population of patients with STEMI. The aim of our study was to determine whether high levels of Nt-proBNP at admission in the acute phase of STEMI could be associated with the onset of CIN.
Methods
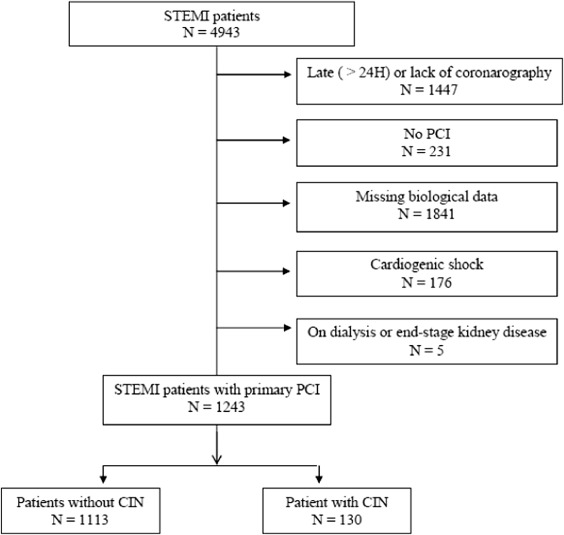
This multicenter study was carried out in patients hospitalized for STEMI from January 1, 2001, to December 3, 2013, and included in the French regional multicenter RICO survey (obseRvatoire des Infarctus de Côte d’Or). STEMI was defined according to current criteria, that is elevation of cardiac enzymes greater than upper limit of normal, associated with >1 criteria: clinical signs with nitroglycerine-resistant retrosternal chest pain lasting >20 minutes and/or electrocardiographic (ECG) modifications suggestive of myocardial infarction (MI) in ≥2 contiguous leads (persistent modification of the ST segment ≥1 mm and/or new pathologic Q wave and/or new left bundle branch block). Exclusion criteria included lack of PCI, admission >24 hours after symptoms onset, missing biologic data, or CM volume. Cardiogenic shock, glomerular filtration rate (GFR) <15 ml/min/1.73 m 2 or requiring dialysis, and death <48 hours after admission were also excluded ( Figure 1 ).
Demographic data, risk factors (hypertension; diabetes; obesity, defined by a body mass index [BMI] >30 kg/m 2 ), treated hypercholesterolemia or total cholesterol >2.5 g/L, family history of coronary artery disease (CAD, defined by premature CAD in the first-degree relative <55 years for men or 65 years for women), current smoking, cardiovascular history, and chronic treatments were collected. The following were also collected at admission: Killip class (Killip 1: no HF, Killip 2: rales <50% in lung fields, Killip 3: pulmonary edema, Killip 4: cardiogenic shock), ECG signs, MI location, and hemodynamic parameters (heart rate [HR], systolic and diastolic blood pressure [SBP and DBP, respectively]). Left ventricular ejection fraction (LVEF) was measured by echocardiography by trained investigators <12 hours after admission and dichotomized at 40% for more clinical relevance.
Patient underwent PCI <24 hours after symptoms onset. CM volume injected during the procedure was prospectively recorded. Type of contrast was chosen by each investigator according to local practice (i.e., Hexabrix hyperosmolar, or Visipaque isosmolar). The number of significant coronary lesions was also recorded. Hospital deaths were determined, and the duration of the intensive care unit stay was collected. Global Registry of Acute Coronary Events (GRACE) score was calculated for each patient ( http://www.outcomes-umassmed.org/grace/acs_risk/acs_risk_content.html ).
Blood sample was taken at admission. Plasma Nt-proBNP was measured using homogeneous chemiluminescence immunoassay on a Vista analyzer (SIEMENS). Glucose was measured using an enzymatic method (glucose oxydase) on a Vitros 750 analyzer (Johnson and Johnson Clinical Diagnostics, Rochester, New York). Glycated hemoglobin (HbA1c) was measured using an ion-exchange high-performance liquid chromatography method (Bio-Rad Laboratories, Richmond, California). C-reactive protein (CRP) levels were determined using an enzymatic method on Xpand (Dade Behring, Deerfield, Illinois). Serum creatinine level (SCL) at admission and <48 hours after PCI was measured using kinetic Jaffe method on a Vista analyzer (SIEMENS). GFR was calculated using Chronic Kidney Disease–EPIdemiology collaboration formula. Serum hemoglobin (Hb) was measured both at admission and <72 hours after admission. The lowest value <72h was recorded (low). Anemia was defined as Hb <10 g/dl.
CIN was defined according to current Kidney Disease: Improving Global outcomes (KDIGO) guidelines endorsed by European Renal Best Practice (ERBP) working group by an absolute (>26.5 μmol/l or 0.3 mg/dl) or a relative (>1.5) increase in SCL from baseline within 48 to 72 hours after injection of the CM.
This study was conducted in accordance with the declaration of Helsinki and was approved by the ethics committee of Dijon University Hospital. Each patient provided written informed consent before taking part in the study.
Results were expressed as median (twenty-fifth to seventy-fifth percentile) for continuous variables or as percentage for dichotomized variables. The normality of continuous variables was tested using the Kolmogorov–Smirnov test. For the logistic regression analysis, levels of Nt-proBNP were log transformed. For the comparison between the 2 groups, dichotomized variables were analyzed by the chi-square or Fisher’s test and continuous variables by the Student t or Mann–Whitney test, as appropriate.
Logistic regression analysis with a descending conditional model was used to identify independent factors linked to the onset of CIN. Variables associated with CIN with a threshold of 1% in univariate analysis were introduced into a multivariate model, that is age, diabetes, hypertension, current smoking, history of stroke, chronic kidney disease, LVEF <40%, anemia, CRP, HR, and GFR<30 ml/min/1.73 m 2 . Volume of CM >250 ml was also forced into the model. A threshold volume of 250 ml was chosen from a receiver operating characteristics (ROC) curve analysis. The threshold for exclusion from the model was set at 5%. The final risk model (model 1) included age, HR, anemia, and eGFR<30 ml/min/1.73 m 2 . Nt-proBNP was then added to the model 1 to provide the model 2. ROC curve analysis was performed to assess the performance of the 2 risk models and the AUC were compared. Furthermore, net reclassification improvement was calculated using tertiles of risk categories (≤10%; >10 to ≤16%; >16%).
An additional logistic regression analysis was also performed to establish the predictive value of CIN for inhospital death beyond GRACE score. SPSS manager (version 12.0, IBM Inc) was used.
Results
Of the 1,243 patients included, CIN was observed in 130 patients (10.4%). Baseline characteristics according to the development of CIN are summarized in Table 1 . Compared with patients without CIN, patients with CIN were older, with a greater proportion of diabetes, hypertension, history of stroke or CKD, but the rate of current smokers was 2-fold higher. In the CIN group, we found that a higher HR on admission, more frequent LVEF <40%, longer time to admission, and greater GRACE score. The proportion of patients on long-term treatment by insulin, angiotensin receptor blocker, angiotensin-converting enzyme inhibitor, or diuretic was also greater in patients with CIN. No difference was found for the other long-term medications including oral antidiabetics and statin.
| Contrast-Induced Nephropathy | p | ||
|---|---|---|---|
| No n=1113 | Yes n=130 | ||
| Risk factors | |||
| Female sex | 286 (26%) | 40 (31%) | 0.213 |
| Age ( years) | 64 ±14 | 72±14 | <0.001 |
| Hypertension | 487 (44%) | 79 (61%) | 0.001 |
| Obesity ∗ | 204 (18%) | 15 (12%) | 0.055 |
| Diabetes | 163 (15%) | 35 (27%) | <0.001 |
| Hypercholesterolemia | 463 (42%) | 52 (40%) | 0.726 |
| Family history of Coronary Artery Disease † | 337 (30%) | 26 (20%) | 0.015 |
| Smoking | 448 (40%) | 27 (21%) | 0.001 |
| History | |||
| Coronary Artery Disease | 123 (11%) | 18 (14%) | 0.342 |
| Stroke | 40 (4%) | 11 (8%) | 0.008 |
| Renal failure | 14 (1.3%) | 9 (6.9%) | 0.001 |
| Clinical data | |||
| Heart Rate, bpm | 75 [64-87] | 81 [70-97] | <0.001 |
| Systolic Blood Pressure ( mmHg) | 135 [120-155] | 136 [121-158] | 0.198 |
| Diastolic Blood Pressure ( mmHg) | 80 [70-94] | 82 [70-97] | 0.522 |
| N=1078 | N=124 | ||
| Left Ventricular Ejection Fraction ( %) | 50 [45-60] | 46[40-55] | <0.001 |
| Left Ventricular Ejection Fraction < 40% | 156 (14%) | 30 (24%) | 0.005 |
| Anterior wall location | 465 (42%) | 62 (48%) | 0.197 |
| Heart failure | 162 (15%) | 30 (23%) | 0.011 |
| Duration of Intensive Care Unit stay ( days) | 4±2 | 5±3 | 0.001 |
| Time symptoms-admission ( min) | 165 [95-270] | 180 [120-360] | 0.037 |
| GRACE score | 144 [124-167] | 172 [144-189] | <0.001 |
| Treatments | |||
| Angiotensin Receptor Blocker | 175 (16%) | 31 (24%) | 0.018 |
| Diuretic | 215 (19%) | 44 (34%) | <0.001 |
| Angiotensin Converting Enzyme inhibitor | 136 (12%) | 24 (18%) | 0.044 |
| Oral antidiabetic | 116 (10%) | 18 (14%) | 0.234 |
| Insulin | 39 (3.5%) | 16 (12%) | <0.001 |
| Aspirin | 138 (12%) | 20 (15%) | 0.334 |
| Beta-blocker | 212 (19%) | 28 (21%) | 0.496 |
| Statin | 226 (20%) | 24 (18%) | 0.620 |
∗ Obesity was defined as Body Mass Index >30 kg/m 2 .
† Family history was defined as premature coronary artery disease (acute coronary syndrome, coronary artery bypass graft, or percutaneous coronary intervention) in 1 st degree relatives (<55 years for men or <65 years for women).
Short-term treatments <48 hours are displayed in Table 2 . Diuretic and insulin were more often given in the CIN group. Patients in the CIN group were less likely to be given β blocker and angiotensin-converting enzyme inhibitor. However, patients in the CIN group were more likely to receive a greater volume of CM (>250 ml), though the difference was not significant. Baseline GFR and Hb lower were decreased in the CIN group ( Table 3 ). The onset of anemia (Hb <10 g/dl) <72 hours was a major risk factor of CIN.
| Contrast-Induced Nephropathy | p | ||
|---|---|---|---|
| No n=1113 | Yes n=130 | ||
| Treatments | |||
| Angiotensin Receptor Blocker | 40 (3.6%) | 2 (1.5%) | 0.306 |
| Diuretic | 166 (15%) | 46 (35%) | <0.001 |
| Angiotensin-Converting Enzyme inhibitor | 787 (71%) | 79 (61%) | 0.020 |
| Oral antidiabetic | 22 (2.0%) | 2 (1.5%) | 1.00 |
| Insulin | 245 (22%) | 41 (31%) | 0.015 |
| Aspirin | 1089 (98%) | 127 (98%) | 0.756 |
| Beta-blocker | 945 (85%) | 102 (78%) | 0.056 |
| Statin | 1032 (93%) | 117 (90%) | 0.267 |
| Revascularisation | |||
| Contrast agent volume ( mL) | 200 [160-293] | 233 [170-300] | 0.229 |
| Contrast agent Volume >250 mL | 323 (29%) | 47 (36%) | 0.092 |
| Number of significant lesions | 0.553 | ||
| 0 | 4 (0.4%) | 0 (0%) | 0.616 |
| 1 | 591 (53%) | 62 (48%) | |
| 2 | 346 (31%) | 47 (36%) | |
| 3 or Left Main | 172 (15%) | 21 (16%) | |
| Thrombolysis | 356 (32%) | 32 (27%) | 0.239 |
| Percutaneous Coronary Intervention success ∗ | 1006 (90%) | 98 (75%) | <0.001 |
| Contrast-Induced Nephropathy | p | ||
|---|---|---|---|
| No n=1113 | Yes n=130 | ||
| At admission | |||
| Glucose ( mmol/L) | 7.70 [6.54-9.60] | 7.88 [6.52-10.0] | 0.226 |
| Glycated Hemoglobin A1c ( %) | 5.8 [5.5-6.2] | 5.9 [5.6-6.6] | 0.059 |
| C-Reactive Protein, ( mg/L) | 3.7 [2.9-8.5] | 5.0 [2.9-15.9] | 0.007 |
| N Terminal fragment of Pro Brain Natriuretic Peptide ( pg/mL) | 247 [79-986] | 1275 [435-4022] | <0.001 |
| Haemoglobin ( g/100mL) | 14.1 [13.1-15.0] | 13.8 [12.4-14.9] | 0.012 |
| 0 to 72h post Percutaneous Coronary Intervention | |||
| Haemoglobin low ( g/100mL) | 12.6 [11.6-13.7] | 11.7 [9.8-12.9] | <0.001 |
| Anaemia | 84 (7%) | 33 (25%) | <0.001 |
| Renal function | |||
| At admission | |||
| Creatinine ( μmol/L) | 83 [72-98] | 90 [71-122] | 0.004 |
| Glomerular Filtration Rate ( mL/min/1.73m 2 ) | 81 [64-96] | 68 [44-88] | <0.001 |
| Glomerular Filtration Rate <30 mL/min/1.73m 2 | 21 (2%) | 16 (12%) | <0.001 |
| 48 to 72h post Percutaneous Coronary Intervention | |||
| Creatinine ( μmol/L) | 85 [74-98] | 133 [108-187] | <0.001 |
| Glomerular Filtration Rate ( mL/min/1.73m 2 ) | 80 [64-94] | 40 [25-59] | <0.001 |
| Glomerular Filtration Rate <30 mL/min/1.73m 2 | 17(1%) | 39(30%) | <0.001 |
| Δ Creatinine Percutaneous Coronary Intervention – admission ( %) | 2 [-7-11] | 37 [31-57] | <0.001 |
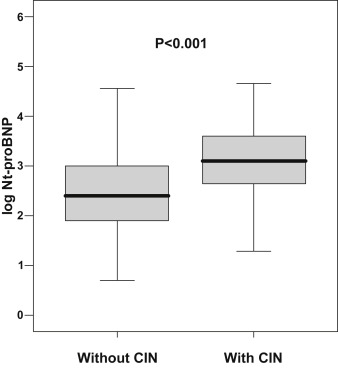
Level of Nt-proBNP was 5-fold greater in patients with CIN ( Figure 2 ). In multivariate logistic regression analysis, age, anemia, HR, and eGFR were associated with the development of CIN (model 1, Table 4 ); When added to the model, Nt-proBNP remained associated with the onset of CIN, even after adjustment for clinical and biologic variables (model 2, Table 4 ). The discriminative capacity of the risk model, as assessed by AUC, was significantly improved by the addition of Nt-proBNP ( Table 4 ). Moreover, the addition of Nt-proBNP to the risk prediction model (model 2 vs model 1) provided significant NRI (0.155, p = 0.003) further confirming the incremental value of Nt-proBNP to predict CIN onset. Short-term treatments such as diuretic or insulin are more frequent in patients with CIN and need therefore to be considered as factors potentially associated with CIN onset. However, when added to the multivariate logistic regression model, insulin failed to remained independently associated with CIN onset (p = 0.405). Diuretic treatment had a strong interaction with Nt-proBNP for the risk assessment of CIN (p <0.001) and therefore was not introduced in the multivariate model to avoid multicollinearity. In addition, when diuretic treatment was introduced in the model as a forced variable, Nt-proBNP remained a strong estimates of CIN (p <0.001). As age was a major factor associated with CIN, in addition to Nt-proBNP level, we searched a potential interaction of age with Nt-proBNP to predict CIN. We found a significant interaction (p <0.001) and then identified an optimal discrimination threshold at 70 years by ROC analysis. Stratified analysis was then performed in patients according to age (<70 years or ≥70 years), using the variables entered in the model 2 ( Table 5 ). Strikingly, risk for CIN associated with Nt-proBNP level was much more pronounced in younger (i.e., <70 years; almost twice greater) compared with older (≥70 years) patients. In contrast, in older patients, baseline renal dysfunction (i.e., GFR <30 ml/min/1.73 m 2 ) was the major determinant for CIN. ROC analysis in this young population showed that the threshold of Nt-proBNP for the prediction of CIN was 204 pg/ml, yielding sensitivity at 80% and specificity at 59%. These findings strongly suggest the specific interest of this biomarker for CIN risk in younger patients.