Preparation for Cardiopulmonary Bypass
Exposure of the Heart
Technique
The remnant of the thymus gland is dissected free from the pericardium. The thymic vessels are all electrocoagulated to prevent the formation of a hematoma or troublesome oozing during the operation. The larger ones should be occluded with metal clips. The pleura is peeled away from the inferior pericardium with a dry sponge, thereby preventing inadvertent entry into the pleural cavities. The electrocautery blade can be used to incise the pericardium and at the same time coagulate the edges. This maneuver may trigger ventricular fibrillation if the cautery blade touches the heart. It is therefore preferable to incise the pericardium with a pair of scissors or a scalpel. The pericardium can then be opened in the usual inverted T fashion and suspended to skin edges or towels (Fig. 2-1).
The sternal retractor should be opened gradually without traumatizing the sternal edges. It can be positioned in such a manner that its cross-arm is in the upper part of the wound. This technique helps to prevent entanglement or overcrowding of various pump lines. The blades of the retractor should be placed as low as possible, and the sternum should be opened only to the extent that is essential for adequate exposure. This prevents possible fracture of the first rib and brachial plexus injury (see Fig. 1-2). Many surgeons prefer sternal retractors with three to four blades which can swivel horizontally and thereby lessen the pressure on the sternal edges.
Dissection Around the Aorta
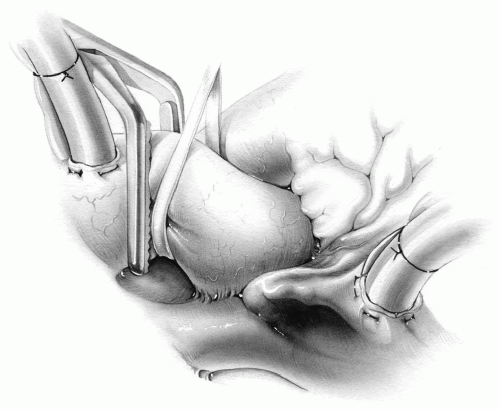
The posterior aspect of the aorta is not always free, and therefore the cross-clamp may not include the entire wall of the aorta (Fig. 2-2). Often it helps to mobilize the aorta to ensure its complete cross-clamping. In primary cardiac surgeries, the area between the pulmonary artery and aorta is dissected in a limited manner to allow a large curved or right-angled clamp to be passed behind the aorta. In redo surgeries, some sharp dissection behind the aorta must be carried out as well. When a clear passage is created, the clamp is used to pass an umbilical tape around the aorta. Traction on the tape allows the aorta to be lifted out of its bed (Fig. 2-3).
 Adventitial tissue on arteries and veins is an integral component of the vascular walls. It should not be dissected free but kept intact whenever possible.
Adventitial tissue on arteries and veins is an integral component of the vascular walls. It should not be dissected free but kept intact whenever possible.Incorporation of adequate adventitial tissue in closure of the aortotomy or various cannulation sites including the superior vena cava and pulmonary artery is a safe and effective technique. The adventitial component is a natural tissue that acts like a reinforcing pledget, adding strength to the closure.
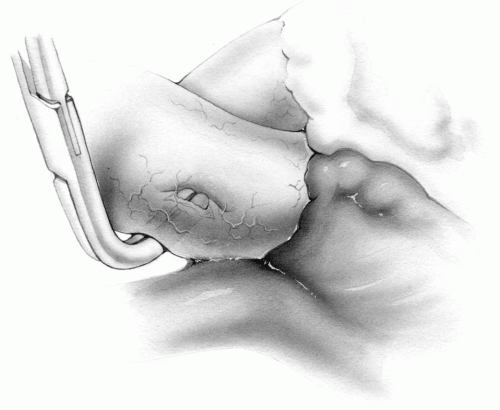
During dissection and passing of the clamp behind the aorta, care must be taken to avoid injury to the posterior wall (Fig. 2-4). If such a complication occurs, it is best to control the bleeding digitally or by packing the area while preparations are made to initiate cardiopulmonary bypass (Fig. 2-5). With the patient on bypass and the aorta cross-clamped, the aorta is opened and the posterior wall is repaired under direct vision (Fig. 2-6).
On rare occasions when the right pulmonary artery takes a more caudal course, it may be injured during dissection around the aorta. If such a problem arises, it is best to control the bleeding by packing the area and to correct the lesion when the heart is decompressed on full cardiopulmonary bypass. The right pulmonary artery can also be injured during dissection of the superior vena cava, especially when passing a tape around this vessel (Fig. 2-7).
Dissection Around the Cavae
Dissection required to pass umbilical tapes around the venae cavae in preparation for total cardiopulmonary bypass may be tedious and occasionally may result in
injury to the great veins. The parietal pericardium is divided on each side of the vena cava, and a plane is established that allows an appropriate curved clamp to be passed around the cava with ease. The umbilical tapes are then introduced around each vessel with a curved clamp.
injury to the great veins. The parietal pericardium is divided on each side of the vena cava, and a plane is established that allows an appropriate curved clamp to be passed around the cava with ease. The umbilical tapes are then introduced around each vessel with a curved clamp.
Dissection around the venae cavae can be cumbersome, particularly if extensive adhesions from previous surgery are present. The right phrenic nerve coursing along the lateral aspect of the cavae and the right atrium on the pleural aspect of the pericardium can easily be injured, either by sharp dissection or injudicious use of cautery. This results in paralysis of the right hemidiaphragm and complicates the ventilatory care of the patient in the postoperative period. The surgeon should therefore attempt to avoid the right phrenic nerve at all costs.
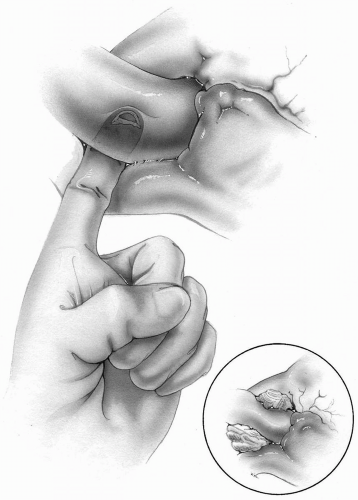
Caval injury is initially controlled digitally. Cardiopulmonary bypass is established, cannulating the aorta and either the inferior vena cava or right atrial appendage, and the problem is managed under direct vision. The site of the tear is brought into view by
gently retracting the great vein with an atraumatic tissue forceps, at which time it can be sutured with fine Prolene. On rare occasions when the torn caval wall is very friable, the suturing may incorporate an adjacent segment of the intact pericardial wall for buttressing and therefore hemostasis. Tension on the suture line is relieved by a curvilinear incision of the pericardium (Fig. 2-8).
gently retracting the great vein with an atraumatic tissue forceps, at which time it can be sutured with fine Prolene. On rare occasions when the torn caval wall is very friable, the suturing may incorporate an adjacent segment of the intact pericardial wall for buttressing and therefore hemostasis. Tension on the suture line is relieved by a curvilinear incision of the pericardium (Fig. 2-8).
Arterial Cannulation
Aortic Cannulation
Technique
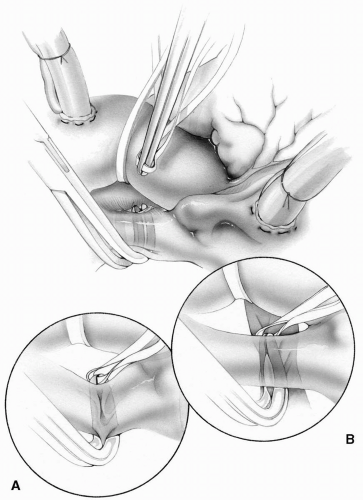
Except in a few specific instances, the aorta is directly cannulated for arterial perfusion during cardiopulmonary bypass. Small bites of the adventitia and media as high up on the aorta as feasible are taken with 3-0 Prolene sutures on noncutting needles to form a single or double purse-string. A stab wound is made within the purse-string sutures. The tip of the aortic cannula is then introduced atraumatically into the opening (Fig. 2-9). The sutures can be buttressed with felt or pericardial pledgets to prevent bleeding from the needle holes. The ends of the purse-string sutures, which have passed through a long, narrow rubber or plastic tube, are secured. The tubing is then tied to the aortic cannula and, if desired, further secured to the edges of the wound (Fig. 2-10). The aortic cannula is allowed to fill retrogradely with blood. It is then connected to the arterial line, making sure that all air has been removed from the circuit.
 In patients undergoing reoperation with scarred aortic walls or pediatric patients, it may be useful to insert an appropriately sized Hegar dilator through the stab wound before inserting the aortic cannula.
In patients undergoing reoperation with scarred aortic walls or pediatric patients, it may be useful to insert an appropriately sized Hegar dilator through the stab wound before inserting the aortic cannula.Although this technique of aortic cannulation is a generally safe approach, serious vascular complications may nevertheless occur. The aorta should be routinely palpated for localized thickening and calcific plaques. Transesophageal echocardiography and epiaortic ultrasonographic scan of the ascending aorta are more sensitive for confirmation and localization of atheromatous changes. The site for cannulation should be disease-free if possible. Usually, the anterior aspect of the aorta just proximal to the base of the innominate artery or the segment along the inner curvature of the aorta adjacent to the pulmonary artery is relatively free of calcification.
 Epiaortic scanning should be performed before the placement of the purse-string sutures. The transducer is passed into a sterile plastic bag, with the tip coated with lubricating jelly to enhance image quality. The pericardial cavity is filled with warm saline and the aortic arch and ascending aorta are scanned.
Epiaortic scanning should be performed before the placement of the purse-string sutures. The transducer is passed into a sterile plastic bag, with the tip coated with lubricating jelly to enhance image quality. The pericardial cavity is filled with warm saline and the aortic arch and ascending aorta are scanned.Porcelain, lead pipe, or eggshell aorta is the term used when the entire ascending aorta is calcified. Cannulation or clamping of this kind of aorta has catastrophic complications, namely, strokes and uncontrollable hemorrhage. In such cases, the femoral or axillary artery and right atrium are cannulated and the aorta is replaced or dealt with under deep hypothermic circulatory arrest (see Management of Porcelain Aorta in Chapter 5).
Partial occluding clamps should be avoided, especially when the aortic pressure is high, unless they are needed to control brisk hemorrhage or other complications. A clamp can crush the diseased wall and give rise to a tear of the intima, resulting in dissection of the aortic wall or disruption with massive bleeding.
Whenever the aortic wall is thin or friable, the pursestring sutures are reinforced with Teflon or pericardial pledgets on each side of the cannula to prevent any injury to the aortic wall or bleeding from the needle sites (Fig. 2-10).
Aggressive introduction of too large an aortic cannula through a small aortic opening can tear the aortic wall, dislodge calcific plaques, and cause separation of the intima and dissection around the cannulation site (Fig. 2-11). An expanding adventitial hematoma may be the first sign of traumatic aortic dissection. The cannula must be removed immediately and the cannulation site excluded carefully with a side-biting clamp (which in itself may further the dissection) to prevent progression of the dissection. On these occasions, retrograde perfusion through the femoral artery should be established promptly and the aortic injury dealt with under controlled conditions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree