The Synergy Between PCI With TAXUS and Cardiac Surgery (SYNTAX) score is effective in predicting clinical outcome after percutaneous coronary intervention (PCI). However, its prediction ability is low because it reflects only the coronary characterization. We assessed the predictive value of combining the ankle-brachial index (ABI) and SYNTAX score to predict clinical outcomes after PCI. The ABI-SYNTAX score was calculated for 1,197 patients recruited from the Shinshu Prospctive Multi-center Analysis for Elderly Patients with Coronary Artery Disease Undergoing Percutaneous Coronary Intervention (SHINANO) registry, a prospective, observational, multicenter cohort study in Japan. The primary end points were major adverse cardiovascular and cerebrovascular events (MACE; all-cause death, myocardial infarction, and stroke) in the first year after PCI. The ABI-SYNTAX score was calculated by categorizing and summing up the ABI and SYNTAX scores. ABI ≤0.49 was defined as 4, 0.5 to 0.69 as 3, 0.7 to 0.89 as 2, 0.9 to 1.09 as 1, and 1.1 to 1.5 as 0; an SYNTAX score ≤22 was defined as 0, 23 to 32 as 1, and ≥33 as 2. Patients were divided into low (0), moderate (1 to 2), and high (3 to 6) groups. The MACE rate was significantly higher in the high ABI-SYNTAX score group than in the lower 2 groups (low: 4.6% vs moderate: 7.0% vs high: 13.9%, p = 0.002). Multivariate regression analysis found that ABI-SYNTAX score independently predicted MACE (hazards ratio 1.25, 95% confidence interval 1.02 to 1.52, p = 0.029). The respective C-statistic for the ABI-SYNTAX and SYNTAX score for 1-year MACE was 0.60 and 0.55, respectively. In conclusion, combining the ABI and SYNTAX scores improved the prediction of 1-year adverse ischemic events compared with the SYNTAX score alone.
The Synergy Between PCI With TAXUS and Cardiac Surgery (SYNTAX) score is a coronary lesion complexity scoring system that is used as a prognostic tool in the short- and long-term risk stratification of patients who undergo percutaneous coronary intervention (PCI). The SYNTAX score reflects only the coronary characterization, so its ability to predict the prognosis of patients who underwent PCI is lower than that of other scoring systems, including the patient’s clinical characteristics. However, these scoring systems need numerous clinical variables and are slightly complex to calculate. In contrast, the ankle-brachial index (ABI) is not only a tool for diagnosing peripheral artery disease but also an indicator of systemic atherosclerosis in vessels such as the coronary, carotid, and cerebrovascular arteries. We hypothesized that simply combining the ABI and SYNTAX scores would improve the prediction of the prognosis of patients who underwent PCI compared with the SYNTAX score alone.
Methods
The Shinshu Prospctive Multi-center Analysis for Elderly Patients with Coronary Artery Disease Undergoing Percutaneous Coronary Intervention (SHINANO) registry has been published previously. Briefly, the registry was a multicenter, prospective, observational registry designed to compare the differences in baseline characteristics and short- and long-term outcomes after initial PCI between elderly and nonelderly patients. From August 2012 to July 2013, a total of 1,923 consecutive patients with any coronary artery disease (stable angina, ST-segment elevation myocardial infarction, non–ST-segment elevation myocardial infarction, and unstable angina) were enrolled from 16 institutions in Nagano prefecture, Japan. This registry had no exclusion criteria. For the current subanalysis, patients with a missing ABI, missing SYNTAX score, ABI >1.5, or previous coronary artery bypass grafting were excluded. This registry was approved by the ethics committee of each hospital and performed in accordance with the Declaration of Helsinki. Informed consent was obtained from each participant. The SHINANO registry was registered with the University Hospital Medical Information Network Clinical Trials Registry, as accepted by the International Committee of Medical Journal Editors (No. UMIN000010070).
The ABI-SYNTAX score was calculated by first reclassifying the ABI and SYNTAX scores and then adding them. ABI ≤0.49 was classified as 4, 0.5 to 0.69 as 3, 0.7 to 0.89 as 2, 0.9 to 1.09 as 1, and 1.1 to 1.5 as 0 points; and SYNTAX score ≤22 was classified as 0, 23 to 32 as 1, and ≥33 as 2 points according to the results of Cox multivariate analysis of each variables. The resulting scores were added. Patients were classified into 3 groups: ABI-SYNTAX score low (0), ABI-SYNTAX score moderate (1 to 2), and ABI-SYNTAX score high (3 to 6). Blood pressure measurements and ABI calculations were performed according to the recommendations of the American Heart Association. The ABI was calculated separately for each leg, and the lower value was used for analyses. Patients with ABI >1.5 were excluded, as in other studies. The SYNTAX score for each patient was calculated by scoring all coronary lesions with a stenosis diameter ≥50% in vessels ≥1.5 mm, using the SYNTAX score algorithm, which is described in full elsewhere.
The primary end points were major adverse cardiac and cerebrovascular events (MACE), defined as a composite of all-cause death, myocardial infarction, and stroke. The secondary end points were all-cause death, cardiac death, myocardial infarction, stroke, and target lesion revascularization.
Definitions were previously reported by the SHINANO registry. All-cause death was defined as mortality from any cause. Cardiac death was defined as any death due to an immediate cardiac cause, deaths related to the PCI procedure, including those related to concomitant treatment, unwitnessed death, and death of unknown cause. Target lesion revascularization was defined as a repeat revascularization driven by ischemia because of a stenosis within the stent or within a 5-mm border proximal or distal to the stent. Left ventricular ejection fraction (LVEF) was measured using echocardiography, and LVEF ≤55% indicated left ventricular dysfunction.
Continuous variables are reported as the mean ± SD and were compared using one-way analysis of variance. Categorical variables are reported as frequencies (percentages) and were compared with the Pearson’s chi-square test. Survival curves were constructed for time-to-event variables with Kaplan-Meier estimates and compared using the log-rank test. Cox regression analysis was used to find independent predictors of MACE. Receiver operator characteristic curves were used to compare the performance and predictive accuracy of the ABI-SYNTAX score and SYNTAX score. A p value <0.05 was considered statistically significant in all analyses. Data were analyzed with SPSS 21 (IBM, Armonk, New York).
Results
Of the 1,923 patients who were recruited in the SHINANO registry, 662 were excluded and 64 were lost to follow-up. Finally, 1,197 (94.9%, mean follow-up 354 ± 54.9 days) completed the 1-year follow-up ( Figure 1 ).

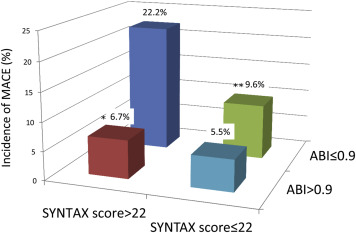
The SYNTAX score ranged from 1 to 57.5, with a mean ± SD of 12.3 ± 8.6 and a median of 10 (interquartile range [IQR] 11). The lower ABI ranged from 0.03 to 1.4, with a mean ± SD of 1.04 ± 0.17 and a median of 1.08 (IQR 0.16). The ABI-SYNTAX score had a mean ± SD of 0.91 ± 1.00 and a median of 1 (IQR 1). Figure 2 shows the incidence of MACE by ABI and SYNTAX score categories. The MACE rate in the group with an SYNTAX score >22 and ABI ≤0.9 was significantly higher than that in the other groups (p = 0.02). In the high SYNTAX score group, the patients with ABI ≤0.9 had a significantly higher rate of MACE than did those with ABI >0.9. The 1,197 patients were divided into 3 groups according to their ABI-SYNTAX score: ABI-SYNTAX score low (0; n = 479), moderate (1 to 2; n = 617), and high (3 to 6; n = 101).
Baseline clinical and angiographic characteristics of the study population according to ABI-SYNTAX score tertiles are listed in Tables 1 and 2 . Patient age, presence of diabetes mellitus, hemodialysis, previous heart failure, and peripheral artery disease were significantly higher in the ABI-SYNTAX score high group, whereas the estimated glomerular filtration rate and LVEF were significantly lower in this group. For the angiographic findings, multivessel disease, calcified lesions, ostial lesions, SYNTAX score, number of stents implanted, and total stent length were significantly higher in the ABI-SYNTAX score high group.
| Variable | Overall (n = 1197) | ABI-SYNTAX score | P value | ||
|---|---|---|---|---|---|
| Low (n = 479) | Moderate (n = 617) | High (n = 101) | |||
| Age (years) | 70.3 ± 11.0 | 67.6 ± 10.7 | 71.4 ± 10.9 | 76.3 ± 9.0 | <0.001 |
| Men | 933 (77.9%) | 401 (83.7%) | 457 (74.1%) | 75 (74.3%) | <0.001 |
| Body mass index (kg/m 2 ) | 24.0 ± 7.2 | 24.2 ± 3.5 | 24.0 ± 9.4 | 22.5 ± 3.6 | 0.083 |
| Hypertension | 876 (73.2%) | 352 (73.5%) | 447 (72.4%) | 77 (76.2%) | 0.714 |
| Dyslipidemia | 717 (59.9%) | 282 (58.9%) | 373 (60.4%) | 62 (61.4%) | 0.847 |
| Diabetes mellitus | 422 (35.3%) | 147 (30.7%) | 227 (36.8%) | 48 (47.5%) | 0.003 |
| Current smoker | 233 (18.6%) | 92 (19.2%) | 118 (19.1%) | 23 (22.8)% | 0.711 |
| Previous smoker | 628 (52.5%) | 253 (52.8%) | 322 (52.2%) | 53 (52.5%) | 0.891 |
| Estimated glomerular filtration rate (mL/min/1.73m 2 ) | 62.1 ± 23.5 | 64.7 ± 22.3 | 60.6 ± 23.8 | 58.8 ± 26.0 | 0.006 |
| Hemodialysis | 67 (5.6%) | 22 (4.6%) | 34 (5.5%) | 11 (10.9%) | 0.043 |
| Previous myocardial infarction | 252 (21.1%) | 89 (18.6%) | 135 (21.9%) | 28 (27.8%) | 0.094 |
| Previous heart failure | 146 (12.2%) | 39 (8.1%) | 83 (13.5%) | 24 (23.8%) | <0.001 |
| Previous stroke | 107 (8.9%) | 37 (7.7%) | 58 (9.4%) | 12 (11.9%) | 0.349 |
| Previous intracranial bleeding | 16 (1.3%) | 5 (1.0%) | 10 (1.6%) | 1 (1.0%) | 0.677 |
| Peripheral artery disease | 138 (11.5%) | 10 (2.1%) | 68 (11.0%) | 60 (59.4%) | <0.001 |
| Atrial fibrillation | 130 (10.9%) | 34 (7.1%) | 83 (13.5%) | 13 (12.9%) | 0.003 |
| Left ventricular ejection fraction (%) | 61.5 ± 12.4 | 63.7 ± 11.6 | 60.5 ± 12.5 | 57.2 ± 14.1 | <0.001 |
| Left ventricular dysfunction | 294 (24.6%) | 88 (18.4%) | 169 (27.4%) | 37 (36.6%) | <0.001 |
| Medication | |||||
| Aspirin | 1165 (97.3%) | 472 (98.5%) | 596 (96.6%) | 97 (96.0%) | 0.099 |
| Thienopyridines | 1089 (91.0%) | 439 (91.6%) | 561 (91.0%) | 89 (88.1%) | 0.773 |
| Angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker | 849 (70.9%) | 326 (68.1%) | 451(73.1%) | 72 (71.3%) | 0.19 |
| β-blocker | 490 (40.9%) | 185 (38.6%) | 262 (42.5%) | 43 (42.6%) | 0.382 |
| Statins | 857 (71.6%) | 344 (71.8%) | 442 (71.6%) | 71 (70.3%) | 0.997 |
| Warfarin | 115 (9.6%) | 35 (7.3%) | 65 (10.5%) | 15 (14.9%) | 0.031 |
| Novel oral anticoagulants | 17 (1.4%) | 6 (1.3%) | 11 (1.8%) | 0 (0%) | 0.349 |
| Variable | Overall (n = 1197) | ABI-SYNTAX score | P value | ||
|---|---|---|---|---|---|
| Low (n = 479) | Moderate (n = 617) | High (n = 101) | |||
| Acute coronary syndrome | 517 (43.2%) | 198 (41.3%) | 280 (45.4%) | 39 (38.6%) | 0.254 |
| Multivessel disease | 433 (36.2%) | 124 (25.9%) | 248 (40.2%) | 61 (60.4%) | <0.001 |
| De novo | 1082 (90.4%) | 431 (90.0%) | 561 (90.9%) | 90 (89.1%) | 0.688 |
| Drug eluting stent in-stent restenosis | 46 (3.8%) | 18 (3.8%) | 22 (3.6%) | 6 (5.9%) | 0.516 |
| Bare metal stent in-stent restenosis | 80 (6.7%) | 32 (6.7%) | 40 (6.5%) | 8 (7.9%) | 0.87 |
| Left main trunk lesions | 16 (1.3%) | 3 (0.6%) | 10 (1.6%) | 3 (3.0%) | 0.119 |
| Calcified lesions | 335 (28.0%) | 116 (24.2%) | 173 (28.0%) | 46 (45.5%) | <0.001 |
| Ostial lesions | 82 (6.9%) | 34 (7.1%) | 33 (5.3%) | 15 (14.9%) | 0.002 |
| Bifurcation lesions | 295 (24.6%) | 117 (24.4%) | 152 (24.6%) | 26 (25.7%) | 0.967 |
| Chronic total occlusion lesions | 71 (5.9%) | 24 (5.0%) | 37 (6.0%) | 10 (9.9%) | 0.17 |
| American Heart Association classification | |||||
| Type B2 | 223 (18.6%) | 88 (18.4%) | 108 (17.5%) | 27 (26.7%) | 0.086 |
| Type C | 546 (45.6%) | 207 (43.2%) | 293 (47.5%) | 46 (45.5%) | 0.371 |
| SYNTAX score | 12.3 ± 8.6 | 9.8 ± 5.5 | 12.8 ± 8.4 | 21.1 ± 14.0 | <0.001 |
| Bare metal stent | 439 (36.7%) | 174 (36.3%) | 235 (38.1%) | 30 (29.7%) | 0.263 |
| Drug eluting stent in-stent restenosis | 599 (50.0%) | 242 (50.5%) | 306 (49.6%) | 51 (50.5%) | 0.95 |
| Plain old balloon angioplasty alone | 159 (13.3%) | 63 (13.2%) | 76 (12.3%) | 20 (19.8%) | 0.12 |
| Number of stents implanted | 1.1 ± 0.7 | 1.0 ± 0.6 | 1.2 ± 0.7 | 1.2 ± 1.0 | 0.008 |
| Total stent length (mm) | 26.1 ± 14.5 | 24.6 ± 12.2 | 26.6 ± 14.8 | 31.0 ± 20.6 | 0.001 |
| Maximum dilatation pressure (atm) | 13.7 ± 3.6 | 13.8 ± 3.5 | 13.6 ± 3.6 | 13.5 ± 3.8 | 0.255 |
Table 3 lists outcomes at 1 year, and Figure 3 lists the incidence of MACE, all-cause death, cardiac death, myocardial infarction, and target lesion revascularization according to the ABI-SYNTAX tertiles during the 1-year follow-up. The incidence of MACE was 6.5% overall. MACE, all-cause death, and stroke were significantly higher in the ABI-SYNTAX score high group. However, there were no significant differences in the incidence of cardiac death, myocardial infarction, and target lesion revascularization across groups. Other causes of death, aside from cardiac causes, were hemorrhage (n = 4), pneumonia (n = 6), cancer (n = 4), and others (n = 13).
| Variable | Overall (n = 1197) | ABI-SYNTAX score | P value | ||
|---|---|---|---|---|---|
| Low (n = 479) | Moderate (n = 617) | High (n = 101) | |||
| Major adverse cardiac and cerebrovascular event | 78 (6.5%) | 21 (4.4%) | 43 (7.0%) | 14 (13.9%) | 0.002 |
| Death | 40 (3.3%) | 7 (1.5%) | 24 (3.9%) | 9 (8.9%) | <0.001 |
| Cardiac death | 12 (1.0%) | 2 (0.4%) | 8 (1.3%) | 2 (2.0%) | 0.206 |
| Myocardial infarction | 25 (2.1%) | 10 (2.1%) | 13 (2.1%) | 2 (2.0%) | 0.997 |
| Q-wave myocardial infarction | 8 (0.7%) | 3 (0.6%) | 5 (0.8%) | 0 (0%) | 0.644 |
| Non Q-wave myocardial infarction | 17 (1.4%) | 7 (1.5%) | 8 (1.3%) | 2 (2.0%) | 0.861 |
| Stroke | 17 (1.4%) | 4 (0.8%) | 8 (1.3%) | 5 (5.0%) | 0.006 |
| Target lesion revascularization | 88 (7.4%) | 31 (6.5%) | 53 (8.6%) | 4 (4.0%) | 0.162 |
The results of the Cox univariate and multivariate analyses are listed in Table 4 . The multivariate analysis found that age, left ventricular dysfunction, and ABI-SYNTAX score were independent predictors of MACE. However, ABI score and SYNTAX score individually were not independent predictors of MACE.



