The American College of Cardiology/American Heart Association recently updated recommendations for percutaneous coronary intervention (PCI) of unprotected left main coronary artery (ULMCA) disease from class III to II(b) according to the results of the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) trial. The SYNTAX score is an angiographic tool using solely the coronary anatomy. We studied the effect of co-morbidities (Parsonnet’s score) on the ability of the SYNTAX score to predict long-term outcomes in patients with ULMCA disease treated by revascularization. A total of 328 patients underwent revascularization of ULMCA from April 2003 to February 2007. Of the 328 patients, 120 underwent PCI (median follow-up 973 days) and 208 underwent coronary artery bypass grafting (CABG) (median follow-up 1,298 days). The ability of the SYNTAX score to predict outcomes was assessed using the Cox proportional hazards model. The outcomes between the PCI and CABG groups were compared by propensity analysis. The median SYNTAX score was 26 in the PCI and 28 in the CABG group (p = 0.5). In the PCI group, greater quartiles were associated with worse survival (62.1% at SYNTAX score of ≥36 vs 82.4% at SYNTAX score of <36, p = 0.03) and all-cause mortality, myocardial infarction, cerebrovascular events, and target vessel revascularization-free (MACCE) survival (47.7%, SYNTAX score ≥20 vs 76.6%, SYNTAX score <20, p = 0.02). Using the Parsonnet score as a covariate, the SYNTAX score continued to be an independent predictor of MACCE and demonstrated a trend toward predicting mortality in the PCI group. In contrast, the SYNTAX score did not predict the outcomes for the CABG group. No difference was found in mortality between the PCI and CABG groups for ULMCA disease, regardless of coronary complexity; although greater SYNTAX scores were associated with increased MACCE rates with PCI compared to CABG. Both the coronary anatomy (SYNTAX score) and co-morbidities (Parsonnet’s score) predicted long-term outcomes for PCI of ULMCA disease. In contrast, the SYNTAX score did not predict the outcomes after CABG. In conclusion, the ideal scoring system to guide an appropriate revascularization decision for ULMCA disease should take into account both the coronary anatomy and the co-morbidities.
The “SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery” (SYNTAX) score is an angiographic tool used to characterize the complexity of coronary artery disease using solely angiographic criteria. This is in contrast to surgical scoring systems such as the Parsonnet score and Euroscore, which use clinical factors important in risk stratification. The SYNTAX score has been believed to be of particular value in evaluating patients with unprotected left main coronary artery (ULMCA) disease, which is characterized by a number of anatomic complexities believed relevant to the choice between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Recently, the SYNTAX score has been shown to be of prognostic value in predicting the outcomes after ULMCA revascularization. However, a potentially important limitation of the SYNTAX score as a tool for decision-making between PCI and CABG is that it does not account for the clinical co-morbidities. The accuracy of the SYNTAX score for predicting outcomes after left main PCI improves with the inclusion of clinical variables in the scoring model. Thus, the aim of our study was to determine the outcomes between PCI and CABG for ULMCA disease using the SYNTAX score and to determine the effect of clinical co-morbidities on the predictive accuracy of the SYNTAX score in patients with ULMCA disease undergoing revascularization at our center.
Methods
A total of 343 patients who underwent revascularization for ULMCA stenosis from April 2003 to February 2007 were included in the present study. ULMCA stenosis was defined as left main stenosis >50%, relative to a reference segment of the left main coronary artery. The patients were excluded from the study if they had undergone concomitant valve replacement surgery, they had undergone bare metal stent implantation in the left main coronary artery, or diagnostic angiograms were not available in the database. The patients with ULMCA disease underwent revascularization with CABG or PCI according to a physician–patient consensus determined by the cardiac operative risk and patient preference. The institutional review board of Cedars-Sinai Medical Center, Los Angeles, approved the present study.
SYNTAX scores were calculated for all patients, as described by Sianos et al, using dedicated software (available at www.syntaxscore.com/calc/start.htm ). All angiograms were analyzed independently by 2 experienced interventional cardiologists who were unaware of the treatment groups. The Parsonnet scores were calculated, as described previously, for all patients, to assess the cardiac operative risk according to the presence of systemic co-morbidities.
The primary end point was all-cause mortality during follow-up after ULMCA revascularization. The secondary end point was a composite of all-cause mortality, myocardial infarction, cerebrovascular events, and target vessel revascularization (MACCE). Mortality was defined as death from any cause, cardiac and noncardiac. Myocardial infarction was defined as cardiac enzymes ≥3 times the upper limit of normal and associated with the presence of ischemic symptoms or new electrocardiographic changes. Periprocedural myocardial infarction was defined as cardiac enzymes ≥3 times the upper limit of normal after PCI and ≥5 times the upper limit of normal after CABG. A cerebrovascular event was defined as stroke, transient ischemic attack, or coma. Target vessel revascularization was defined as repeat revascularization of the left main coronary artery, including any segments of the left anterior descending artery and the left circumflex artery.
The patients in the PCI and CABG groups were divided into 4 quartiles each, according to the distribution of the SYNTAX scores. Survival and MACCE-free survival were compared across the SYNTAX score quartiles. We then compared the outcomes between the PCI and CABG groups according to the SYNTAX score. As described previously, a propensity score model using 18 variables was developed by multivariate logistic regression analysis to estimate the probability of a patient in the present study to undergo CABG. This was done to account for the differences in the baseline characteristics between the PCI and CABG groups. The patients were divided into 3 groups according to the extent of coronary artery disease: SYNTAX score <13 (isolated left main disease involving the ostial/midshaft/distal left main artery without left anterior descending artery/left circumflex artery involvement), SYNTAX score 13 to 25 (complex left main disease—left main bifurcation disease involving left anterior descending artery/left circumflex artery involvement or distal left main with proximal left anterior descending artery/left circumflex artery involvement), and SYNTAX score >25 (extensive coronary artery disease involving multiple complex lesions and left main disease). The propensity score was used as a covariate in the Cox proportional hazards models to compare the outcomes between the PCI and CABG groups according to the extent of coronary artery disease in the SYNTAX score subgroups.
Continuous variables are presented as the mean ± SD, and discrete categorical variables as the percentage (frequency), unless specified otherwise. Categorical variables were compared using the chi-square or Fisher exact test, as appropriate. Continuous variables were compared using analysis of variance or the Kruskal-Wallis test, as appropriate. Overall survival and MACCE-free survival were estimated using the Kaplan-Meier method and compared using the log-rank test. Hazard ratios (HRs) and 95% confidence intervals (CIs) were assessed using the Cox proportional hazards model. A 2-sided 5% significance level was used throughout. Statistical calculations were performed using the Statistical Analysis Systems, version 9.1 (SAS Institute, Cary, North Carolina).
Results
A total of 343 consecutive patients (age 69.9 ± 11.9 years, 70.3% men) underwent revascularization for ULMCA disease from April 2003 to January 2007 at our institution. Of the 343 patients, 120 underwent PCI and 223 underwent CABG. Diagnostic angiograms were not available for 15 CABG patients who were excluded from the present analysis. The median follow-up was 1,031 days (interquartile range 861 to 1,260) in the PCI group and 1,339 days (interquartile range 979 to 1,622) in the CABG group. The median SYNTAX score was 26 (range 10 to 68.5) in the PCI group and 28 (range 10 to 49) in the CABG group. The SYNTAX score distribution was skewed toward greater values in the PCI group (skewness coefficient 0.63). In contrast, the CABG group had an almost normal-looking score distribution. The patients were divided into quartiles according to the SYNTAX score distribution: PCI group: quartile 1, SYNTAX score 10 to 19; quartile 2, SYNTAX score 19.5 to 24; quartile 3, SYNTAX score 26 to 35; and quartile 4, SYNTAX score 36 to 68.5; and CABG group: quartile 1, SYNTAX score 10 to 21; quartile 2, SYNTAX score 22 to 27; quartile 3, SYNTAX score 27 to 34; and quartile 4, SYNTAX score 35 to 49.
The baseline clinical characteristics in the different quartiles are summarized in Table 1 . The baseline clinical characteristics were similar among the different quartiles, except for the ejection fraction in the PCI group and the family history of coronary artery disease and ejection fraction in the CABG group. The patients in the higher quartiles tended to have a lower ejection fraction in the CABG group and the patients in the highest quartile in the PCI group had a significantly lower ejection fraction compared to the lower 3 quartiles.
| Characteristic | PCI (n = 120) | CABG (n = 208) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 (n = 30) | Q2 (n = 28) | Q3 (n = 31) | Q4 (n = 31) | p Value | Q1 (n = 48) | Q2 (n = 53) | Q3 (n = 53) | Q4 (n = 54) | p Value | |
| Age (years) | 67.9 ± 15.3 | 70.8 ± 14.6 | 68.4 ± 14.1 | 76.3 ± 10.0 | 0.07 | 67.8 ± 10.5 | 70.1 ± 11.2 | 70.7 ± 9.6 | 68.9 ± 11.9 | 0.56 |
| Men | 57 (17%) | 50 (14%) | 68 (21%) | 58 (18%) | 0.59 | 71 (34%) | 86 (44%) | 66 (34%) | 80 (43%) | 0.066 |
| Body mass index (kg/m 2 ) | 29.7 ± 10.1 | 28.1 ± 8.0 | 28.2 ± 4.2 | 27.0 ± 6.8 | 0.91 | NA | NA | NA | NA | NA |
| Diabetes mellitus | 27 (8%) | 36 (10%) | 32 (10%) | 45 (14%) | 0.49 | 31 (15%) | 30 (16%) | 32 (17%) | 22 (12%) | 0.66 |
| Hypertension ⁎ | 72 (21%) | 71 (20%) | 71 (22%) | 87 (27%) | 0.36 | 79 (38%) | 76 (39%) | 75 (39%) | 72 (39%) | 0.88 |
| Hyperlipidemia † | 79 (23%) | 68 (19%) | 71 (22%) | 81 (25%) | 0.62 | 81 (39%) | 80 (41%) | 71 (37%) | 76 (41%) | 0.61 |
| Current smoker | 18 (5%) | 18 (5%) | 13 (4%) | 25 (7%) | 0.71 | 10 (5%) | 18 (9%) | 15 (8%) | 24 (13%) | 0.34 |
| Ejection fraction | 54.6 ± 14.1 | 57.4 ± 9.6 | 54.8 ± 13.1 | 47.8 ± 14.5 | 0.03 | 56.7 ± 8.9 | 55.5 ± 8.6 | 52.0 ± 12.7 | 51.5 ± 13.1 | 0.048 |
| Chronic obstructive pulmonary disease | 13 (4%) | 14 (4%) | 6 (2%) | 10 (3%) | 0.76 | 8 (4%) | 12 (6%) | 12 (6%) | 13 (7%) | 0.90 |
| Peripheral vascular disease | 28 (8%) | 18 (5%) | 23 (7%) | 26 (8%) | 0.85 | NA | NA | NA | NA | NA |
| Intra-aortic balloon pump | 36 (10%) | 39 (11%) | 58 (18%) | 66 (19%) | 0.07 | NA | NA | NA | NA | NA |
| Unstable angina | 30 (9%) | 43 (12%) | 23 (7%) | 35 (11%) | 0.40 | 23 (11%) | 29 (15%) | 33 (17%) | 20 (11%) | 0.47 |
| Previous myocardial infarction | 28 (8%) | 25 (7%) | 29 (9%) | 23 (7%) | 0.95 | 13 (6%) | 24 (12%) | 29 (15%) | 20 (11%) | 0.24 |
| Previous percutaneous coronary intervention | 20 (6%) | 36 (10%) | 19 (6%) | 23 (7%) | 0.47 | NA | NA | NA | NA | NA |
| Previous stroke | 11 (3%) | 4 (1%) | 6 (2%) | 6 (2%) | 0.78 | 4 (2%) | 6 (3%) | 10 (5%) | 13 (7%) | 0.39 |
| Chronic kidney disease | 7 (2%) | 0 (0%) | 13 (4%) | 10 (3%) | 0.30 | 8 (4%) | 4 (2%) | 2 (1%) | 6 (3%) | 0.47 |
⁎ Blood pressure >120/80 mm Hg.
In the PCI group, 7 patients (23%) in quartile 1, 6 (19.3%) in quartile 2, 3 (10%) in quartile 3, and 11 (37.9%) in quartile 4 died. The higher quartiles were associated with significantly increased mortality rates compared to the lower quartiles (37.9% in quartile 4 vs 17.5% in quartiles 1 to 3; p = 0.015; Figure 1 A). Similarly, higher quartiles were associated with significantly increased MACCE rates (52.2% for quartiles 2 to 4 vs 23.3% for quartile 1; p = 0.013; Figure 1 A). In contrast, no statistically significant difference in the MACCE rates (p = 0.45) or mortality (p = 0.179) was found among the different quartiles when the SYNTAX score was applied to the CABG group ( Figure 1 B).
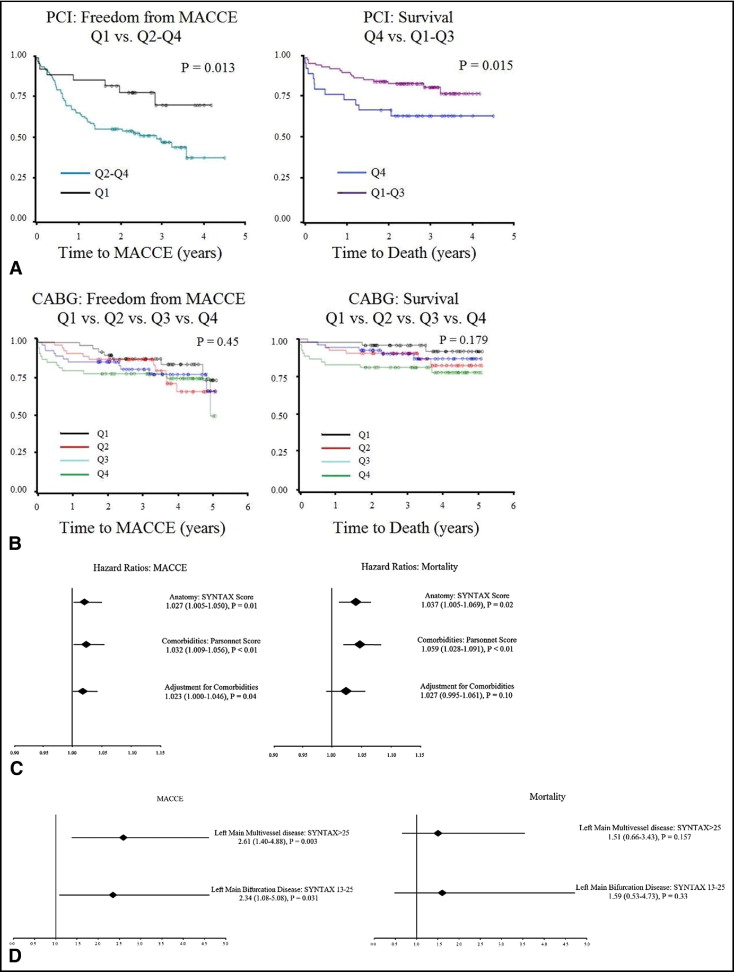
Because both systemic co-morbidities (as assessed by the Parsonnet score) and coronary anatomy (as assessed by the SYNTAX score) can predict the outcomes, we evaluated the ability of the SYNTAX score to independently predict the outcomes in the PCI group, after adjusting for the co-morbidities using the Parsonnet score ( Table 2 ). When assessed individually, both the SYNTAX score (HR 1.037, 95% CI 1.005 to 1.069, p = 0.021) and the Parsonnet score (HR 1.059, 95% CI 1.028 to 1.091, p = 0.0002) were significant predictors of mortality. After entering the Parsonnet score as a covariate in the Cox proportional hazards model, the SYNTAX score continued to show a trend, although not statistically significant, toward predicting mortality (HR 1.027, 95% CI 0.995 to 1.061, p = 0.104; Figure 1 C).



