Although the American Heart Association recommends a prehospital electrocardiogram (ECG) be recorded for all patients who access the emergency medical system with symptoms of acute coronary syndrome (ACS), widespread use of prehospital ECG has not been achieved in the United States. A 5-year prospective randomized clinical trial was conducted in a predominately rural county in northern California to test a simple strategy for acquiring and transmitting prehospital ECGs that involved minimal paramedic training and decision making. A 12-lead ECG was synthesized from 5 electrodes and continuous ST-segment monitoring was performed with ST-event ECGs automatically transmitted to the destination hospital emergency department. Patients randomized to the experimental group had their ECGs printed out in the emergency department with an audible voice alarm, whereas control patients had an ECG after hospital arrival, as was the standard of care in the county. The result was that nearly 3/4 (74%) of 4,219 patients with symptoms of ACS over the 4-year study enrollment period had a prehospital ECG. Mean time from 911 call to first ECG was 20 minutes in those with a prehospital ECG versus 79 minutes in those without a prehospital ECG (p <0.0001). Mean paramedic scene time in patients with a prehospital ECG was just 2 minutes longer than in those without a prehospital ECG (95% confidence interval 1.2 to 3.6, p <0.001). Patients with non–ST-elevation myocardial infarction or unstable angina pectoris had a faster time to first intravenous drug and there was a suggested trend for a faster door-to-balloon time and lower risk of mortality in patients with ST-elevation myocardial infarction. In conclusion, increased paramedic use of prehospital ECGs and decreased hospital treatment times for ACS are feasible with a simple approach tailored to characteristics of a local geographic region.
Acquisition of a prehospital 12-lead electrocardiogram (ECG) in patients with ST-elevation myocardial infarction (STEMI) has been shown to result in greater use of reperfusion therapy, faster reperfusion times, and a trend for lower mortality. Despite these benefits, <1/4 of patients with STEMI transported by emergency medical services (EMSs) in the United States receive a prehospital ECG. Our goal was to select a county that was not providing prehospital ECG, develop a tailor-made program for this county, and evaluate its effectiveness in a prospective randomized clinical trial. The tailor-made prehospital electrocardiographic program we developed involved synthesis of a 12-lead ECG from a 5-electrode configuration with continuous ST-segment monitoring and automatic cell phone transmission of ECGs to the destination emergency department (ED) when ST-segment events occurred in the field. Our intervention was termed “Synthesized Twelve-lead ST Monitoring and Real-time Tele-electrocardiography” (ST SMART) and we implemented it in a county in northern California. An aim of the present analysis was to determine whether the ST SMART prehospital electrocardiographic program would result in better paramedic use of prehospital ECG than the National Registry–reported use of 24.7%. Additional aims were to compare patients with and without a prehospital ECG in paramedic scene time, hospital time to treatment (STEMI, door to balloon; non-STEMI and unstable angina pectoris, door to first intravenous acute coronary syndrome [ACS] drug), and survival over the 5-year span of the study.
Methods
The ST SMART study was a prospective randomized clinical trial in Santa Cruz County, California from June 2003 to June 2009. We purposely chose to implement the ST SMART program in Santa Cruz County because it is representative of counties across the United States without prehospital electrocardiographic programs. The county has no large academic medical centers, consists of just 445 square miles with a limited EMS budget, and has geographic challenges for rapid ambulance transport. The county is mostly coastal mountain range with about 25% of the 255,602 residents living in rural areas served by a network of fragile roads that are likely to be closed periodically each winter due to flooding, washouts, mudslides, and falling trees. When the study began in 2003, median time from 911 call to ED arrival was 39.5 minutes, which makes electrocardiographic transmission from the field a logical choice to investigate for decreasing hospital time to treatment.
The county has 2 community hospitals in small cities located 10 miles apart and these hospitals participated in the study. The larger of the 2 hospitals (admission capacity 232) had full cardiac services including cardiac surgery and a cardiac catheterization laboratory providing percutaneous coronary intervention. However, catheterization laboratory personnel were not on-site at night or on weekends so they had to be called to the hospital if a patient required primary percutaneous coronary intervention for acute MI. The prestudy door to balloon time for this hospital was 105 minutes (National Registry of Myocardial Infarction database). The second hospital (admission capacity 102) in an agricultural region serves a population that is 75% Latino with a low rate of health insurance and the county’s highest rate of unemployment. Because this hospital did not have primary percutaneous coronary intervention capability, patients with STEMI were usually transferred to the larger hospital.
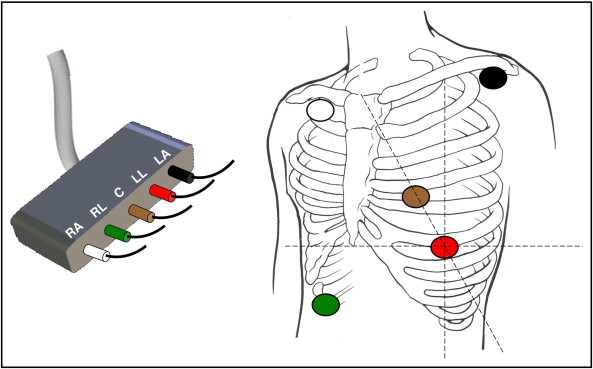
All 26 paramedic-staffed emergency vehicles responding to 911 calls in the county were equipped with portable monitor–defibrillators (Lifepak12, Physio-Control, Redmond, Washington) that were modified with special study software to (1) synthesize a 12-lead ECG from 5 electrodes, (2) measure ST amplitudes in all 12 leads every 30 seconds, and (3) automatically transmit an ECG to the destination ED if there was a change in ST amplitude of 0.2 mV in ≥1 lead or 0.1 mV in ≥2 contiguous leads lasting 2.5 minutes. The 5-electrode lead configuration that was developed for the ST SMART study is shown in Figure 1 . The synthesized 12-lead ECG was validated in a study reported previously.
The ST SMART portable monitor–defibrillator device collected 20 seconds of electrocardiographic data and then selected the 10 seconds with the best signal-to-noise ratio for developing a noise-free median beat, from which ST-segment measurements were made in all 12 leads. If 1 20-second sample was unacceptably noisy, the device did not use it for ST-segment measurements but rather analyzed the subsequent 20 seconds of data. The ST SMART device used a bandwidth of 0.05 to 150 Hz, which is the filtering recommended for diagnostic standard 12-lead ECGs.
All 83 county paramedics were taught to apply the 5 electrodes and manually transmit an initial ECG for patients who had symptoms of ACS ( Table 1 ). This initial manual electrocardiographic transmission activated the continuous ST-segment monitoring software that was otherwise inactive for routine rhythm monitoring of patients without ACS. All subsequent transmissions of ST-event ECGs occurred automatically without paramedic decision making. If transmission failed because of poor cell phone coverage, the software would automatically redial up to 3 attempts to transmit an ECG. Paramedics were instructed not to delay at the scene but rather to allow the device to transmit the ECG while traveling to the hospital. They visualized a single limb lead for routine rhythm monitoring and did not see the synthesized 12-lead ECG in the field.
| Patients who call 911, are ≥30 years old, are not in cardiac arrest, and have any of the following |
| 1. Chest pain or pressure, arm or jaw pain |
| 2. New-onset shortness of breath, not due to asthma |
| 3. Syncope, not due to drug overdose or intoxication |
| If accompanied by nausea/vomiting or sweating, electrocardiogram should definitely be transmitted |
A central computer received transmitted ECGs and special software randomized the patient to an experimental or control group. Patients randomized to the experimental group had their initial and any subsequent ST-event ECGs printed out in the destination ED with an audible voice alarm stating “incoming ECG from the field.” Patients in the control group had an ECG after hospital arrival, which was the standard of care in the county.
Emergency physicians examined incoming ECGs from the field to determine whether the patient had a STEMI. If so, the cardiologist on call was alerted and the cardiac catheterization laboratory personnel were called in. If personnel were on-site and ready at the time the patient reached the hospital, the patient bypassed the ED and went directly to the cardiac catheterization laboratory for primary percutaneous coronary intervention. Because the synthesized ECG was investigational, a standard 12-lead ECG was required in the hospital to confirm the diagnosis.
Institutional review boards of the University of California at San Francisco and the 2 hospitals approved the study with a waiver of consent in the field to avoid delays in patients reaching the hospital due to the study. Community consent was obtained by a front-page report in the county’s newspaper ( Santa Cruz Sentinel ) and by posting information on hospitals’ and EMS agencies’ Web sites, including the fire department and American Medical Response ambulance company. Patients were invited to participate in the study by a research nurse after they reached the hospital or, if discharged from the ED, by a letter followed by a telephone call from the research nurse. If patient consent was not obtained, their prehospital electrocardiographic data that had already been collected were not used in the analysis.
American College of Cardiology key data elements for measuring clinical management and outcomes of patients with ACS were used to define variables for the study, including patient characteristics (demographics, coronary risk factors, cardiac history), clinical presentation, diagnostic tests, percutaneous coronary intervention or other procedures, medications, and patient outcomes. Electrocardiographic criteria for STEMI and non-STEMI were defined by new universal criteria for MI. These criteria included ST-segment elevation at the J-point with cut-off points ≥0.2 mV in men and ≥0.15 mV in women in leads V 2 to V 3 and/or ≥0.1 mV in other leads, or horizontal or downsloping ST-segment depression ≥0.05 mV and/or T-wave inversion of ≥0.1 mV. All electrocardiographic criteria had to be present in 2 contiguous leads.
Unstable angina pectoris was defined as angina or equivalent without biomarker evidence of necrosis with any 1 of the 3 following features: (1) angina occurring at rest and prolonged, usually >20 minutes, (2) new-onset angina with Canadian Cardiovascular Society classification ≥III severity, or (3) recent acceleration of angina reflected by an increase in severity of ≥1 Canadian Cardiovascular Society class to class ≥III.
Because patient report of symptom onset is often unreliable and is missing or variable between EMSs and hospital records for the same patient, we used 911 call time as a surrogate for symptom onset. The 911 call time was time stamped by the computer when the call was picked up by the dispatcher at an EMS call center. These times could not be edited after the call was closed. Computer time was automatically synchronized with official Greenwich Time every day.
To determine the true denominator of ACS cases over the study period, electronic databases from the 2 hospitals were analyzed for all patients during the 5-year enrollment period who were transported by EMSs and who had an International Classification of Diseases, Ninth Revision code of MI or unstable angina pectoris. Then, to confirm that the MI or unstable angina pectoris was a “presenting” condition, rather than a complication after hospital admission, all EMS prehospital care reports were reviewed. After determining the true denominator of total ACS cases in the county over the 5-year period, we determined EMS use by calculating the proportion of patients with ACS who had a prehospital ECG transmission.
Because key time variables (911 call to first ECG, door to balloon, door to drug) were skewed, a log-transformation of these times was applied to normalize the distribution and 2-tailed t tests for independent samples were used to compare control and experimental groups. Mann-Whitney nonparametric test was also used for all time comparisons between groups. Survival analysis with log-rank Mantel-Cox test was used to test differences between control and experimental patients’ survival over the 5-year follow-up period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


