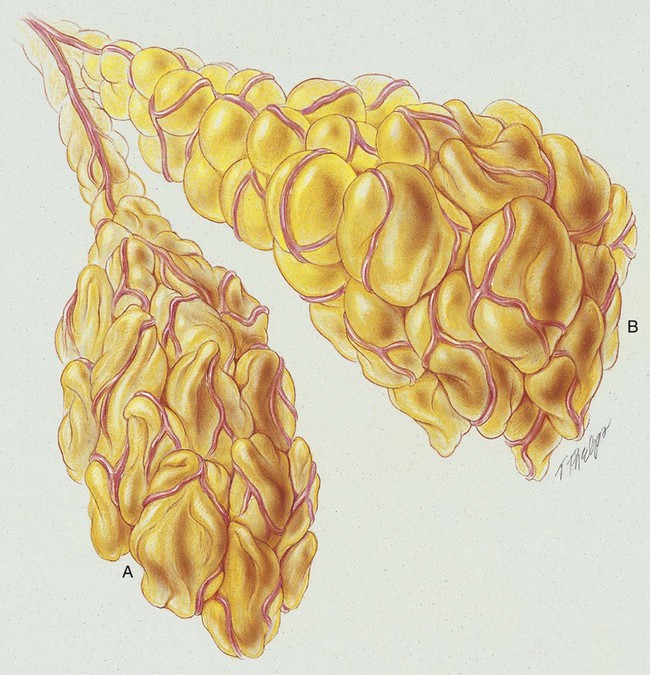
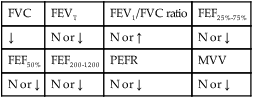
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with postoperative atelectasis. • Describe the causes of postoperative atelectasis. • List the cardiopulmonary clinical manifestations associated with postoperative atelectasis. • Describe the general management of postoperative atelectasis. • Describe the clinical strategies and rationales of the SOAP presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. Atelectasis, in the strict sense of the term, is defined as the condition in which the lungs of the newborn remain unexpanded (airless) at birth. In the clinical setting, however, the meaning of atelectasis in all age groups generally is broadened to include partial or total collapse of previously expanded lung regions. Atelectasis may be limited to the smallest lung unit (i.e., alveolus or primary lobule*; see Figure 42-1), or it may involve an entire lung or a segment or lobe of the lung. In this chapter, postoperative atelectasis is used as a prototype of the atelectasis process. Postoperative atelectasis commonly is seen after upper abdominal and thoracic surgical procedures.
Postoperative Atelectasis
Anatomic Alterations of the Lungs