Physiology and Physiologic Studies of the Esophagus
André C. H. Duranceau
Pasquale Ferraro
Normal Esophageal Function
Pharynx
The function of the pharynx has received less attention than that of the esophagus, partly because water-infused systems do not accurately measure pressure events in the pharynx. Dodds and associates,34 however, measured pharyngeal contractions in human subjects using intraluminal strain gauges and found average contraction pressures of 200 mm Hg, with pressures recorded up to 600 mm Hg. The pharyngeal contraction lasts about 0.2 to 0.5 seconds. The rapidity of the pharyngeal contraction wave (9–25 cm/sec) requires it to be recorded in this fashion. Frequently an initial increase in pressure occurs before the single pharyngeal peak. This increase is usually thought to be caused by the tongue thrust, the “trapped” air column, or the advancing bolus.
Upper Esophageal Sphincter
The upper esophageal sphincter (UES) is a high-pressure zone that separates the pharynx from the esophagus. Its most important role may be to prevent esophagopharyngeal regurgitation; gastroesophageal reflux occurs in normal individuals, and the sphincter may prevent the regurgitation of gastric contents into the pharynx. The sphincter may also have a role in preventing the entry of air into the esophagus, although this probably is not an important function.
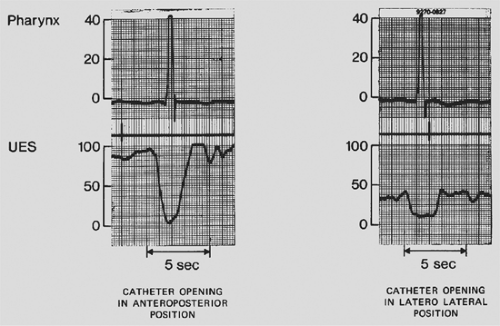
The cricopharyngeus is a muscle sling attached posteriorly to both laminae of the cricoid cartilage. The configuration and location of this muscle give it a role similar to that of the bowstring, with tension exerted mostly in the anteroposterior direction. Winans82 has documented this asymmetry within the sphincter. Using an eight-lumen catheter with all recording ports arranged circumferentially at the same level, he observed pressures of 100 mm Hg in the anteroposterior position and 30 mm Hg in the lateral orientation (Fig. 131-1).
It is generally agreed that the cricopharyngeus is the major component of the UES. This muscle is approximately only 1 cm long, however, so it cannot account totally for the 2- to 3-cm width of the high-pressure zone of the UES recorded by Winans82 and Welch and colleagues.80
As suggested by Airdar,2 passive elastic forces may play a role in the maintenance of closure of the UES in humans. From the investigations of Asoh and Goyal5, this certainly appears to be true in the opossum, in which a residual closing pressure remains in the anteroposterior direction after the nervous supply to the sphincter muscle is removed. Nevertheless, UES pressure is probably predominantly a result of tonic muscle contraction. Shipp and coworkers73 recorded sustained electromyographic activity from the cricopharyngeus muscle in humans.
Sokol and associates75 have reported that during swallowing, the UES moves vertically approximately 2 cm. This movement has led to methodologic problems in the study of UES function using a perfused side-hole catheter. Gerhardt46 and Welch80 and
their colleagues, sampling via rapid pull-through techniques in normal controls, have recorded anteroposterior basal tone in the range of 100 to 130 mm Hg.
their colleagues, sampling via rapid pull-through techniques in normal controls, have recorded anteroposterior basal tone in the range of 100 to 130 mm Hg.
Adaptation by Dent29 and Kahrilas and associates52 of the sleeve manometric technique for the study of the UES has provided further insights into UES function. Basal UES pressure was found by Kahrilas and colleagues53 to decrease during sleep to a level of 6 to 13 mm Hg, whereas in awake subjects it was approximately 60 mm Hg. Circumferential pressure-sensing transducers can provide direct measures of the circumferential squeeze by the sphincter. As well, the new electronic topographic manometry, with its increased number of pressure sensors, may provide a three-dimensional display of pressure at the pharyngoesophageal junction.21,66
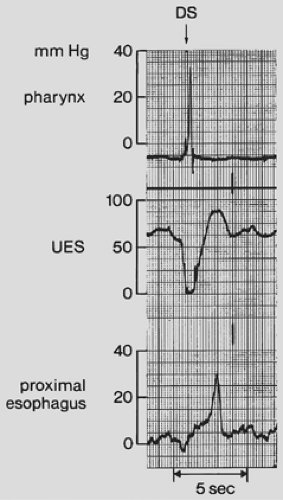
Relaxation of the UES that allows the passage of material through it appears to occur with the onset of swallowing (Fig. 131-2), and, as noted by Kahrilas and associates,55 it also occurs independent of swallowing to allow belching. Several stimuli that increase UES tone have been studied, including balloon distention in the esophagus, reported by Creamer and Schlegel,25 Gerhardt,46 and Kahrilas,53 and their colleagues. Also studied were acidification of the esophageal lumen, recorded by Gerhardt and associates,46 and slow, intraesophageal gas insufflation (as opposed to rapid distention), which produces relaxation, as noted by Kahrilas and coworkers.55
A contraction of the high-pressure zone is observed after UES relaxation. It occurs with the progression of the pharyngeal contraction toward the cervical esophagus. This closing pressure may increase the sphincter pressure to twice its resting pressures. Baseline pressures then return in the sphincter, and contraction continues as primary peristalsis in the cervical esophagus (see Fig. 131-2).
Esophageal Body
The musculature of the esophageal body is not tonically contracted. The role of the longitudinal muscle in esophageal function is difficult to study. Sugarbaker and colleagues76 have suggested that it may improve the mechanical properties of the esophagus for bolus transport. The circular muscle, however, is much easier to study because of its lumen-occluding contraction, which passes down the esophageal body, pushing contents ahead of it.
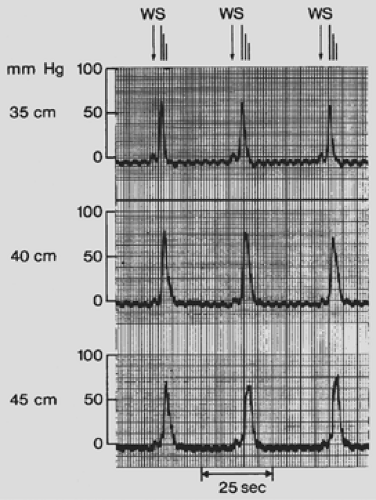
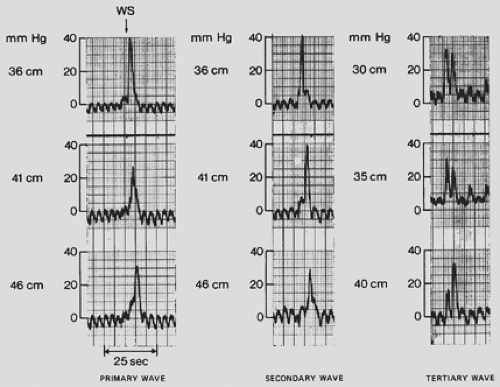
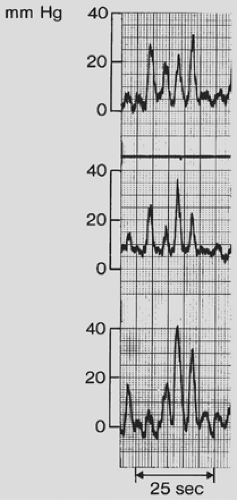
Primary peristalsis is triggered voluntarily by swallowing but thereafter is not under voluntary control (Fig. 131-3). Not all peristaltic waves are complete in normal subjects. In response to dry swallows, complete waves occur on only approximately two-thirds of occasions. Specific patterns can be observed, such as the peristaltic “fade-out” at the aortic arch level. Tertiary contractions in the distal esophagus can be recorded in response to de- glutition (Figs. 131-4 and 131-5). Occasionally, no detectable wave can be seen in response to swallows, as reported by Dodds and coworkers31 and Hollis and Castell.48 As observed in our control population,40 however, water swallows produce more complete peristaltic sequences. Other factors that may influence primary peristaltic activity are posture and age: a decrease in amplitude is seen when the subject is supine and in men >80 years of age, as reported by Kaye and Wexler56 and Hollis and Castell.48
The esophageal wave travels down the esophageal body at a speed of 2 to 5 cm/sec. The wave of contraction that occurs in response to deglutition progresses slowly in the proximal striated muscle area. It slows further at the striated–smooth muscle junction and then accelerates in the lower half of the
esophagus except just above the lower sphincter, where it is seen to slow again (see Fig. 131-3). In similar fashion, peak contraction pressures are weak in the striated esophagus and stronger in the distal esophagus. The values obtained in recording esophageal body motility vary from source to source, and the influence of different recording techniques is well documented.
esophagus except just above the lower sphincter, where it is seen to slow again (see Fig. 131-3). In similar fashion, peak contraction pressures are weak in the striated esophagus and stronger in the distal esophagus. The values obtained in recording esophageal body motility vary from source to source, and the influence of different recording techniques is well documented.
Peristaltic sequences can also be modified by the rate of swallowing. Swallows at 5-second intervals or less tend to inhibit peristalsis completely; completely normal sequences occur only when swallows are taken at >20-second intervals, as reported by Ask and Tibbling4 and Meyer and colleagues.63
The control of primary peristalsis is complex. The striated muscle is probably directly controlled by the nucleus ambiguus through the vagus, whereas the smooth muscle portion is probably controlled by a combination of extrinsic vagal and local neural control. Both cholinergic excitatory and nonadrenergic, noncholinergic inhibitory mechanisms were suggested by Christensen,22 as well as by Sarna72 and Crist26 and their coworkers, to be involved in normal peristalsis.
Secondary peristalsis refers to peristaltic waves that are not controlled by swallowing but usually are in response to esophageal distention or irritation. These secondary waves, which have been studied less extensively than primary peristaltic contractions, probably have a “housekeeper” role in clearing refluxed material from the esophagus (see Fig. 131-4).
Tertiary contractions (Fig. 131-6; also see Figs. 131-4 and 131-5) can be abnormal contractions occurring in response to swallowing (see Figs. 131-5 and 131-6), or they can appear spontaneously between swallows (see Figs. 131-4 and 131-6). Rubin71 has suggested a relationship between esophageal motor disorders and the emotional states of patients during recordings. Nonpropulsive contractions and repetitive spontaneous contraction were observed when motor function of the esophageal body was recorded during “affectively charged conversation.” Spontaneous tertiary contractions occur in healthy individuals but are observed more often in patients with strongly anxious personalities (see Figs. 131-4, 131-5 and 131-6).
Lower Esophageal Sphincter
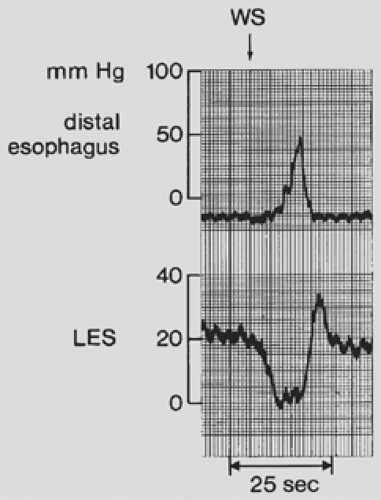
It is now accepted that there is both a physiologic lower esophageal sphincter (LES), as emphasized by Dodds and
associates,32 and an anatomic LES, as documented by Liebermann-Meffert and colleagues,62 and that the maintenance of basal tone is the major mechanism preventing gastroesophageal reflux (Fig. 131-7).
associates,32 and an anatomic LES, as documented by Liebermann-Meffert and colleagues,62 and that the maintenance of basal tone is the major mechanism preventing gastroesophageal reflux (Fig. 131-7).
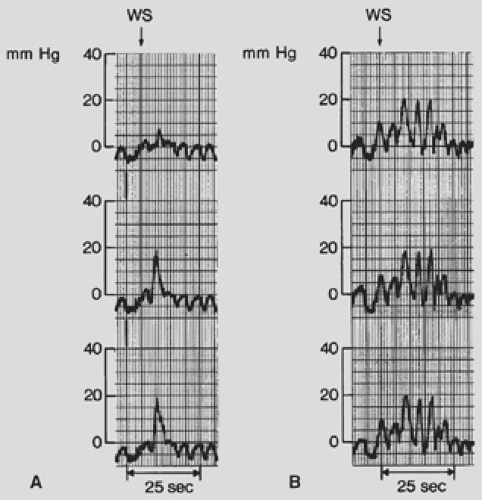 Figure 131-5. A. Single tertiary contraction in response to a voluntary swallow. B. Repetitive nonpropulsive activity after deglutition. WS, wet swallow. |
Winans81 has pointed out that the pressure profile of the LES shows considerable radial asymmetry, with the highest pressures being recorded in the left posterior orientation. The reasons for this asymmetry are not clear. As with the UES, the LES relaxes to allow passage of luminal contents in either direction, relaxation occurring with peristaltic activity in the esophageal body or gaseous distention in the fundus of the stomach.
The mechanisms underlying the control of basal tone in the LES are not well understood. Fisher43 and Dodds32 and their coworkers wrote that cholinergic vagal drive seems a likely candidate, at least in part. Circulating hormones, such as gastrin, are considered less likely to contribute to basal tone. Basal tone varies greatly in normal individuals. In the fasting state, the migrating motor cycle may influence LES pressure, which tends to increase during the cycle, as recorded by Dent and associates,27 and can reach high levels during phase III gastric contractions. Basal tone rises during increases in intra-abdominal pressure; it remains controversial whether this change is a reflex rise in pressure or an increased diaphragmatic compression of the LES, as suggested by Boyle and Cohen.15 Perhaps the evidence, as reported by Landers and Jamieson,59 is beginning to favor the involvement of a reflex.
Relaxation of the LES occurs with swallowing, with esophageal body distention, and with gastric fundus distention. Transient LES relaxation (TLESR) is a phenomenon of relaxation lasting 5 to 30 seconds, described by Dent and colleagues.28 These TLESRs probably arise as a result of gastric distention, leading to nonadrenergic, noncholinergic inhibition of LES
tone. As suggested by Dent28 and Dodds33 and associates, such LESRs may be the most important factor in both physiologic and pathologic reflux.
tone. As suggested by Dent28 and Dodds33 and associates, such LESRs may be the most important factor in both physiologic and pathologic reflux.
Other factors that should be mentioned, as noted by Bona- vina and colleagues,12 as contributing to pressure in the LES region are extrinsic compression by diaphragmatic muscle, which is probably most important during straining, and the intra-abdominal position of the LES, which allows intra-abdominal pressure changes to buttress the LES. The tonic contractions of the crus of the diaphragm, demonstrated by electromyography during various physiologic events, support the concept of “extrinsic LES” as proposed by Mittal and colleagues.65
The Variables Affecting the Recording of Esophageal Motility
Accurate recording of the physiologic events that occur with swallowing leads to an understanding of the pathophysiologic mechanisms of esophageal disorders. Although initial motility studies were mostly oriented toward research, evaluation of motor function is now considered essential in the assessment of esophageal disease.
Esophageal motility studies record pressures simultaneously at several levels within the esophagus, allowing evaluation of the esophageal body and of the sphincters that close the upper and lower ends of the esophagus.
Intraluminal manometry is the method best suited for the study of motility in humans. Technical refinements in the past two decades, discussed by Dodds,35 by Castell and co-workers,17 and more recently by Pandolfino and Kahrilas,66 have led to greatly improved capability for accurate measurement with current techniques.
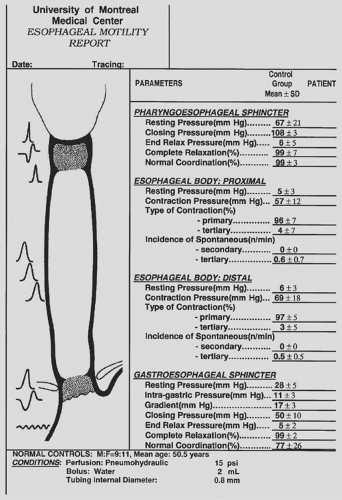
Meticulous attention to the recording method and the numerous factors that may affect it is necessary. For this reason, it is important to have a control population evaluated with the local recording technique. This effort ensures more accuracy and gives a better perspective of what can be interpreted as normal in a patient population (Fig. 131-8). The recording system used is usually water-perfused, and the patient is supine while being studied.
The preferred system of fluid-filled catheter manometry includes a pneumohydraulic infusion pump and small (0.8-mm internal diameter) polyvinyl tubing. This system reduces the high infusion rate required to record accurately the rapidly changing pressures in using a mechanically driven pump with syringes. Tutuian79 has recently documented that single-use disposable catheters made with small balloons filled with air could be a valuable alternative. Table 131-1 summarizes the variables that may affect recording of esophageal physiology and its interpretation.
Constantly perfused catheters ensure reliability in the pressures recorded. Without perfusion, considerable variability is observed from patient to patient. Pope67 has reported that if mechanical perfusion is used, the infusion rate shows a direct influence on pressure values. To overcome the inconvenience of infusing high volumes of fluid during a study and allow more accurate changes in pressure over time (ΔP/ΔT) to be recorded, a constant-pressure infusion system was developed by Arndorfer and colleagues.3 It pushes small volumes of water through a noncompliant system and is now more commonly used (Fig. 131-9).
Miniaturized pressure transducers integrated into a recording catheter provide side recording strain gauges for esophageal body contractions as well as circumferential gel-surrounded transducers for accurate recording of sphincters. These pressure transducers provide more accurate pharyngeal pressure recordings.
The new topographic esophageal manometry provides an increased number of closely positioned pressure sensors, offering a dynamic presentation of peristalsis. The initial cost of the more sophisticated systems, their repair or upgrade expenses, and the advantages they offer over conventional water-perfused manometry need to be confirmed.66
When a perfused system is being used, the size of the motility tube influences the recorded pressures, with an increase in size leading to an increase in the pressure recorded. The length of the recording tube may impose a “dragging” effect on the system and result in lower recorded pressures.
Both esophageal sphincters have an irregular configuration and exhibit vertical movement during deglutition. Special attention to these areas is required if reliable recordings are to be obtained. Dent29 devised a 5-cm-long perfused sleeve that
provides reliable LES pressure measurements despite esophageal movement. A similar sleeve catheter was developed by Kahrilas and colleagues52 for the study of the UES. This catheter follows the sleeve principle and permits reliable recording despite movement of the catheter in the sphincter. The use of computer imaging with circumferential pressure measurements taken simultaneously can generate a sphincter pressure vector volume. Such an assessment is considered reliable and superior to the pullback method used in standard manometry.66 Both sleeve recordings and the sphincter pressure vector volume provide optimal pressure readings within the sphincter. Despite more accurate recording of pressures in both sphincters, interpretation of relaxation and coordination of these areas remain to be improved.
provides reliable LES pressure measurements despite esophageal movement. A similar sleeve catheter was developed by Kahrilas and colleagues52 for the study of the UES. This catheter follows the sleeve principle and permits reliable recording despite movement of the catheter in the sphincter. The use of computer imaging with circumferential pressure measurements taken simultaneously can generate a sphincter pressure vector volume. Such an assessment is considered reliable and superior to the pullback method used in standard manometry.66 Both sleeve recordings and the sphincter pressure vector volume provide optimal pressure readings within the sphincter. Despite more accurate recording of pressures in both sphincters, interpretation of relaxation and coordination of these areas remain to be improved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree