Persistent Sciatic Artery
Presentation
A 54-year-old woman with left calf claudication for 40 years has developed similar right-sided symptoms in the past year. Symptoms occur after walking four to five blocks. She has hypertension and hypercholesterolemia. On physical examination, she has 1+ (out of 4) femoral pulses and 3+ popliteal pulses bilaterally. Pedal pulses are 1 to 2+ bilaterally. She has no foot ulcers.
Differential Diagnosis
In a patient with risk factors for atherosclerosis, occlusive disease should be considered first as the etiology for claudication. However, the duration of this patient’s symptoms suggests a potential congenital diagnosis, including aortic coarctation, embryologic arterial abnormalities, or cardiac lesions causing peripheral emboli. In a patient with a stronger pulse at the popliteal level compared to the femoral artery, persistent sciatic artery (PSA) should be suspected.
Workup
Although very rare with an incidence of 0.03% to 0.06%, PSA can result in limb loss if not identified and corrected in select cases, with aneurysms forming in 40% to 61% of PSA cases. The most common presentations are a painful, pulsatile gluteal mass; symptoms of sciatic nerve compression; and distal ischemia, although 40% to 50% are asymptomatic and identified incidentally on computed tomography (CT) scan. The mean age of PSA patients is 57 years with an equal distribution in men and women. PSAs are bilateral in 18% to 22%. Physical exam may identify a pulsatile mass in the buttocks or leg and diminished or absent femoral pulse with the presence of a palpable popliteal pulse (Cowie’s sign). Concomitant findings of varicose veins, persistent sciatic veins, arteriovenous malformations, and abdominal wall capillary hemangiomas have been reported.
Diagnostic Tests and Results
Noninvasive vascular studies with exercise should be done to identify the degree of ischemia. This patient had ankle-brachial indices of 0.68 and 0.74 on the right and left, respectively, decreasing to 0.4 and 0.71 after 1 minute of exercise. She is able to exercise for 5 minutes, completing the 283-yard protocol with right calf weakness. Diagnostic imaging studies include ultrasound, CT angiogram (Fig. 1), and arteriography (Fig. 2A–D) Magnetic resonance arteriography without contrast can be used in patients with renal insufficiency.
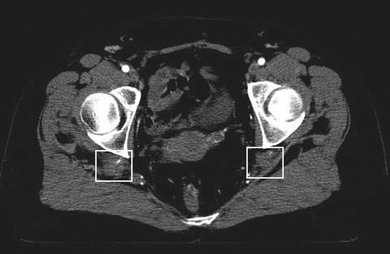
FIGURE 1 CT scan of the abdomen and pelvis demonstrates bilateral thrombosed 2-cm PSA aneurysms (white boxes) from the pelvis to the popliteal arteries.


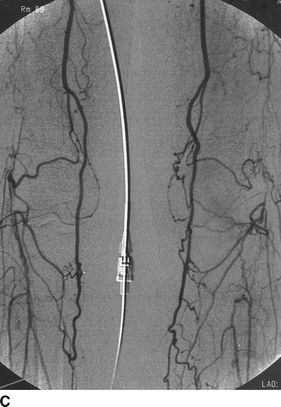
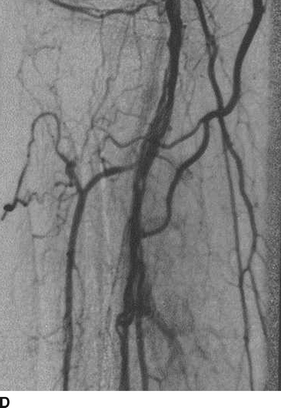
FIGURE 2 Abdominal aortogram with bilateral lower extremity runoff shows a right remnant sciatic artery (white box) that is thrombosed as it exits the pelvis, refilling a tiny fragment at the lesser trochanter level (A). No evidence of the left sciatic artery is noted on arteriogram. The distal bilateral superficial femoral arteries (B) end at the adductor hiatus, and the popliteal arteries refill via two collateral arteries (C). There are luminal irregularities in both popliteal arteries indicative of partially recanalized thrombus (D).
Diagnosis and Treatment
Surgical Approach
Management of PSA with or without aneurysmal changes depends on the degree of symptoms. No intervention is required if PSA is found incidentally or if the patient has stable mild ischemic symptoms, such as the described patient. PSA aneurysm rupture has not been reported, but aneurysm size should be followed serially with ultrasound or CT angiogram.
A PSA aneurysm alone, without significant distal ischemic disease, can be successfully managed with percutaneous embolization as well as exclusion with a stent graft. If catheter-based techniques are unsuccessful, open ligation with or without concomitant arterial revascularization has been described. Interposition grafting, with either prosthetic or vein conduit, from the normal femoral, external iliac, or hypogastric artery to the popliteal artery may be performed in conjunction with aneurysm ligation or endoaneurysmorrhaphy via a retroperitoneal approach. The limb loss rate has been reported as high as 18%, but this includes many patients with primary amputations due to embolic events.
Special Intraoperative Considerations
Excision of the aneurysm should be avoided, as it is often adherent to the sciatic nerve, and footdrop has been reported in open aneurysm repair. In addition, in comparing patients with aneurysm resection/endoaneurysmorrhaphy to those with exclusion/embolization, each had similar improvement in relief of compressive effects. Patients with PSA should also be treated carefully if undergoing hip operations due to the surgical proximity of the aberrant artery or if undergoing renal transplantation to the ipsilateral hypogastric artery.
Postoperative Management
Postoperative follow-up depends on the degree of revascularization or percutaneous treatment, with physical exam, noninvasive studies, and serial imaging (ultrasound or CTA). There is no data to support chronic anticoagulation, although antiplatelet agents would likely be used in patients with concomitant ischemia.
Case Conclusion
This 54-year-old woman has bilateral persistent sciatic arteries with aneurysmal degeneration and stable claudication. She has evidence of prior embolic events, but has little to no flow within the aneurysms on the present examination. Although femoropopliteal reconstruction could be considered, as she has adequate external iliac and common femoral arteries, the patient did not feel that her symptoms were lifestyle limiting and no operation was performed. Serial CT scans were recommended on a yearly basis to assess aneurysm size.



