The door-to-balloon times frequently exceed the recommended delay. We therefore evaluated the performance of a novel “physician-less” cardiac catheterization laboratory (CCL) activation system relying on the automated electrocardiographic diagnosis alone. From January 2010 to 2012, first responders performed electrocardiograms in the field for all patients with a complaint of chest pain or dyspnea. An automated machine diagnosis of “acute myocardial infarction” resulted in immediate CCL activation and direct transfer without human reinterpretation or transmission of the electrocardiogram. Any activation resulting from a nondiagnostic ECG (no ST-segment elevation) was deemed inappropriate and classified as resulting from either human or machine error. Of 155 activations, 136 (88%) were electrocardiographically appropriate. Of these, 128 patients had a final diagnosis of ST-segment elevation myocardial infarction. A door-to-balloon time of <90 minutes was achieved in 99%, the procedural success was high (94%), and the overall mortality was low (3%). Of the electrocardiographically appropriate activations, 8 (5%) were false-positive results. The remaining 19 activations (12%) were inappropriate. Compared with the electrocardiographically appropriate activations, those with inappropriate activations had significantly greater rates of hypertension (p = 0.0070) and known coronary artery disease (p = 0.0008) and higher presenting heart rates (p <0.0001). The causes for inappropriate activation were approximately evenly split between human and machine error. In conclusion, a combination of prehospital automated ST-segment elevation myocardial infarction diagnosis and “physician-less” CCL activation was safe and effective in ensuring target door-to-balloon times in virtually all patients and resulted in an acceptable rate of inappropriate CCL activation.
An ST-segment elevation myocardial infarction (STEMI) diagnosis at first medical contact and prehospital cardiac catheterization laboratory (CCL) activation have been suggested as strategies to reduce door-to-balloon times. However, the possibility exists of an increased burden of false-positive (FP) results and inappropriate activation (IA) of the CCL without real-time physician oversight. We describe the performance of a newly implemented “physician-less” system of automated in-the-field STEMI diagnosis and prehospital CCL activation without prior human electrocardiogram (ECG) interpretation. We have also proposed concise, easily applicable, and nonoverlapping definitions of IA and false-positive activation and describe the factors associated with IA.
Methods
In January 2010, a new system of prehospital STEMI diagnosis and prehospital CCL activation was implemented in the region (247 km 2 ) served by a community hospital with a standalone CCL in Laval, Québec, Canada (population 401,553 in 2011). In accordance with the CCL activation protocol, any patient presenting with a complaint of chest pain or dyspnea had an in-the-field ECG performed by the ambulance technician (first responder without advance care training). An automated electrocardiographic diagnosis of STEMI (“acute myocardial infarction”, Zoll Medical Corporation, Zoll Canada, Mississauga, Ontario, Canada) resulted in CCL team activation by the ambulance technician (simultaneous paging system) and direct patient transfer to the CCL without transmission or reinterpretation of the ECG by medical personnel before the patient’s arrival at the percutaneous coronary intervention center. Ambulance technicians in the province of Québec have basic training in the performance of ECGs but are not trained to interpret them. According to the referral algorithm, any patient with hemodynamic instability is referred to the nearest emergency room.
All consecutive prehospital CCL activations from January 1, 2010 to January 31, 2012 were analyzed as part of a quality of care initiative. The patient demographics, clinical characteristics, in-hospital clinical event data, and ECGs were gathered from the electronic medical records. The CCL procedural data were prospectively collected in a dedicated database, and the landmark time points were abstracted from electronic medical records and the CCL database.
True STEMI was defined as an ST-segment elevation associated with a significant lesion or altered Thrombolysis In Myocardial Infarction flow in a coronary artery corresponding to the myocardial territory on the presenting ECG. FP CCL activation was defined as any activation resulting from an accurately identified elevation in the ST segment but without identification of a corresponding culprit lesion or altered Thrombolysis In Myocardial Infarction flow at angiography (e.g., pericarditis or takotsubo cardiomyopathy). Such CCL activations were judged to be appropriate in the context of a patient with chest pain (ECG appropriate ). In contrast, any activation resulting from a nondiagnostic ECG was considered inappropriate. To qualify as a nondiagnostic ECG, the 2 reviewing cardiologists had to state that they would definitely not have activated the CCL on the basis of the prehospital ECG in a clinical setting of chest pain. In the case of disagreement, there was a provision for a third cardiologist to independently review the ECG. Ambulance technicians were not asked to evaluate the appropriateness in terms of patient age or co-morbidities. However, percutaneous coronary intervention center staff could choose not to proceed with coronary angiography upon evaluation of the patient and ECG, but only after the patient had arrived at the percutaneous coronary intervention center and the CCL team had already been mobilized.
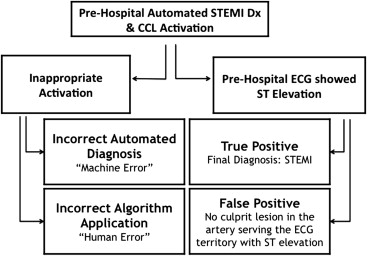
IAs were then subsequently analyzed and categorized as either machine error or human error. Machine error was defined as any machine diagnosis of acute myocardial infarction according to an in-the-field ECG of sufficient quality that had been determined not to show any significant ST-segment elevation, as described. Human error was defined as any failure to observe the established prehospital STEMI diagnosis and referral algorithm. Examples of human error included performing and acting on a prehospital ECG for a patient without a chief complaint of chest pain or dyspnea and failure to ensure a prehospital ECG tracing of sufficient quality. These concepts are described schematically in Figure 1 .
The door-to-balloon and contact-to-balloon times were defined conventionally as the interval between the patient’s arrival at the hospital or first medical contact in the field, respectively, and the time of activation of the first intracoronary device for those undergoing percutaneous coronary intervention. Prehospital system delay was defined as the interval from first medical contact to arrival at the percutaneous coronary intervention center and was calculated for all patients. All times were abstracted from the ambulance technician and CCL reports contained in the patients’ electronic medical records. The timepieces were not synchronized.
Procedural success was defined as <10% residual stenosis and final Thrombolysis In Myocardial Infarction grade 3 flow. System performance was evaluated in terms of quality, efficiency, and safety. The primary quality outcome was the rate of IA, as defined. The secondary quality outcomes were the reasons for IAs, categorized as either human or machine error, and the FP rate. The primary efficiency outcome of interest was the door-to-balloon time for patients with confirmed STEMI. The secondary efficiency outcomes included the proportion of patients with a door-to-balloon time of <90 minutes, the contact-to-balloon time, the proportion of patients with a contact-to-balloon time of <120 minutes, and procedural success. The primary safety outcome of interest was the rate of in-hospital major adverse cardiovascular events (defined as the composite of death, myocardial infarction, stroke, or revascularization), Thrombolysis In Myocardial Infarction major bleeding, and the rate of emergent patient transfer to a cardiac surgery-capable center.
Rates are presented as the total number and percentage of the group total, unless otherwise indicated. Non-normal continuous data are presented as the median and interquartile range and normal continuous data as the mean ± SD. Fisher’s exact and Student’s t tests were used to compare the baseline demographics and co-morbidity rates between the IAs and appropriate activations, as the type of data dictated. Statistical significance was defined as a 2-tailed chance of type I error (alpha) <0.05 for all analyses. All analyses were performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina).
Results
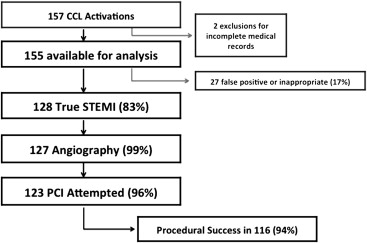
We identified 157 instances in which the described prehospital diagnosis and referral system resulted in CCL activation from the field during the study period ( Figure 2 ). Two patients were excluded because of incomplete data. The baseline patient characteristics for the remaining 155 activations are listed in Table 1 .
| Clinical Characteristic | All Activations (n = 155) | ECG Appropriate | ECG Inappropriate (n = 19) | p Value ∗ | ||
|---|---|---|---|---|---|---|
| All (n = 136) | True STEMI (n = 128) | FP Result (n = 8) | ||||
| Age (yrs) | 65 ± 14 | 65 ± 14 | 65 ± 14 | 64 ± 17 | 72 ± 15 | 0.0584 |
| Men | 99 (73%) | 99 (73%) | 94 (73%) | 5 (63%) | 11 (58%) | 0.1874 |
| Diabetes | 25 (18%) | 25 (18%) | 22 (17%) | 3 (38%) | 5 (26%) | 0.5340 |
| Hypertension | 70 (52%) | 70 (52%) | 64 (50%) | 6 (75%) | 16 (84%) | 0.0070 |
| Dyslipidemia | 68 (50%) | 68 (50%) | 64 (50%) | 4 (50%) | 13 (68%) | 0.1489 |
| Tobacco | 59 (43%) | 59 (43%) | 57 (45%) | 2 (25%) | 3 (16%) | 0.0244 |
| Known or suspected CAD | 17 (12%) | 17 (12%) | 15 (12%) | 2 (25%) | 9 (57%) | 0.0008 |
| Previous revascularization | 15 (11%) | 15 (11%) | 13 (10%) | 2 (25%) | 5 (26%) | 0.0746 |
| Previous stroke or TIA | 6 (4%) | 6 (4%) | 6 (5%) | 0 | 2 (11%) | 0.2545 |
| Peripheral arterial disease | 11 (8%) | 11 (8%) | 10 (8%) | 1 (13%) | 3 (16%) | 0.3827 |
| CRF (CrCl <60 ml/min) | 45 (33%) | 45 (33%) | 41 (32%) | 3 (38%) | 9 (47%) | 0.3034 |
| Dialysis | 3 (2%) | 3 (2%) | 3 (2%) | 0 | 1 (5%) | 0.4127 |
| BMI >30 kg/m 2 † | 38 (30%) | 36 (30%) | 34 (27%) | 2 (29%) | 2 (25%) | – |
| Killip class III-IV | 8 (5%) ‡ | 8 (6%) § | 8 (6%) | NA | NA | – |
| Heart rate (beats/min) | 77 ± 25 | 74 ± 19 | 74 ± 19 | 78 ± 22 | 99 ± 46 | <0.0001 |
∗ Comparison of all ECG appropriate and ECG inappropriate.
† Missing values for 28 patients overall.
‡ Twenty-seven cases not applicable.
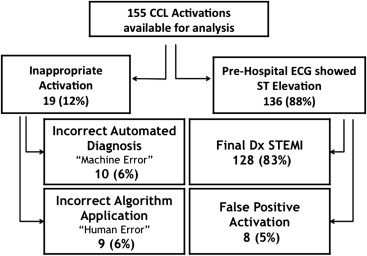
Of the 155 activations, 128 (83%) resulted in a final diagnosis of STEMI (“true STEMI”), 8 patients (5%) had ST-segment elevation on the presenting ECG, but were FP activations, and 19 (12%) were considered IAs (no ST-segment elevation). Of these 19, human error was implicated in 9 (47% of IA), 2/3 of which resulted from acting on poor quality tracings. Machine error occurred in 10 (53%), of which 1/2 were related to a supraventricular tachyarrhythmia >140 beats/min ( Figure 3 ).
The reasons for FP ST-segment elevation in this cohort were peri- or myocarditis in 2 patients, takotsubo cardiomyopathy in 1, Brugada syndrome in 1, coronary vasospasm in 1, known left bundle branch block in 1, and ST-segment changes due to old infarcts in 2 patients.
Compared with those with ECG-appropriate activations, those with IA had significantly higher rates of hypertension (p = 0.0070) and known coronary artery disease (p = 0.0008), and significantly higher presenting heart rates (p <0.0001; Table 1 ). Also, a trend toward older age in the IA group was seen.
In the 123 patients with true STEMI receiving primary percutaneous coronary intervention, the median door-to-balloon time was 46 minutes (interquartile range 39 to 56), and the recommended door-to-balloon time of <90 minutes was achieved in 99% of patients (1 patient had a door-to-balloon time of 98 minutes). More than 75% of patients had a door-to-balloon time of <60 minutes. The median first medical contact (in the field) to balloon (contact-to-balloon) time was 76 minutes (interquartile range 67 to 88), and 98% achieved a contact-to-balloon time of <120 minutes (1 patient had a contact-to-balloon time of 122 minutes and 1 of 132 minutes; Table 2 ). There was a tendency toward longer delays for activations occurring after 11 p.m. , but this had no effect on the proportion of patients achieving the target door-to-balloon time ( Table 3 ). The median prehospital system delay for all 155 patients was 28 minutes (interquartile range 23 to 33).
| Variable | Median (min) | Time <90 min (%) | Time <120 min (%) | Maximum Delay (min) |
|---|---|---|---|---|
| D2B | 46 (38–56) | 99 | 100 | 98 |
| C2B ∗ | 76 (67–88) | 78 | 98 | 132 |
∗ Time of first medical contact was unavailable for 3 patients.
| n | Median (min) | Time <60 min (%) | Time <90 min (%) | Time <120 min (%) | |
|---|---|---|---|---|---|
| D2B time | |||||
| Weekday | 31 | 40 (25–53) | 77 | 97 | 100 |
| Weekday evening | 26 | 46 (39–57) | 85 | 100 | 100 |
| Weekday night | 14 | 55 (44–56) | 79 | 100 | 100 |
| Weekend | 52 | 48 (42–56) | 83 | 100 | 100 |
| C2B time ∗ | |||||
| Weekday | 30 | 65 (47–86) | 37 | 73 | 96 |
| Weekday evening | 26 | 78 (67–89) | 19 | 89 | 100 |
| Weekday night | 14 | 82 (75–86) | 7 | 79 | 100 |
| Weekend | 50 | 79 (71–90) | 6 | 76 | 98 |
∗ Number discrepancies due to missing first medical contact times for 3 patients.
In the confirmed STEMI group, left anterior descending territory culprit lesions were responsible for 39% of presentations, 6% presented in Killip class III to IV, and 123 (96%) underwent an attempt at primary percutaneous coronary intervention. Radial access was used in 72% of the percutaneous coronary interventions, and procedural success was achieved in 94%. The procedural characteristics for all 3 groups are listed in Table 4 .



