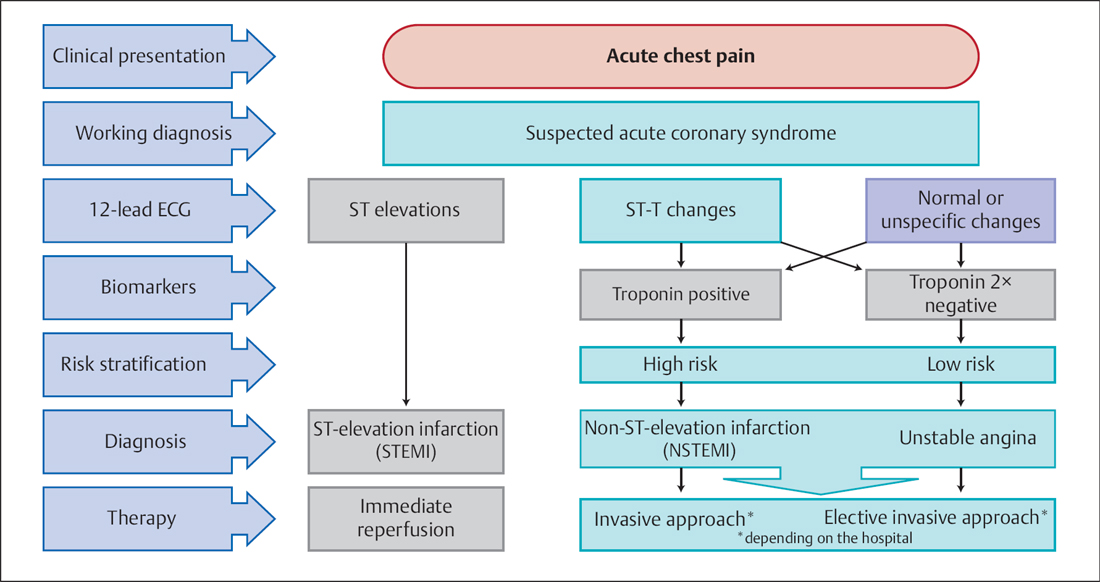
23 Percutaneous Coronary Intervention in Acute Coronary Syndrome Acute coronary syndrome (ACS) is defined as the sudden onset of symptoms and persistent, typical chest pain, with or without transient or persistent ST-segment changes in the ECG. Along with clinical symptoms, the 12-lead ECG and the biomarkers troponin and CK-MB are the basis for the classification of ACS into unstable angina, non–ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). Numerous scores have been developed for risk stratification. The GRACE risk score (http://www.outcomesumassmed.org/grace) has high validity for the assessment of in-hospital and 6-month mortality. The cause of ACS is usually a total or subtotal thrombotic occlusion of a coronary vessel due to a ruptured coronary plaque. Thus, the therapeutic aim for ACS is the rapid, complete, and persistent restoration of coronary perfusion in the affected coronary vessel. The therapy is based upon the following: This chapter will focus on coronary revascularization. Concomitant pharmacological therapy is discussed in more detail in Chapter 30, which deals with peri- and postinterventional antithrombotic therapy for coronary interventions. The indication for an invasive strategy for ACS without ST-segment elevation depends on clinical, biochemical, and ECG findings (Fig. 23.1). – ST-elevations in the 12-lead ECG – Persistent or recurrent angina with or without ST-segment changes – Signs of heart failure or hemodynamic instability – Life-threatening arrhythmias (ventricular tachycardia/ventricular fibrillation) – Increased hs-troponin, increase or decrease of hstroponin – Dynamic ST-segment changes – Diabetes mellitus – Renal insufficiency – Impaired left ventricular function – Early post-infarction angina – Prior myocardial infarction – PCI during the preceding 6 months – Prior CABG – Intermediate or high GRACE risk score (see above) – No recurrent angina – No heart failure – No ECG changes – No biomarker increase (hs-troponin, CK-MB) Two options are available for achieving complete coronary reperfusion: interventional therapy and thrombolysis. The advantage of thrombolysis is that it can be administered anywhere, even pre-hospitalization. The major disadvantages are the following: Mechanical recanalization of the infarct artery by PCI compensates for these disadvantages. Three therapeutic approaches are differentiated: Primary PCI is the therapy of choice in ACS. The method has the following advantages: Primary PCI is the treatment of choice in all patients with acute myocardial infarction if it can be initiated within 90 minutes after the first medical contact and if an experienced team at a dedicated center is available. This requires that a team be available 24 hours a day, every day. To stay within the 90-minute time window and thus offer primary PCI to as many patients with acute myocardial infarction as possible, it is necessary to organize in regional provider networks. The need for primary PCI is uncontroversial in patients with cardiogenic shock and in patients with contraindications for thrombolysis. In our center, primary PCI is generally done in all patients with acute myocardial infarction and symptom onset in < 24 hours or if symptoms persist after 24 hours. The rapid preparation and performance (Fig. 23.2
 A normal ECG does not exclude an acute coronary syndrome.
A normal ECG does not exclude an acute coronary syndrome.
 The diagnosis of NSTEMI is not exclusively based on a positive troponin test but has to be made in light of the clinical setting (chronic kidney disease, sepsis, and so on) and troponin kinetics.
The diagnosis of NSTEMI is not exclusively based on a positive troponin test but has to be made in light of the clinical setting (chronic kidney disease, sepsis, and so on) and troponin kinetics.
 Anti-ischemic drugs (β-blocker, nitrates)
Anti-ischemic drugs (β-blocker, nitrates)
 Anticoagulants (heparin, low-molecular-weight heparin, direct thrombin inhibitors, fondaparinux)
Anticoagulants (heparin, low-molecular-weight heparin, direct thrombin inhibitors, fondaparinux)
 Antiplatelet therapy (aspirin, prasugrel, ticagrelor, clopidogrel, GP IIb/IIIa inhibitors)
Antiplatelet therapy (aspirin, prasugrel, ticagrelor, clopidogrel, GP IIb/IIIa inhibitors)
 Coronary revascularization (intervention (fibrinolysis))
Coronary revascularization (intervention (fibrinolysis))
 Long-term management
Long-term management
Acute Coronary Syndrome without ST-segment Elevation
 Emergency invasive approach:
Emergency invasive approach:
 Early invasive approach (< 72 hours)
Early invasive approach (< 72 hours)
 Elective or noninvasive approach
Elective or noninvasive approach
Acute Coronary Syndrome with ST-segment Elevation
 The method is only indicated for STEMI.
The method is only indicated for STEMI.
 It is only indicated if interventional revascularization is not possible within 90 minutes after the initial contact with medical personnel.
It is only indicated if interventional revascularization is not possible within 90 minutes after the initial contact with medical personnel.
 Depending on the plasminogen activator, the primary reperfusion of the infarct vessel succeeds in only ~50 to 85 % of cases.
Depending on the plasminogen activator, the primary reperfusion of the infarct vessel succeeds in only ~50 to 85 % of cases.
 Successful reperfusion does not mean TIMI 3 flow, which is only achieved in 55 % of patients.
Successful reperfusion does not mean TIMI 3 flow, which is only achieved in 55 % of patients.
 The reocclusion rate is high.
The reocclusion rate is high.
 Time between initiation of thrombolysis and successful reperfusion is 45 to 90 minutes.
Time between initiation of thrombolysis and successful reperfusion is 45 to 90 minutes.
 There is currently no noninvasive clinical method that can assess early and accurately the success or failure of thrombolysis.
There is currently no noninvasive clinical method that can assess early and accurately the success or failure of thrombolysis.
 0.5 to 1.5 % of patients have an intracranial hemorrhage.
0.5 to 1.5 % of patients have an intracranial hemorrhage.
 Only within the first 2 hours after symptom onset does thrombolysis have a reperfusion rate similar to that of PCI.
Only within the first 2 hours after symptom onset does thrombolysis have a reperfusion rate similar to that of PCI.
 Due to the numerous contraindications, thrombolysis is only performed in 25 % of patients with acute infarction.
Due to the numerous contraindications, thrombolysis is only performed in 25 % of patients with acute infarction.
 Primary PCI: PCI without prior thrombolysis for the sole mechanical reperfusion of the infarct vessel
Primary PCI: PCI without prior thrombolysis for the sole mechanical reperfusion of the infarct vessel
 Rescue PCI: PCI after failed thrombolysis with ongoing infarction
Rescue PCI: PCI after failed thrombolysis with ongoing infarction
 “Facilitated” PCI: PCI immediately after lysis to remove the residual stenosis in the infarct vessel independently of the thrombolysis result
“Facilitated” PCI: PCI immediately after lysis to remove the residual stenosis in the infarct vessel independently of the thrombolysis result
Primary PCI
 Rapid and confirmed restoration of TIMI 3 flow in the infarct vessel in > 90 % of patients with simultaneous removal of the underlying stenosis
Rapid and confirmed restoration of TIMI 3 flow in the infarct vessel in > 90 % of patients with simultaneous removal of the underlying stenosis
 The possibility of reperfusion therapy in patients with contraindications for thrombolysis
The possibility of reperfusion therapy in patients with contraindications for thrombolysis
 Immediate knowledge of the coronary status and ventricular function, so that individualized risk stratification is possible
Immediate knowledge of the coronary status and ventricular function, so that individualized risk stratification is possible
 Secure arterial access for additional postinterventional procedures such as intra-aortic counterpulsation or other pump systems
Secure arterial access for additional postinterventional procedures such as intra-aortic counterpulsation or other pump systems
 Indication
Indication
 Procedure
Procedure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree