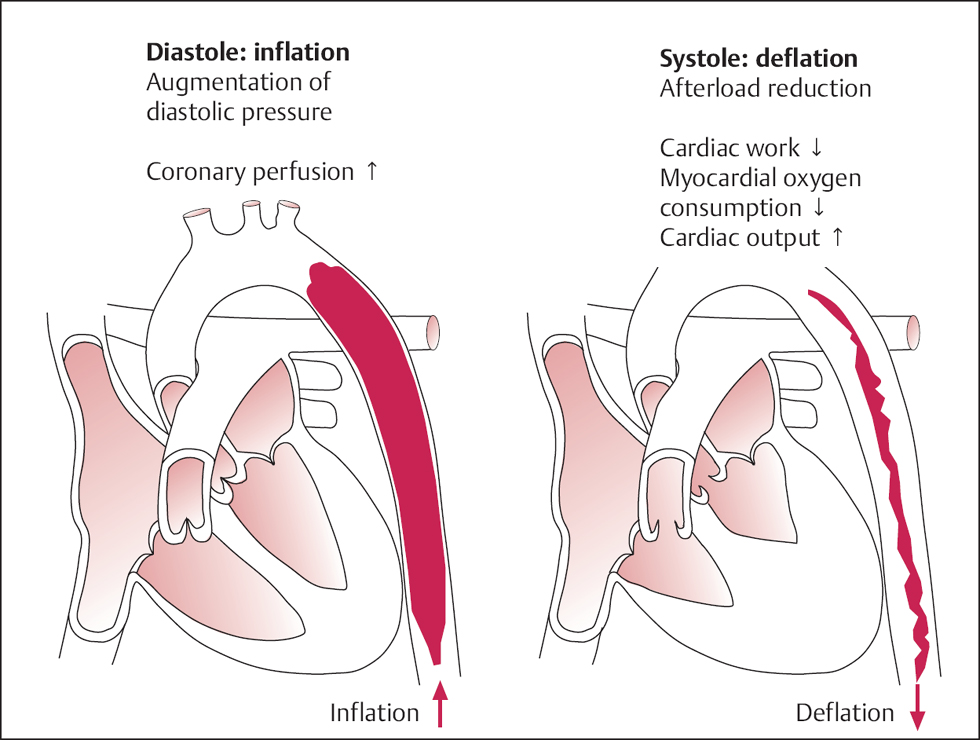
30 Percutaneous Cardiac Support Systems Percutaneous circulatory support systems play an established role in the peri- and postprocedural therapy of high-risk cardiac patients. Pump-driven systems can be differentiated from the intra-aortic balloon pump: for the intra-aortic balloon pump to be efficacious, the cardiac index generated by the patient must be sufficient, whereas for pump-driven systems the pump itself actively transports blood. The major indications for the systems are Systems for complete cardiopulmonary support including oxygenation will not be discussed. The more complex active pump systems result in more powerful hemodynamic unloading and thus symptomatic improvement in the patient. However, they are also associated with a higher rate of complications. Personal view We believe it is important that an intra-aortic balloon pump is available in all hospitals that treat patients with acute cardiac diseases. The pump systems that actively unload the heart should be reserved for centers with appropriate experience in interventional and intensive care. The intra-aortic balloon pump (IABP) is a mechanical circulatory support system for hemodynamic stabilization of patients in cardiogenic shock. The system consists of a polyurethane balloon catheter, which is positioned in the descending thoracic aorta, and an extracorporeal pump with control unit. The pump rapidly fills the balloon with helium in diastole and before the beginning of systole completely empties it again (intra-aortic counter-pulsation). As a consequence, the diastolic aortic pressure is augmented by the balloon. In contrast, the rapid run-off of the blood when the balloon is emptied just before systole decreases the effective aortic blood volumes, with reduction in the systolic aortic pressure and thus left ventricular afterload (Fig. 30.1). Intra-aortic counterpulsation has the following effects: – Increase in coronary perfusion pressure – Increased perfusion of other organs: brain, kidney, etc. – Decreased cardiac work – Reduction in myocardial oxygen consumption – Increased cardiac output The intra-aortic pressure can be measured via the catheter tip while the IABP is in action. For that purpose balloons with fiberoptic pressure recording or with conventional pressure measurement are available. The balloons are available in different volumes (30, 34, or 40 mL), the use of which depends on the patient’s sex, body surface area, and putative aortic diameter. Depending on the manufacturer, the diameter of the nonexpanded balloon is 7F, 7.5F, or 8F. Indications: – Ventricular septal rupture: reduction of the shunt volume by decreasing afterload – Severe acute mitral regurgitation due to papillary muscle rupture: reduction of the regurgitant fraction by decreasing afterload IABP should only be used in patients if the severe left ventricular dysfunction is presumed transient (example: stunned myocardium) or if the cause of the shock can be treated in the short term (examples: severe ischemia, ventricular septal rupture, transplantation). Thus, there is no indication for IABP in patients with end-stage heart failure or terminal, inoperable CAD. Other contraindications are The IABP in cardiology is used exclusively in the critically sick patient, usually under emergency conditions. In our center, IABPs are used most frequently in patients with cardiogenic shock due to acute myocardial infarction. With persistent shock after PCI of the infarct vessel, the IABP is placed during or immediately after completion of the intervention and while the patient is still in the catheterization laboratory. Thus, vessel access via the femoral artery has already been established and fluoroscopy allows immediate verification of the position of the catheter. In contrast, placement of the IABP in the intensive care unit/cardiac care unit is usually done at the bedside and without fluoroscopy.
 Cardiogenic shock of various origins
Cardiogenic shock of various origins
 High-risk interventions
High-risk interventions
Intra-aortic Balloon Pump
 Basics
Basics
 Augmentation of the diastolic aortic pressure with
Augmentation of the diastolic aortic pressure with
 Afterload reduction with
Afterload reduction with
 For an IABP to be of benefit, the stroke volume has to be above a certain threshold. The cardiac index should be at least 1.2 to 1.4 L/m2, the mean arterial pressure should be > 40 mm Hg.
For an IABP to be of benefit, the stroke volume has to be above a certain threshold. The cardiac index should be at least 1.2 to 1.4 L/m2, the mean arterial pressure should be > 40 mm Hg.
 Tachyarrhythmias can significantly impair augmentation or even completely abolish it.
Tachyarrhythmias can significantly impair augmentation or even completely abolish it.
 Indications and Contraindications
Indications and Contraindications
 Cardiogenic shock in acute myocardial infarction
Cardiogenic shock in acute myocardial infarction
 Mechanical complications of acute myocardial infarction with shock:
Mechanical complications of acute myocardial infarction with shock:
 Severe, refractory myocardial ischemia with multivessel disease or main stem stenosis (bridging until CABG)
Severe, refractory myocardial ischemia with multivessel disease or main stem stenosis (bridging until CABG)
 High-risk percutaneous coronary intervention (PCI) during shock
High-risk percutaneous coronary intervention (PCI) during shock
 Elective high-risk PCI with prophylactic IABP insertion
Elective high-risk PCI with prophylactic IABP insertion
 Weaning from cardiopulmonary bypass
Weaning from cardiopulmonary bypass
 Bridging to cardiac transplant
Bridging to cardiac transplant
 Significant aortic regurgitation (increase in regurgitant volumes by diastolic augmentation)
Significant aortic regurgitation (increase in regurgitant volumes by diastolic augmentation)
 Abdominal aortic aneurysm
Abdominal aortic aneurysm
 Aortic dissection
Aortic dissection
 Severe peripheral arterial disease of the pelvis and the lower extremity
Severe peripheral arterial disease of the pelvis and the lower extremity
 Technique
Technique
 Instruments
Instruments
 Extra-stiff guidewire with J-tip (length 150 cm)
Extra-stiff guidewire with J-tip (length 150 cm)
 Dilator
Dilator
 If required 7F or 8F sheath
If required 7F or 8F sheath
 60-mL syringe
60-mL syringe
 Balloon catheter (30-, 34-, 40-mL balloon, depending on putative aortic diameter)
Balloon catheter (30-, 34-, 40-mL balloon, depending on putative aortic diameter)
 Extension tubing
Extension tubing
 Control unit with pump and helium gas bottle
Control unit with pump and helium gas bottle
 Procedure
Procedure
Insertion of the balloon catheter
 Selection and preparation (removal of air with the 60-mL syringe with attached one-way valve) of the balloon catheter
Selection and preparation (removal of air with the 60-mL syringe with attached one-way valve) of the balloon catheter
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree